Abstract
Bleeding in non-steroidal anti-inflammatory drug (NSAID) users limited their prescription. This first multicenter full case–control study (325 cases and 744 controls), explored the association of e-NOS intron 4 variable number tandem repeat (VNTR) polymorphism with upper gastrointestinal hemorrhage (UGIH) in NSAID exposed and unexposed populations and assessed any interaction between this polymorphism and NSAIDs. NSAID users carrying e-NOS intron 4 wild type genotype or VNTR polymorphism have higher odds of UGIH than those unexposed to NSAIDs [Odds Ratio (OR): 6.62 (95% Confidence Interval (CI): 4.24, 10.36) and OR: 5.41 (95% CI 2.62, 11.51), respectively], with no effect modification from VNTR polymorphism-NSAIDs interaction [Relative Excess Risk due to Interaction (RERI): −1.35 (95% CI −5.73, 3.03); Synergism Index (S): 0.77 (95% CI 0.31, 1.94)]. Similar findings were obtained for aspirin exposure. Non-aspirin NSAID users who carry e-NOS intron 4 VNTR polymorphism have lower odds of UGIH [OR: 4.02 (95% CI 1.85, 8.75) than those users with wild type genotype [OR: 6.52 (95% CI 4.09, 10.38)]; though the interaction estimates are not statistically significant [RERI: −2.68 (95% CI −6.67, 1.31); S: 0.53 (95% CI 0.18, 1.55)]. This exploratory study suggests that the odds of UGIH in NSAID or aspirin users does not modify according to patient´s e-NOS intron 4 genotype.
Similar content being viewed by others
Introduction
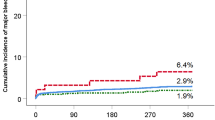
Aspirin and non-aspirin non-steroidal anti-inflammatory drugs (NSAIDs) are among the most frequently used therapeutic agents for a wide variety of indications due to their effectiveness and cost-efficiency1,2,3. The use of aspirin, an archetype of NSAIDs, in secondary prevention against cardiovascular diseases is well established4. Recent reports also demonstrated that the beneficial effects of NSAIDs and aspirin extend to a reduced risk of other major diseases including digestive tract cancers, hepatocellular carcinoma, cholangiocarcinoma, breast cancer, pancreatitis and liver fibrosis5,6,7,8,9,10. However, the idiosyncratic effects manifested by susceptible individuals, mainly gastrointestinal bleeding, have limited the application of NSAIDs and aspirin in primary prevention11,12,13. Gastrointestinal bleeding remains a major medical concern as it is among the main causes of hospitalizations related to digestive diseases in several countries14. Non-variceal upper gastrointestinal hemorrhage (UGIH) represents a serious medical challenge worldwide, with an incidence of 48 to 160 cases per 100,000 adults per year and a mortality rate ranging between 1.1% and 11%15.
Nonetheless, a general discontinuation of NSAIDs or aspirin use might not be a sufficient solution. A recent cohort study of low-dose aspirin for primary or secondary prevention against cardiovascular diseases showed that the cessation of aspirin therapy in patients free from major surgery or bleeding increases the risk of cardiovascular events by more than 30%16. Accordingly, a combination of pharmacogenetic and pharmacoepidemiologic studies is needed to assess and improve the use of personalized NSAIDs treatment.
Gastrointestinal bleeding in patients who use NSAIDs and aspirin was associated with genetic polymorphisms17,18,19,20,21,22. In the gastrointestinal tract, vasodilation and mucosal blood flow are mediated by Nitric Oxide (NO). Prostaglandins also exert a fundamental role in protecting the gastric mucosa from damage23. Circulating NO is mainly produced by endothelial NO synthase (e-NOS) and plays a fundamental role in protecting the gastric mucosa, repairing gastric damage induced by NSAIDs and aspirin, regulating blood flow, fostering angiogenesis, preventing thrombosis, cardiac or vascular contractility, controlling cardiovascular tissue remodeling, and inhibiting platelet aggregation24,25,26,27. Reduced bioavailability of NO predisposes to hypertension, thrombosis and vasospasm28.
Genetic variations in e-NOS influence the expression of this gene, and thus could modify drug response and influence the development of some diseases24,26,29. In specific, the levels of NO in the plasma are significantly affected by genetic variations in intron 4 of e-NOS gene30. The 27-base pairs (bp) variable number of tandem repeat (VNTR) polymorphism in this intron represents a type of these genetic variations. VNTRs are sequences of DNA with a high degree of polymorphism among individuals in the length of repeated nucleotides that lie adjacent to each other in the genome31. The ancestral allele of e-NOS intron 4 VNTR polymorphism consists of five repeats of the 27 bp segment and is known as “4b”, whereas its variant comprises a tandem of four repeats of the 27 bp sequence and is denoted “4a”24,30.
