Abstract
Both the innate and adaptive immune responses are deregulated in individuals with obesity and are key drivers of its associated metabolic alterations. Although the anti-inflammatory growth differentiation factor 15 (GDF-15) is a candidate protein against obesity, its mechanisms regulating the immune responses are not fully cleared. We examined whether GDF-15 was related to serum immunoglobulins in a children’s cohort assessed longitudinally during childhood. Results showed that circulating GDF-15 positively associated with IgA (p < 0.002) and IgG (p < 0.001) levels and the IgA*IgG product (p < 0.001) in apparently healthy children at both baseline (age 9) and follow-up (age 13). The associations were readily observed in heavier children (those with BMI-SDS above the median) as well as in children with higher renal fat accumulation (those with renal fat-to-height ratio above the median) and remained significant after correcting for possible confounding variables. Serum GDF-15 levels accounted for up to 16% of the variance of follow-up IgG levels and up to 14% of the variance of follow-up IgA*IgG product. The longitudinal associations of the anti-inflammatory GDF-15 with IgA, IgG and the IgA*IgG product in children with higher BMI or higher renal fat accumulation suggest a role of GDF-15 in human obesity through the regulation of the immune adaptive system.
Similar content being viewed by others
Introduction
Obesity and its associated metabolic alterations have reached epidemic proportions, also in childhood1. A crucial driver of this process is the chronic low-grade inflammation observed in individuals with obesity. Chronic inflammation is known to have the active participation of innate immune system, including T cell activation and production of immunoglobulins by B lymphocytes infiltrating the visceral adipose tissue2,3. Growth differentiation factor 15 (GDF-15) is a candidate protein in the fight against obesity because of its anti-inflammatory, anorexigenic and lipolytic properties4. Despite the fact that GDF-15 is recognized as a key circulating anti-inflammatory factor, scarce publications in obese children have been reported5 and its mechanisms regulating immune responses are not fully elucidated. IgA and IgG have been related to a poorer metabolic profile in obese children6, and. higher concentrations of IgA and IgG have been reported in obese adults7 and children8, suggesting that there is a relationship between the adaptive immune system and adipose tissue function. We hypothesized that GDF-15 would be associated with components of the immune system in children with obesity.
The aim of this study was to examine whether GDF-15 was related to serum levels of IgA and IgG in a cohort of apparently healthy children assessed longitudinally during childhood both at baseline and at follow-up. Analyses were also performed in groups thereof with higher body mass index (BMI) or renal fat.
Methods
The study population consisted of 204 Caucasian children (101 girls and 103 boys) assessed longitudinally at baseline (8.5 ± 1.8 years) and at follow-up (13.0 ± 1.9 years). Subjects were consecutively recruited among those seen in a primary care setting in Girona, a region in North-eastern Spain, and included in a previously reported children’s cohort9,10. Briefly, inclusion criteria were (1) age between 6 and 10 years; (2) no pubertal development, as judged by a specifically trained nurse using Tanner criteria (breast stage I; testicular volume bilaterally < 4 ml). Exclusion criteria were (1) major congenital anomalies; (2) abnormal blood count, abnormal liver, kidney or thyroid functions; (3) evidence of chronic illness or prolonged use of medication; (4) acute illness or use of medication in the month preceding potential enrolment. The study protocol was approved by the Ethics Review Committee of the Institutional Review Board of Dr. Josep Trueta Hospital and was performed in accordance with their code of ethics, guidelines and regulations. Informed written consent was obtained from the parents.
Clinical examination followed by venous blood sampling in the fasting state was performed in the morning as previously reported9,10. Briefly, weight and height were measured with a calibrated scale and a Harpenden stadiometer, respectively. Body mass index (BMI) was calculated as weight divided by the square of height in meters. Age-adjusted and sex-adjusted standard deviation scores (SDS) for BMI were calculated using regional normative data. Renal fat thickness was assessed by high-resolution ultrasonography using a linear 12-MHz transducer (MyLabTM25, Esaote). Averages of three to five measurements were used in the study. All measurements were performed by the same observer who was unaware of the clinical and laboratory characteristics of the subjects. Intra-subject coefficient of variation for ultrasound measurements was less than 6%. Blood pressure was measured in the supine position on the right arm after a 10-min rest using an electronic sphygmomanometer with cuff size appropriate for children’s arm circumference.
