Abstract
Pediatric extrapulmonary tuberculosis (EPTB) is a diagnostic challenge. A new immunochemistry based MPT64 antigen detection test has shown improved sensitivity compared to current laboratory tests. The aim of this study was to implement and validate the test performance in a resource limited African setting. Presumptive pediatric (0–18 y) EPTB patients were prospectively enrolled at Mbeya Zonal Referral Hospital, and followed to the end of treatment or until a final diagnosis was reached. Specimens from suspected sites of infection were subject to routine diagnostics, GeneXpert MTB/RIF assay and the MPT64 test. The performance of the tests was assessed using mycobacterial culture as well as a composite reference standard. 30 patients were categorized as TB cases, 31 as non-TB cases and 2 were uncategorized. In the TB group, the three most common infections were adenitis (30%), peritonitis (30%) and meningitis (20%). The sensitivity, specificity, positive predictive value, negative predictive value and accuracy of the MPT64 test was 92%, 88%, 87%, 92% and 90%, respectively. Mortality was equally high among TB/non-TB cases (23% vs 21%), and malnutrition was the main comorbidity among TB cases. The MPT64 test was implementable in the routine diagnostics in a low-resource setting and improved the diagnosis of pediatric EPTB.
Similar content being viewed by others
Introduction
Diagnosing extrapulmonary tuberculosis (EPTB) in children is a challenge. The paucibacillary nature of the disease, the nonspecific clinical presentation, the need for invasive sampling and poor performance of current diagnostic tools such as mycobacterial (Mtb) culture, acid fast bacilli staining (AFB) and GeneXpert MTB/RIF assay (Cepheid, Sunnyvale, California, United States -GeneXpert) adds to the challenge. The current gold standard test, Mtb culture, does not have a perfect sensitivity, has a long turnaround time and has technical and logistical challenges, but is necessary for drug susceptibility testing. The World Health Organization (WHO) has endorsed the use of GeneXpert for EPTB samples1. A recent Cochrane review found varying sensitivity of GeneXpert across different EPTB samples with high specificity2. AFB is of limited diagnostic value3. Most nucleic acid amplification tests, other than GeneXpert, have better sensitivity than Mtb culture, but are complex, technically demanding, and have the risk of contamination3. Furthermore, they are unable to separate between dead and viable bacteria and, except from GeneXpert, gives no drug susceptibility results, all limiting their use in the resource constrained setting3. Fine needle aspiration cytology (FNAC) of mass lesions has high sensitivity, but it is often difficult to distinguish tuberculous lesions form other granulomatous conditions, non-tuberculous mycobacteria and atypical lesions in advanced human immunodeficiency virus (HIV) disease, thereby reducing its specificity3. Histology sampling is invasive and is done less in children and lacks specificity. As a consequence few pediatric EPTB cases are microbiologically confirmed4, and empirical treatment with anti-tuberculosis therapy for presumptive EPTB is often started. This can lead to both over- and undertreatment, thus contributing to excess mortality and morbidity. There is a clear need for better diagnostic tools that are robust, precise and implementable in a low resource setting.
Immunostaining using anti-MPT64 has shown to have comparable sensitivity and specificity to nested polymerase chain reaction3,5. MPT64 is a protein secreted by the mycobacterium tuberculosis complex species. It is not detected in non-tuberculous mycobacteria and Bacillus Calmette-Guerin strains with RD2 deletion6. A recent study in Zanzibar found a sensitivity of 100% for TB adenitis in children when comparing the anti-MTP64 test (MPT64 test) to a composite reference standard7.
Tanzania is one of 30 high burden TB countries8. In 2018 EPTB constituted 20% of the 75,828 notified TB cases, and 14% of all new TB cases were pediatric. 28% of all new TB cases were HIV infected in 20189. Mbeya region in the Southern Highlands of Tanzania, has an HIV prevalence of 9.3% among adults (> 15 years old), with an estimated pediatric (< 15 y) prevalence of 0.5%10. The National Nutrition Survey estimates a prevalence of severe and moderate acute malnutrition of 2.7% in children < 5 years in Mbeya region11. Mbeya Zonal Referral Hospital is a tertiary hospital, and serves approximately 8 million people in six regions in the Southern Highlands.