The allele 4a was previously associated with a lower risk of UGIH in aspirin users32. Nonetheless, the protective effect of this e-NOS genetic variant against UGIH was determined in a study that included a selective group of patients exposed to aspirin32. The lack of data about individuals unexposed to aspirin in that study32, makes it impossible to determine whether the reported reduced risk of UGIH is due to a protective effect of 4a e-NOS allele itself or generated from a modification of effect from an interaction between this genetic variation and aspirin, in which case, further investigation is needed.
Accordingly, in this study, we aimed to explore the association of e-NOS intron 4 VNTR polymorphism with UGIH in a population composed of patients exposed and unexposed to NSAIDs. In addition, we investigated the effect modification by 4a and 4b alleles on NSAIDs-related UGIH. We also performed a stratified analysis by type of NSAIDs (i.e. any NSAIDs, aspirin NSAIDs and non-aspirin NSAIDs).
2. Methods.
Study design and population
We carried out a multicenter, full case–control study. Three hundred twenty-five cases and 744 controls were prospectively recruited (incident cases) from four health centers in Spain in two different waves (2004–2007, and 2013–2015).
Cases were defined as patients admitted to the hospital for UGIH, diagnosed surgically or endoscopically. All eligible UGIH cases of any grade of severity were included.
Controls were patients who had a programmed unpainful surgery (such as prostatic adenoma, eye cataract, ear pinning, lipoma, vocal cord cyst, septoplasty and thyroid nodules) that was not related to NSAID exposure.
Adults (> 18 years old), of European origin, and biologically unrelated cases and controls were recruited from the same health centers. We used the native tongue of the participants or the original language of their parents as a proxy of ethnicity33,34,35,36.
Cases and controls were matched on age, sex, recruiting health center and period of recruitment. We used the same protocol as that of two related studies published previously21,37.
Participants were interviewed by trained health personnel using a comprehensive questionnaire that was specifically designed for this study. The questionnaire included questions about the consumed medicines, source of prescriptions and indications of use, recurrent symptoms for which NSAIDs were recommended and the prescribed treatments to alleviate these symptoms. It also included questions about caffeine consumption, dietary habits, alcohol intake and tobacco smoking. Prompt cards of commercial NSAIDs (aspirin and non-aspirin NSAIDs) boxes were used to help the participant identify and recall better the use of these drugs. All NSAIDs were considered for the analysis, irrespective of their route of administration. The interview was repeated on subsequent dates when needed, such as in case of the patient’s tiredness to complete the whole interview and/or failure to remember some information.
The reliability of the interview was rated using a 0–10 Likert scale as perceived by the interviewer. To confirm that NSAID exposure took place prior to any symptom of UGIH, an index date of NSAID use was defined. For cases, the index date was the day of occurrence of the first symptoms of UGIH, whereas it was the recruitment date for the controls. We determined the index date by relying on the patient’s clinical history, but the researchers were blind to patient’s exposure to NSAIDs. In line with previous related studies, a seven-day etiologic window was established starting from the index date38,39,40.
All participants were tested for the presence of anti-Helicobacter pylori immunoglobulin G using enzyme linked immunosorbent assay (ELISA). The following commercial kits were applied according to the manufacturer’s protocol [Human Anti-Helicobacter pylori IgG ELISA Kit (ab108736, Abcam, Cambridge, England), and Captia™ H. pylori IgG EIA (ref: 2,346,400, Trinity Biotech Captia, Co. Wicklaw, Ireland)]. Participants were asked whether they have ever been treated against Helicobacter pylori infection in order to avoid having any false positive result from a previous infection.
Genotyping
The eNOS intron 4 VNTR polymorphism was detected by polymerase chain reaction (PCR) using the following primers: 5′-AGGCCCTATGGTAGTGCCTTT-3′ and 5′-TCTCTTAGTGCTGTGGTCAC-3′41,42,43. The reaction mixture (a total volume of 25 µl) contained 2.5 µl of 10 × PCR buffer, including 100 ng of genomic DNA, 1.5 mM MgCl2, 0.2 mM of each dNTP, 500 nmol of each primer and 5 U Taq polymerase. PCR was performed with 35 cycles of 30 s at 94 °C for denaturation, 30 s at 63 °C for annealing, and 1 min at 72 °C for extension, followed by final extension for 5 min at 72 °C. The following fragments were produced: 393 bp band (4 copies of the 27 bp repeat), and 420 bp band (5 copies of the 27 bp repeat). The amplified product was size fractionated by the D1000 Screen Tape assay (Agilent Technologies, CA) on Agilent 4200 TapeStation system according to manufacturer’s recommendations. For quality control, 5% of the samples were selected to repeat PCR and genotyping, and no discrepancies were found. All cases and controls were genotyped using a phenotype-blind process. Hardy–Weinberg equilibrium was tested in the control group (significance threshold: P-value < 0.001), using SNPassoc Library of the R package44, to check for possible bias in the selection of controls45,46.