All serum samples were obtained between 8:00 and 9:00 AM under fasting conditions. Fasting serum immunoreactive insulin was assayed as described previously9. Total IgG, IgA and IgM were measured by a commercial nephelometric immunoassay (Immage Immunochemistry Systems; Beckman Coulter). The intra-assay CVs were 2.0–2.6%, 2.5–2.9% and 2.4–3.2%, respectively. GDF-15 was measured by an ELISA (Human GDF-15 DuoSet ELISA, R&D Systems). The sensitivity was 7 pg/ml and intra-assay CVs were less than 8%. Serum samples were kept frozen at -80 °C until assay. Follow-up data were obtained 4 years after the baseline visit and the same anthropometric, clinical and laboratory variables (except for GDF-15) were assessed following the same methodology.
Statistical analyses were performed using SPSS version 22.0 (SPSS Inc.). Results are expressed as mean ± standard deviation (SD). Logarithmic transformation was used to obtain normally distributed values for GDF-15 and immunoglobulins. Differences across groups defined by the median of BMI-SDS or the median of renal fat-to-height ratio were examined by independent T-test (continuous data) and by Chi square (categorical data). The relation between variables was analyzed by Pearson bivariate correlations followed by multivariate linear regression analyses. The enter method was used for computing the independent variables and the step-wise method was used for additionally computing individual R2 values. Significance level was set at p < 0.05.
Results
The total studied population comprised 204 apparently healthy children with a mean BMI-SDS of 0.62 ± 1.40. Circulating baseline GDF-15 levels ranged from 35 to 221 pg/ml (Table 1). Subjects were split into subgroups according to the median value of baseline BMI-SDS (Supplementary Table S1) and according to the median value of baseline renal fat-to-height ratio (as a proxy of visceral fat accumulation; Table 1). Differences between subgroups according to renal fat-to-height ratio were seen in almost all anthropometric parameters being analyzed such as weight, height, BMI and renal fat (Table 1).
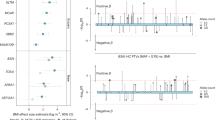
Bivariate correlations showed that GDF-15 was positively associated at baseline with IgG levels and with the IgA*IgG product in all studied subjects (mean age 9 years; all p < 0.05; data not shown). Moreover, when analyzing the subgroups defined by the median of BMI-SDS or the median of renal fat-to-height ratio, children with higher BMI-SDS (data not shown) and especially those with higher renal fat-to-height showed positive correlations between circulating GDF-15 and IgA (p = 0.004), IgG (p = 0.001) levels and the IgA*IgG product (p < 0.001; Fig. 1a).
Follow-up data at a mean age of 13 years showed that baseline GDF-15 was also positively associated with follow-up IgA and IgG levels as well as the IgA*IgG product, when analyzing all subjects or those children with BMI-SDS above the median (all p < 0.05; data not shown), but especially when analyzing those children with renal fat-to-height ratio above the median (all p < 0.002; Fig. 1b).
Finally, multivariate regression analyses assessed on the previously observed correlations showed that circulating GDF-15 remained independently associated with IgA, IgG and the IgA*IgG product in children with BMI-SDS or renal fat-to-height ratio above the median at baseline, after correcting for possible confounding variables such as age, sex and BMI (Supplementary Table S2). In these models, baseline GDF-15 levels accounted for up to 10% of the variance of IgG levels and up to 6% of the variance of the IgA*IgG product.
At follow-up, baseline GDF-15 remained also independently associated with follow-up IgA, IgG and the IgA*IgG product in children with BMI-SDS or renal fat-to-height ratio above the median, after correcting for the same confounding variables (Supplementary Table S2). In these models, baseline GDF-15 explained up to 16% of the variance of follow-up IgG levels and up to 14% of the variance of the follow-up IgA*IgG product.