The aim of this study was to assess if the MPT64 test was implementable in the routine TB care for children at Mbeya Zonal Referral Hospital, and to compare the performance of the test to the routine diagnostic tests including GeneXpert.
Materials and methods
Recruitment of patients, data collection and follow up
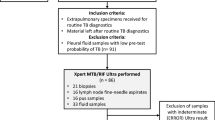
The study was part of a larger study conducted at Mbeya Zonal Referral Hospital to validate the MPT64 antigen detection test. The study design is shown in Fig. 1. Children (0–18 y) with suspected EPTB from both the in- and outpatient services were prospectively enrolled between April 1st 2016 and July 31st 2017. Clinicians were asked to recruit patients with suspected EPTB from both in-and outpatient services. The study protocol did not give any guidance to the clinicians with regards to which symptoms/findings that were compatible with EPTB. Mbeya Zonal Referral Hospital mainly receives referrals from other clinics.
Relevant clinical data was collected through a questionnaire previously developed and validated in a similar study in Zanzibar7. To assess the validity of the questions, the translation of the questions between English/Swahili was done by two separate bilinguals. Any ambiguity in the questions was assessed and corrected after a test among three patients in the Zanzibar study. The questionnaire included questions about sociodemographic characteristics, health seeking behavior, TB knowledge and beliefs and previous medical history. Information about HIV status was obtained from the patient disclosure, and additional HIV testing was performed only per request of the clinicians as per standards of care. Further, radiological examinations and biochemistry was prescribed by the clinicians. Patients who did not consent or had received TB treatment within the last 12 months were excluded. Data collection and clinical examination was done by medical officers hired for the purpose of the study.
Patients were followed up at 2–3 months, at the end of treatment, or until a diagnosis other than EPTB was reached. If the patients had been marked as lost to follow up, a new tracing was performed. In addition, a review of electronic hospital records was done both at Mbeya Zonal Referral Hospital and Baylor College of Medicine Children´s Foundation Tanzania (Baylor) for completeness of clinical data. Baylor provides comprehensive care and treatment for pediatric tuberculosis, HIV/AIDS, malnutrition and other complicated or chronic pediatric conditions in the region.
Diagnostic samples and laboratory tests
Samples were taken from suspected site of infection by the pathologists. Materials from superficial, palpable masses and enlarged lymph nodes were collected using a 22 gauge needle attached to a syringe, while applying minimal negative pressure. The material obtained was smeared on to glass slides for cytological examination, MPT64 staining and Ziehl–Neelsen staining (ZN). Sterile saline was used to rinse the needle and syringe to obtain specimens for Mtb culture and GeneXpert.
Diagnostic tests
Microscopy for AFB was done using ZN. Mtb cultures and GeneXpert samples were sent to the Central Tuberculosis Reference Laboratory located at the Muhimbili National Hospital in Dar es Salaam. Samples were sent in a cool box within two days after sampling using public transportation bi-weekly. The samples were stored at 4 degrees before transportation. Culture was performed on Lowenstein-Jensen medium according to the standard protocol of the Central Tuberculosis Reference Laboratory. GeneXpert was also performed according to the protocol of the Central Tuberculosis Reference Laboratory, in accordance with the WHO protocol.
Cytological slides were stained with the Papanicolaou stain, histological slides with haematoxylin and eosin. On FNAC granulomatous inflammation with/without necrosis or any necrosis (excluding suppurative inflammation) was defined as compatible with TB12. Biopsy findings compatible with TB were defined as the same as the FNAC findings. On cytology, finding of predominantly lymphocytes and/or macrophages, or epitheloid cells and/or necrosis was defined as compatible with TB13,14,15,16,17.