Statistical analysis
The 27 bp e-NOS intron 4 VNTR polymorphism was genotyped for all participants who were then stratified into four categories according to NSAID exposure (exposed/unexposed) and genotype (wild type/genetic variation). The wild type genotype was denoted “b allele” and defined as five copies of the 27 bp repeats in both alleles (5/5). The genetic variant was denoted “a allele” when characterized by four copies of the 27 bp repeats in both alleles (4/4) or “ab allele” in case of possessing four copies of the 27 bp repeats in one allele and five copies of the same repeat in the second allele (4/5). The group that comprised patients who were “unexposed to NSAIDs and carriers of the wild type genotype” was used as a reference category.
Adjusted Odds Ratios (OR) of UGIH and their 95% Confidence Intervals (CI) were estimated using the generalized linear mixed models for dependent binomial variables. The statistical models were constructed by considering the following four consecutive levels: patient, strata of cases and controls (each case and its matched controls), health center, and period of patients’ recruitment. We used a random-effects model to assess the effect of the period of patients’ recruitment and a nested random-effects model for the strata of cases and controls, and health center. The models were estimated using the lmer function of the lme4 R package47. Initially, in univariate analysis, we explored the effect of potential confounders including age, Body Mass Index (BMI), sex, tobacco smoking, alcohol intake, caffeine consumption, diet, previous history of arthrosis and/or gastrointestinal disorders other than UGIH, Helicobacter pylori infection, source of information (i.e. whether the interview was answered by the patient independently or with the help of a healthcare assistant / direct relatives), number of undertaken interviews, reliability of the interview as perceived by the interviewer, and exposure to medications that are not NSAIDs. Potential confounders were retained in the model if they changed the OR of the main variable by at least 10%, and provided that the Schwartz’s Bayesian Information Criterion was enhanced48,49.
Subsequently, the additive interaction effect between e-NOS intron 4 VNTR polymorphism and NSAIDs on UGIH was determined by calculating the Relative Excess Risk due to Interaction (RERI) and the Synergism Index (S) estimates along with their 95% CI.
We also undertook a stratified analysis by type of NSAIDs where we assessed the effect of e-NOS VNTR polymorphism on UGIH in 1) non-aspirin NSAIDs users, and 2) aspirin NSAIDs users.
Ethical aspects
Participants signed a written informed consent before their enrolment in the study.
Ethics approval
The study was approved by the ethics committee for clinical research of each participating health center: Barcelona (CEIC; protocol number: Es38121226Z), Euskadi (CEIC-E; protocol number: PI2013101), Galicia (CEIC-G; protocol number: 2013/263) and Valladolid (CEIC-VA-ESTE-HCUV; protocol number: PI-14–142). All procedures were performed in accordance with the 1964 Helsinki declaration and comparable ethical standards.
Results
General patients’ characteristics
Three hundred twenty-five cases and 744 controls fulfilled the inclusion criteria and were included in the study. Their demographic and clinical characteristics are presented in Table 1.
Genotyping
The genotyping was successful for all 1069 participants. Table 2 represents the distribution of the wild type and the polymorphic genotypes across cases and controls.
The homozygous genotype (420 bp/420 bp) denoted by “b” allele was the most prevalent in our study population [247 cases (76%) and 550 (73.9%) controls] (Table 2). Accordingly, “b” allele was deemed as the ancestral wild type allele.
Seventy-eight (24%) cases and 194 (26.1%) controls carried genetic variants of e-NOS intron 4 VNTR polymorphism. The controls followed Hardy–Weinberg equilibrium (p-value = 0.025).
Association of e-NOS VNTR polymorphism with UGIH
Table 3 summarizes the association of NSAID, non-aspirin NSAID and aspirin use with UGIH, stratified by e-Nos intron 4 genotype (wild type/genetic variation).
No association was observed between the polymorphic alleles of e-NOS intron 4 VNTR and UGIH in patients unexposed to any NSAID [OR: 1.14 (95% 0.74, 1.74)], non-aspirin NSAIDs [OR: 1.18 (95% 0.78, 1.78)] and aspirin [OR: 1.03 (95% CI 0.70, 1.51)] (Table 3).
Modification of the effect of NSAIDs on UGIH by e-NOS VNTR polymorphism
As shown in Table 3, an association was observed between exposure to any NSAID and UGIH. Nonetheless, no substantial difference in the magnitude of this association was detected between NSAIDs users with e-NOS intron 4 wild type genotype [OR: 6.62 (95% CI 4.24, 10.36)] and those users with e-NOS intron 4 VNTR polymorphism [OR: 5.41 (95% CI 2.62, 11.15)].
Similar findings were obtained for aspirin exposure by individuals carrying the wild type genotype [OR: 5.17 (95% CI 2.11, 12.68)] and by individuals carrying the genetic variants of e-NOS intron 4 [OR: 5.80 (95% CI 1.32, 25.46)] (Table 3).