Discussion
The main result of the study is that GDF-15 associates positively and longitudinally with IgA, IgG and IgA*IgG product in children with higher BMI or higher renal fat accumulation.
As previously reported by our group and others, IgA and IgG are upregulated in obesity7,8 and related to a poorer metabolic profile in children6. Hence, immunoglobulins such as IgA and IgG seem to be closely related to the altered metabolic status in obesity. Although immunoglobulins present functional diversification, IgG is often described as pathogenic11 and IgA has been demonstrated to be an inducer of inflammation12.
B lymphocytes, which secrete IgA and IgG antibodies, have been shown to be among the first cells to be recruited into visceral adipose tissue, followed by recruitment of T cells3, which in turn could dictate the extent of the local inflammatory response through macrophage modulation and secretion of pro-inflammatory cytokines13. GDF-15 is known to be secreted as an adipokine14, and similarly to other adipokines may regulate the innate and adaptive immune response15. Along the same line, GDF-15 was shown to inhibit T cell stimulation and reduce dendritic cell maturation markers in dendritic cell cultures16. Others have shown that GDF15 is up-regulated as a physiological counter-regulatory mechanism in disorders associated with cell stress17. Finally, a relationship between GDF-15 and immunoglobulins has been also found, for example, in subjects with IgG4-related disease18 or patients with IgA nephropathy19.
Taking into account our results and the previous literature discussed above it is plausible to speculate that the anti-inflammatory GDF-15 could regulate the adaptive immunity by means of counteracting the pro-inflammatory effects of IgA and IgG and thus reducing the obesity-related low-grade inflammation state.
We acknowledge some limitations of our study such as not observing any direct associations between GDF-15 and obesity parameters, for instance, BMI or renal fat in our studied children. One explanation might be that in our study, children were overall healthy. It has been suggested that a threshold degree of obesity is necessary to elicit an adaptive immune system response in adipose tissue20. Accordingly, GDF-15 correlations with IgA and IgG were significant in heavier children (those with BMI-SDS above the median) and in children with higher accumulation of renal fat (those with renal fat-to-height above the median), which give support to a possible role of GDF-15 in obesity-triggered inflammation. Among the strengths of our study is the longitudinal independent associations between GFD-15, IgA, IgG and the IgA*IgG, suggesting a causal role of GFD-15 in the regulation of adaptive immunity.
In conclusion, serum GDF-15 associates positively and longitudinally with IgA, IgG and the IgA*IgG product in children with higher BMI or higher renal fat accumulation. Our results suggest that GDF-15 could exert its known anti-inflammatory activity by regulating at least in part the adaptive immunity, especially in heavier subjects or in those with more visceral fat accumulation. Further research studies may help disclose whether GDF-15 treatment can limit the pro-inflammatory effects of IgA and IgG in obesity.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Garrido-Miguel, M. et al. Prevalence and trends of overweight and obesity in European children from 1999 to 2016: A systematic review and meta-analysis. JAMA Pediatr. 173(10), e192430 (2019).
Winer, D. A., Winer, S., Chng, M. H. Y., Shen, L. & Engleman, E. G. B Lymphocytes in obesity-related adipose tissue inflammation and insulin resistance. Cell. Mol. Life Sci. 71(6), 1033–1043 (2014).
Zhu, F., Wang, A., Li, Y., Liang, R., Li, D., & Li, B. Adipose tissue-resident regulatory T cells. In Advances in Experimental Medicine and Biology, vol. 1011, 153–162 (Springer, 2017).
Wischhusen, J., Melero, I. & Fridman, W. H. Growth/differentiation factor-15 (GDF-15): From biomarker to novel targetable immune checkpoint. Front. Immunol. 11, 951 (2020).
Yuca, S. A. et al. The relationship between metabolic parameters, cardiac parameters and MIC-1/GDF15 in obese children. Exp. Clin. Endocrinol. Diabetes 125(2), 86–90 (2017).
Bassols, J. et al. Increased serum IgG and IgA in overweight children relate to a less favourable metabolic phenotype. Pediatr. Obes. 9(3), 232–238 (2014).