Regarding exposure to non-aspirin NSAIDs, patients carrying e-NOS intron 4 VNTR polymorphism have lower odds of UGIH than non-aspirin NSAID users with wild type genotype of e-NOS intron 4 [OR: 4.02 (95% CI 1.85–8.75) and OR: 6.52 (95% CI 4.09, 10.38), respectively] (Table 3).
Our exploratory analysis suggests that there is no interaction between e-NOS intron 4 VNTR polymorphism and any NSAID on UGIH. We also did not observe an interaction between e-NOS intron 4 VNTR polymorphism and aspirin exposure. However, our findings reveal decreased odds of UGIH from a potential interaction between e-NOS intron 4 VNTR polymorphism and non-aspirin NSAID use, though the interaction estimates were not statistically significant [RERI: −2.68 (95% CI −6.67, 1.31); S: 0.53 (95% CI 0.18, 1.55)].
Discussion
Numerous studies associated the risk of gastrointestinal bleeding with genetic polymorphisms. However, there is a lack of knowledge about the influence of genetic variation on UGIH from NSAID and aspirin exposure. eNOS gene is known to exert fundamental activities in protecting gastric mucosa and repairing NSAIDs/aspirin-caused damage. Nevertheless, there is a shortage of information about the effect of variations in this gene on drug response26. In a recent study on the effect of polymorphisms on aspirin-related UGIH, we suggested that aspirin users who carry the inherited allele of rs1799983 polymorphism of NOS3 gene have lower odds of UGIH21. Therefore, in this multicentre case–control study, we conducted an exploratory analysis of the effect of eNOS intron 4 VNTR polymorphism on UGIH in users and non-users of NSAIDs (any NSAID, non-aspirin and aspirin NSAIDs).
The findings of this study reveal that genetic variants of e-NOS intron 4 VNTR polymorphism might not interact with aspirin and consequently, they might not modify the odds of UGIH in aspirin users. Our results also suggest a potentially decreased odds of UGIH in users of non-aspirin NSAIDs who carry the polymorphic genotype of e-NOS intron 4 VNTR. The interaction between non-aspirin NSAIDs and e-NOS intron 4 VNTR polymorphism was not statistically significant, hence, these secondary findings should be considered exploratory and interpreted with caution until replicated in a larger study. If these findings were confirmed, it would mean that the odds of UGIH in any NSAID users carrying e-NOS intron 4 VNTR polymorphism could be overestimated due to the inclusion of aspirin users. They would also allow better management of non-aspirin NSAID personalized medicine.
At the molecular level, the production of NO, a mediator of various physiological functions in the gastrointestinal tract27, seems to be affected by the genetic variation of 27-bp VNTR of e-NOS intron 4. The microRNA derived from this VNTR polymorphism suppresses e-NOS expression, and in specific the ancestral allele “4b” generates more microRNA and thus inhibits further the production of NO24,50,51. On the contrary, the intake of low-dose aspirin increases NO production by blood vessels and stimulates e-NOS enzymatic activity52. As e-NOS is the main isoform responsible for the regulation of vasodilation in the gastrointestinal system, it is expected that carrying the allelic variant 4a of e-NOS may reduce the risk of gastrointestinal bleeding. However, our exploratory analysis revealed that e-NOS intron 4 VNTR polymorphism is not associated with reduced odds of bleeding in aspirin users. This finding could be influenced by the limited number of individuals with e-NOS intron 4 VNTR polymorphism who were on aspirin treatment in our study. Due to the lack of full-case control studies (i.e., studies that encompass users and non-users of aspirin), we cannot compare our findings with those of other reports. However, it is crucial to highlight that our results differ from that of Piazuelo and colleagues who found an association between the genetic variant “4a” of e-NOS gene and lower odds of UGIH in aspirin users32. The study of Piazuelo involved aspirin users exclusively, and thus the effect of 4a e-NOS allele on aspirin-related UGIH could not be determined53. Accordingly, future larger studies are required to guarantee a comprehensive assessment of the effect of e-NOS intron 4 VNTR polymorphism on UGIH in users of aspirin and NSAIDs.
In general, the use of VNTR polymorphism in NSAID or aspirin personalized medicine has been very limited so far, although the high polymorphic characteristics of VNTR make them very informative in determining the loci for diseases31. Research studies have mainly focused on investigating the effect of SNPs in complex diseases or studying drug responses54. To date, only five studies have examined the association of VNTR polymorphism with aspirin and/or NSAIDs. These studies were carried out in different populations and targeted distinct health conditions, highlighting therefore the need for more research on the influence of VNTR polymorphism on NSAIDs- and aspirin-related UGIH (Table 4).
ALOX5, arachidonate 5-lipoxygenase; eNOS, endothelial nitric oxide synthase; FLAP, 5-lipoxygenase-activating protein; PGIS, prostacyclin synthase; UGIH, upper gastrointestinal haemorrhage.
Though our study is exploratory, it is characterized by various points of strength that might help designing future larger studies. Including both groups of participants “exposed and unexposed to NSAIDs” and stratifying by the type of NSAIDs (i.e., aspirin and non-aspirin) permitted providing a comprehensive assessment of these drugs. Adjusting the measures of effect for a large number of potentially confounding factors decreased the risk of confounding in these estimates59. Limiting the analysis to a specific ethnic group (i.e., using the native tongue of the participant or the original mother/father language as a proxy of ethnicity) allowed avoiding bias due to ethnic differences. The inclusion of only biologically unrelated participants prevented bias from the over-representation of ancestral alleles60. The use of catalogue of NSAIDs prompt cards during the interview aided the participants to recall and identify better the use of these drugs, and reviewing the medical records of the patients assisted in the reduction of the risk of recall bias.
Our findings need to be confirmed by larger studies and in different populations. Stratifying the study population by drug exposure and genotype resulted in a limited number of UGIH cases and controls in each stratum, especially in aspirin subgroup analysis, which was then reflected in the width of the estimated confidence intervals. The sample size limitation also precluded carrying out the initially planned dose–response analysis. Therefore, our findings correspond to any exposure to NSAIDs/aspirin. Reproducing the study in a larger population would allow for (1) increasing the number of cases and controls per subgroup and consequently improving the statistical power of the observed associations and (2) undertaking further analysis such as evaluating a dose–response relationship. Furthermore, our results cannot be generalized to non-white European populations due to ethnic differences. Replicating the study in different ethnic groups would permit testing the association between e-NOS intron 4 VNTR polymorphism, NSAIDs and UGIH in genetically different populations.
In conclusion, this exploratory study suggests that exposure to NSAIDs or aspirin does not modify the odds of UGIH according to patient’s e-NOS intron 4 genotype. It also suggests that e-NOS intron 4 VNTR polymorphism might reduce the odds of UGIH in non-aspirin NSAID users. More research is needed to understand the pharmacogenetics of NSAIDs, especially aspirin, which possess a large spectrum of protective and prophylactic properties, and more room should be given to VNTR polymorphism in studies oriented towards personalized medicine.
Data availability
The datasets generated and analyzed for this study can be found in the FigShare Repository [https://doi.org/10.6084/m9.figshare.13109663.v1].
References
Thorat, M. A. & Cuzick, J. Prophylactic use of aspirin: systematic review of harms and approaches to mitigation in the general population. Eur J Epidemiol 30, 5–18. https://doi.org/10.1007/s10654-014-9971-7 (2015).
an overview of cardiovascular risks. Meek, I. L., Van de Laar, M. A. & H, E. V. Non-steroidal anti-Inflammatory drugs. Pharmaceuticals 3, 2146–2162. https://doi.org/10.3390/ph3072146 (2010).
Paulose-Ram, R. et al. Prescription and non-prescription analgesic use among the US adult population: results from the third National Health and Nutrition Examination Survey (NHANES III). Pharmacoepidemiol. Drug Saf. 12, 315–326. https://doi.org/10.1002/pds.755 (2003).
Godley, R. W. & Hernandez-Vila, E. Aspirin for primary and secondary prevention of cardiovascular disease. Tex Heart Inst J 43, 318–319. https://doi.org/10.14503/THIJ-16-5807 (2016).
Iqbal, U. et al. Use of anti-platelet agents in the prevention of hepatic fibrosis in patients at risk for chronic liver disease: a systematic review and meta-analysis. Hepatol Int 13, 84–90. https://doi.org/10.1007/s12072-018-9918-2 (2019).
Simon, T. G. et al. Daily Aspirin use associated with reduced risk for fibrosis progression in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 17, 2776–2784 e2774. https://doi.org/10.1016/j.cgh.2019.04.061 (2019).
Jiang, Z. G. et al. Aspirin use is associated with lower indices of liver fibrosis among adults in the United States. Aliment Pharmacol. Ther. 43, 734–743. https://doi.org/10.1111/apt.13515 (2016).
Wang, S. et al. Association of aspirin therapy with risk of hepatocellular carcinoma: A systematic review and dose-response analysis of cohort studies with 2.5 million participants. Pharmacol Res 151, 104585. https://doi.org/10.1016/j.phrs.2019.104585 (2020).
Win, T. T., Aye, S. N., Lau Chui Fern, J. & Ong Fei, C. Aspirin and reducing risk of gastric cancer: systematic review and meta-analysis of the observational studies. J Gastrointestin Liver Dis 29, 191–198.https://doi.org/10.15403/jgld-818 (2020)
Agrawal, A. & Fentiman, I. S. NSAIDs and breast cancer: a possible prevention and treatment strategy. Int. J. Clin. Pract. 62, 444–449. https://doi.org/10.1111/j.1742-1241.2007.01668.x (2008).
Piepoli, M. F. et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Eur Heart J 37, 2315–2381. https://doi.org/10.1093/eurheartj/ehw106 (2016).