Gonzalez-Quintela, A. et al. Serum levels of immunoglobulins (IgG, IgA, IgM) in a general adult population and their relationship with alcohol consumption, smoking and common metabolic abnormalities. Clin. Exp. Immunol. 151(1), 42–50 (2008).
Okamatsu, Y. et al. Ghrelin and leptin modulate immunity and liver function in overweight children. Pediatr. Int. 51(1), 9–13 (2009).
Prats-Puig, A. et al. Balanced duo of anti-inflammatory SFRP5 and proinflammatory WNT5A in children. Pediatr. Res. 75(6), 793–797 (2014).
Prats-Puig, A. et al. α-Defensins and bacterial/permeability-increasing protein as new markers of childhood obesity. Pediatr. Obes. 12(2), e10 (2017).
Wang, T. T. & Ravetch, J. V. Functional diversification of IgGs through Fc glycosylation. J. Clin. Investig. 129(9), 3492–3498 (2019).
Hansen, I. S., Baeten, D. L. P. & den Dunnen, J. The inflammatory function of human IgA. Cell. Mol. Life Sci. 76(6), 1041–1055 (2019).
Winer, S. & Winer, D. A. The adaptive immune system as a fundamental regulator of adipose tissue inflammation and insulin resistance. Immunol. Cell Biol. 90(8), 755–762 (2012).
Ding, Q. et al. Identification of macrophage inhibitory cytokine-1 in adipose tissue and its secretion as an adipokine by human adipocytes. Endocrinology 150(4), 1688–1696 (2009).
Umano, G. R. et al. Pediatric Obesity And The Immune System. Front. Pediatr. 7, 487 (2019).
Zhou, Z. et al. Growth differentiation factor-15 suppresses maturation and function of dendritic cells and inhibits tumor-specific immune response. PLoS ONE 8(11), e78618 (2013).
Tsai, V. W. W., Husaini, Y., Sainsbury, A., Brown, D. A. & Breit, S. N. The MIC-1/GDF15-GFRAL pathway in energy homeostasis: Implications for obesity, cachexia, and other associated diseases. Cell Metab. 28(3), 353–368 (2018).
Kawashiri, S. Y. et al. Association of serum levels of fibrosis-related biomarkers with disease activity in patients with IgG4-related disease. Arthritis Res. Ther. 20(1), 1–8 (2018).
Na, K. R. et al. Growth differentiation factor 15 as a predictor of adverse renal outcomes in patients with immunoglobulin A nephropathy. Intern. Med. J. 47(12), 1393–1399 (2017).
Artemniak-Wojtowicz, D., Pyrżak, B. & Kucharska, A. M. Obesity and chronic inflammation crosslinking. Cent. Eur. J. Immunol. 45(4), 461–468 (2020).
Acknowledgements
The authors are grateful to all the children and parents who participated in the study.
Funding
The study was supported by Grant Nos. PI16/01335 and PI19/00451 (to A.L.-B.) and PI17/00557 (to J.B.) from the National Institute of Health Carlos III (Fund for Health Research FIS, Spain), projects co-financed by Fondo Europeo de Desarrollo Regional (FEDER). GC-B holds a Sara Borrell fellowship from the National Institute of Health Carlos III (CD19-00172).
Author information
Authors and Affiliations
Contributions
G.C.-B. contributed to the conception of the study and its design, carried out experiments, performed data analysis and wrote the first draft of the manuscript. A.G.-V., B.M.-P., A.P.-P., S.X.-T. and E.P.-C. contributed to data collection and reviewed the manuscript. F.d.Z., L.I. and J.B. reviewed the manuscript. A.L.-B. conceived the study and contributed to writing the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Carreras-Badosa, G., Gómez-Vilarrubla, A., Mas-Parés, B. et al. Longitudinal association of the anti-inflammatory serum marker GDF-15 with serum IgA and IgG in apparently healthy children. Sci Rep 11, 18215 (2021). https://doi.org/10.1038/s41598-021-97386-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-97386-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.