American Geriatrics Society Beers Criteria Update Expert, P. American Geriatrics Society. updated beers criteria for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 63(2227–2246), 2015. https://doi.org/10.1111/jgs.13702 (2015).
Arnett, D. K. et al. ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary. 74(1376–1414), 2019. https://doi.org/10.1016/j.jacc.2019.03.009 (2019).
Lanas, A. et al. Non-variceal upper gastrointestinal bleeding. Nat. Rev. Dis. Primers. 4, 18020. https://doi.org/10.1038/nrdp.2018.20 (2018).
Jairath, V., Martel, M., Logan, R. F. & Barkun, A. N. Why do mortality rates for nonvariceal upper gastrointestinal bleeding differ around the world? A systematic review of cohort studies. Can. J. Gastroenterol. 26, 537–543. https://doi.org/10.1155/2012/862905 (2012).
Sundstrom, J. et al. Low-dose Aspirin discontinuation and risk of cardiovascular events: a Swedish nationwide, population-based cohort study. Circulation 136, 1183–1192. https://doi.org/10.1161/CIRCULATIONAHA.117.028321 (2017).
Wu, Y. et al. Study of clinical and genetic risk factors for Aspirin-induced gastric mucosal injury. Chin. Med. J. (Engl.) 129, 174–180. https://doi.org/10.4103/0366-6999.173480 (2016).
Shiotani, A. et al. Single nucleotide polymorphism markers for low-dose aspirin-associated peptic ulcer and ulcer bleeding. J. Gastroenterol. Hepatol. 29(Suppl 4), 47–52. https://doi.org/10.1111/jgh.12770 (2014).
Shiotani, A. et al. Novel single nucleotide polymorphism markers for low dose aspirin-associated small bowel bleeding. PLoS ONE 8, e84244. https://doi.org/10.1371/journal.pone.0084244 (2013).
Cho, J. H. et al. The IL-1B genetic polymorphism is associated with Aspirin-induced peptic ulcers in a Korean Ethnic Group. Gut Liver 10, 362–368. https://doi.org/10.5009/gnl15129 (2016).
Mallah, N. et al. Influence of polymorphisms involved in platelet activation and inflammatory response on Aspirin-related upper gastrointestinal bleeding: A case-control study. Front. Pharmacol. 11, 860. https://doi.org/10.3389/fphar.2020.00860 (2020).
Agundez, J. A., Garcia-Martin, E. & Martinez, C. Genetically based impairment in CYP2C8- and CYP2C9-dependent NSAID metabolism as a risk factor for gastrointestinal bleeding: is a combination of pharmacogenomics and metabolomics required to improve personalized medicine?. Expert. Opin. Drug. Metab. Toxicol. 5, 607–620. https://doi.org/10.1517/17425250902970998 (2009).
Whittle, B. J. Role of prostaglandins in the defense of the gastric mucosa. Brain Res. Bull. 5(Suppl 1), 7–14. https://doi.org/10.1016/0361-9230(80)90297-x (1980).
Farah, C., Michel, L. Y. M. & Balligand, J.-L. Nitric oxide signalling in cardiovascular health and disease. Nat. Rev. Cardiol. 15, 292–316. https://doi.org/10.1038/nrcardio.2017.224 (2018).
Gresele, P., Momi, S. & Guglielmini, G. Nitric oxide-enhancing or -releasing agents as antithrombotic drugs. Biochem. Pharmacol. 166, 300–312. https://doi.org/10.1016/j.bcp.2019.05.030 (2019).
Cotta Filho, C. K., Oliveira-Paula, G. H., Rondon Pereira, V. C. & Lacchini, R. Clinically relevant endothelial nitric oxide synthase polymorphisms and their impact on drug response. Expert. Opin. Drug Metab. Toxicol. 1:1–25. https://doi.org/10.1080/17425255.2020.1804857 (2020).
Lanas, A. Role of nitric oxide in the gastrointestinal tract. Arthritis Res Ther 10 Suppl 2, S4. https://doi.org/10.1186/ar2465 (2008).
Naseem, K. M. The role of nitric oxide in cardiovascular diseases. Mol. Aspects Med. 26, 33–65. https://doi.org/10.1016/j.mam.2004.09.003 (2005).
Oliveira-Paula, G. H., Pereira, S. C., Tanus-Santos, J. E. & Lacchini, R. Pharmacogenomics and hypertension: current Insights. Pharmgenom. Pers. Med. 12, 341–359. https://doi.org/10.2147/PGPM.S230201 (2019).
Wang, X. L. et al. Genetic contribution of the endothelial constitutive nitric oxide synthase gene to plasma nitric oxide levels. Arterioscler Thromb. Vasc. Biol. 17, 3147–3153. https://doi.org/10.1161/01.atv.17.11.3147 (1997).
Nakamura, Y., Koyama, K. & Matsushima, M. VNTR (variable number of tandem repeat) sequences as transcriptional, translational, or functional regulators. J. Hum. Genet. 43, 149–152. https://doi.org/10.1007/s100380050059 (1998).
Piazuelo, E., Fuentes, J., Garcia-Gonzalez, M. A., Jimenez, P. & Lanas, A. A case-control study of the association between polymorphisms of the endothelial nitric oxide synthase and glycoprotein IIIa genes and upper gastrointestinal bleeding in users of low-dose aspirin. Clin. Ther. 30, 121–130. https://doi.org/10.1016/j.clinthera.2008.01.020 (2008).
Baker, J. L., Rotimi, C. N. & Shriner, D. Human ancestry correlates with language and reveals that race is not an objective genomic classifier. Sci. Rep. 7, 1572. https://doi.org/10.1038/s41598-017-01837-7 (2017).
Barbujani, G., Whitehead, G. N., Bertorelle, G. & Nasidze, I. S. Testing hypotheses on processes of genetic and linguistic change in the Caucasus. Hum. Biol. 66, 843–864 (1994).
Comission, E. Analysis and comparative review of equality data collection practices in the European Union. Data collection in the field of ethnicity (2020).
Longobardi, G. et al. Across language families: Genome diversity mirrors linguistic variation within Europe. Am. J. Phys. Anthropol. 157, 630–640. https://doi.org/10.1002/ajpa.22758 (2015).
Figueiras, A. et al. CYP2C9 variants as a risk modifier of NSAID-related gastrointestinal bleeding: a case-control study. Pharmacogenet. Genomics 26, 66–73. https://doi.org/10.1097/FPC.0000000000000186 (2016).
Lanas, A. et al. Nitrovasodilators, low-dose aspirin, other nonsteroidal antiinflammatory drugs, and the risk of upper gastrointestinal bleeding. N. Engl. J. Med. 343, 834–839. https://doi.org/10.1056/NEJM200009213431202 (2000).
Laporte, J. R., Carne, X., Vidal, X., Moreno, V. & Juan, J. Upper gastrointestinal bleeding in relation to previous use of analgesics and non-steroidal anti-inflammatory drugs. Catalan Countries Study on Upper Gastrointestinal Bleeding. Lancet 337, 85–89. https://doi.org/10.1016/0140-6736(91)90744-a (1991).
Laporte, J. R., Ibanez, L., Vidal, X., Vendrell, L. & Leone, R. Upper gastrointestinal bleeding associated with the use of NSAIDs: newer versus older agents. Drug Saf. 27, 411–420. https://doi.org/10.2165/00002018-200427060-00005 (2004).
Marroni, A. S. et al. Consistent interethnic differences in the distribution of clinically relevant endothelial nitric oxide synthase genetic polymorphisms. Nitr. Oxide 12, 177–182. https://doi.org/10.1016/j.niox.2005.02.002 (2005).
Tanus-Santos, J. E. et al. Effects of endothelial nitric oxide synthase gene polymorphisms on platelet function, nitric oxide release, and interactions with estradiol. Pharmacogenetics 12, 407–413. https://doi.org/10.1097/00008571-200207000-00008 (2002).
Thameem, F. et al. Endothelial nitric oxide synthase (eNOS) gene polymorphisms and their association with type 2 diabetes-related traits in Mexican Americans. Diab. Vasc. Dis. Res. 5, 109–113. https://doi.org/10.3132/dvdr.2008.018 (2008).
González, J., Moreno, V. SNPassoc: SNPs-Based Whole Genome Association Studies. https://CRAN.R-project.org/package=SNPassoc (2020).
Chen, J. & Chatterjee, N. Exploiting Hardy-Weinberg equilibrium for efficient screening of single SNP associations from case-control studies. Hum. Hered. 63, 196–204. https://doi.org/10.1159/000099996 (2007).
Salanti, G., Amountza, G., Ntzani, E. E. & Ioannidis, J. P. Hardy-Weinberg equilibrium in genetic association studies: an empirical evaluation of reporting, deviations, and power. Eur. J. Hum. Genet. 13, 840–848. https://doi.org/10.1038/sj.ejhg.5201410 (2005).
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting Linear Mixed-Effects Models using lme4. J. Stat. Softw. 67, 1–48. https://doi.org/10.18637/jss.v067.i01 (2015).
Schwarz, G. Estimating the dimension of a model. Ann. Stat. 6, 461–464 (1978).
Mickey, R. M. & Greenland, S. The impact of confounder selection criteria on effect estimation. Am. J. Epidemiol. 129, 125–137. https://doi.org/10.1093/oxfordjournals.aje.a115101 (1989).
Zhang, M. X. et al. Regulation of endothelial nitric oxide synthase by small RNA. Proc. Natl. Acad. Sci. USA 102, 16967–16972. https://doi.org/10.1073/pnas.0503853102 (2005).
Zhang, M. X. et al. Effect of 27nt small RNA on endothelial nitric-oxide synthase expression. Mol. Biol. Cell 19, 3997–4005. https://doi.org/10.1091/mbc.E07-11-1186 (2008).
O’Kane, P. et al. Aspirin acetylates nitric oxide synthase type 3 in platelets thereby increasing its activity. Cardiovasc. Res. 83, 123–130. https://doi.org/10.1093/cvr/cvp120 (2009).
Estany-Gestal, A., Salgado-Barreira, A., Sanchez-Diz, P. & Figueiras, A. Influence of CYP2C9 genetic variants on gastrointestinal bleeding associated with nonsteroidal anti-inflammatory drugs: a systematic critical review. Pharmacogenet. Genomics 21, 357–364. https://doi.org/10.1097/FPC.0b013e328346d2bb (2011).
Brookes, K. J. The VNTR in complex disorders: the forgotten polymorphisms? A functional way forward?. Genomics 101, 273–281. https://doi.org/10.1016/j.ygeno.2013.03.003 (2013).
Kleinstein, S. E. et al. Genetic variation in the lipoxygenase pathway and risk of colorectal neoplasia. Genes Chromosom. Cancer 52, 437–449. https://doi.org/10.1002/gcc.22042 (2013).
Poole, E. M. et al. Prostacyclin synthase and arachidonate 5-lipoxygenase polymorphisms and risk of colorectal polyps. Cancer Epidemiol Biomarkers Prev 15, 502–508. https://doi.org/10.1158/1055-9965.EPI-05-0804 (2006).
Jin, Y. Y., Yu, G. Z., Wang, Y., Cui, L. Y. & Xin, X. M. Variable number of tandem repeats polymorphism of platelet glycoprotein Ib alpha in Chinese people and CC genotype with aspirin sensitivity in patients with cerebral infarction. J Clin Pharm Ther 34, 239–243. https://doi.org/10.1111/j.1365-2710.2008.00992.x (2009).
Cervera, A. et al. The BC genotype of the VNTR polymorphism of platelet glycoprotein Ibalpha is overrepresented in patients with recurrent stroke regardless of aspirin therapy. Cerebrovasc Dis 24, 242–246. https://doi.org/10.1159/000104485 (2007).
Hsu, P. I. & Tsai, T. J. Epidemiology of upper gastrointestinal damage associated with low-dose Aspirin. Curr Pharm Des 21, 5049–5055. https://doi.org/10.2174/1381612821666150915104800 (2015).
Malomane, D. K. et al. Efficiency of different strategies to mitigate ascertainment bias when using SNP panels in diversity studies. BMC Genomics 19, 22. https://doi.org/10.1186/s12864-017-4416-9 (2018).
Acknowledgements
The authors would like to thank the health personnel who helped in recruiting and interviewing the patients and members of the EMPHOGEN project (P. López, P. Sánchez-Diz, A. Ruano, E. Domínguez, A. Estany-Gestal, S. Ortega, A. Carvajal, B. Ruiz, M.M. de Pancorbo, P. Ruiz).
Funding
This work was supported by a grant from Instituto de Salud Carlos III [PI12/02414]/Plan Estatal de I + D + I 2012–2016; Fondo Europeo de Desarrollo Regional (FEDER); the Novartis, Pfizer and Dr Esteve pharmaceutical companies; the Health Research Fund/Fondo de Investigación Sanitaria [PI021512, PI021364, PI020661, PI021572]; Ministry of Health & Consumer Affairs, Spain [SAF2002-04057]; Galician Regional Authority, Spain [PGIDIT03PXIC20806PN]; Department of Health of the Basque Country [03/11092 and 11/111103]; and Fundacion vasca de innovacin e investigacin sanitarias [OSIBG19/002 and OSIBG18/105]. The genotyping service was carried out at CEGEN-PRB3-ISCIII; Instituto de Salud Carlos III and ERDF [PT17/0019, of the PE I + D + I 2013–2016].
Author information
Authors and Affiliations
Contributions
C.A., L.I., X.V., and A.F. conceived the research idea, designed the study, and supervised and administered the project. N.M. carried out the literature review and conceptualized and wrote the manuscript. N.M. and M.P. analyzed the data. A.F. supervised data analysis. N.M. participated in the genetic laboratory testing. M.Z.C., EI-G., I.P.–Z., F.M.G., J.I.G., L.V., L.M.-A., M.S.G., V.V.G. and A.S.B. involved in patients’ recruitment and data registration. All authors contributed to data interpretation, reviewed the earlier version of the manuscript and approved it for submission and agree to be accountable for the content of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mallah, N., Zapata-Cachafeiro, M., Aguirre, C. et al. A multicenter case–control study of the effect of e-nos VNTR polymorphism on upper gastrointestinal hemorrhage in NSAID users. Sci Rep 11, 19923 (2021). https://doi.org/10.1038/s41598-021-99402-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-99402-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.