Two technicians at MZRH were trained in the procedure of immunocytochemistry/immunohistochemistry staining (immunostaining). Two pathologists (WM and LT) received training in evaluating immunostaining. The previously alcohol fixed smears were hydrated through decreasing grades of alcohol, washed in distilled water, and incubated with hydrogen peroxide to inhibit endogenous peroxidase activity. Immunostaining was performed as described previously18,19, but with some modification7, by using an in-house polyclonal anti-MPT64 antibody at 1/250 dilution and Dako kit (Dako Envision + System-HRP, K4009, Dako, Glostrup, Denmark) to demonstrate the MPT64 antigens. The primary antibody was then applied and incubated, as described previously7. The immunostained slides were assessed by the local pathologist (WM and LT). The pathologists were blinded for the results of Mtb culture and GeneXpert. The immunostaining was regarded as positive if reddish granular intracytoplasmic staining or extracellular staining was found in necrotic areas, as shown in Fig. 2.
Positive MPT64 staining (red-brown color) in TB cases. Picture (a) MPT64 immunostained smear from pleural effusion showing positive spots (red-brown) within macrophages (X40). Picture (b) MPT64 immunostained smear of CSF showing positive spots within macrophages(X40). Picture (c): MPT64 immunostained smear from FNAC of lymph node. Positive spots for MPT64 are seen and the background shows extensive caseous necrosis (X40). Picture (d) MPT64 immunostained histological section of lymph node of adult patient. Positive spots for MPT64 within cytoplasm of macrophages and background showing granuloma formation and necrosis (X40).
Definitions
Categorization of patients
Patients were classified into the confirmed TB, probable TB, possible TB and not TB groups according to a composite reference standard (CRS), as shown in Table 1.
Malnutrition, immunosuppression and severity of EPTB manifestations
Severe and moderate acute malnutrition was defined by the clinicians in Mbeya Zonal Referral Hospital and Baylor using WHO 2006 growth references11. Severe and moderate cases were merged as ´Malnutrition´ for analysis. HIV infected patients, patients with suspected hematological malignancies, lymphomas and patients on immunosuppressive drugs were grouped together as ´Immunosuppression´ for statistical analysis. For statistical analysis TB adenitis was labelled as ´non-severe TB´ and all other EPTB manifestations were labelled ´severe-TB´.
Ethical considerations
The project was approved by the Regional Committee for Medical Research Ethics in Norway, REK Helse-Vest (2014/46/REK vest), and the Ethical committee for biomedical research at the National Medical Research Coordinating Comittee in Tanzania with ethical clearance reference number NIMR/HQ/R.8a/Vol.IX/2142. All experiments were performed in accordance with relevant guidelines and regulations. Written informed consent and assent (for under 18 y) were obtained from all patients or caretakers. Invasive sampling was done per request of the clinicians based on patient management, not primarily for study purposes. Patients were HIV tested routinely, and not for the purpose of the study.
Statistical analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) for Mac, version 25.0. Chi square test was used to assess differences in categorical variables. Not normally distributed variables were assessed using non-parametric tests. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy was calculated using cross-tabulation. A p-value < 0.05 was considered as statistically significant.
Results
Patient characteristics
A total of 63 patients were included in the study, as shown in Fig. 1. Per the CRS, 30 (49%) patients were classified as TB cases; 10 (33%) confirmed, 12 (40%) probable and 8 (27%) possible, respectively. 31 (51%) patients were classified as non-TB cases. 2 cases were unclassifiable and were excluded from further analysis.
Table 2 shows the baseline characteristic of the two groups. The median age in the TB and non-TB group was 8 and 10 years, respectively. There was not a significant difference in gender distribution among the two groups, but within the TB group the significant majority of cases were male (70%). A statistically significant higher proportion of patients in the TB group were recruited as inpatients.
The sites of suspected disease were heterogeneous. In the TB group, the three most common infections were adenitis (30%), peritonitis (30%) and meningitis (20%). Non-severe disease was more prevalent than severe disease in the non-TB group.
Overall, 8/55 (15%) patients were HIV positive. There was a non-significant difference in numbers of HIV infected between the TB and non-TB group. Malnutrition was the main comorbidity, with 17 patients (29%) being malnourished. Malnutrition was more prevalent among TB patients, with a prevalence of 43% vs 13% in the TB and the non-TB patients, respectively.
The two major non-TB diagnosis were malignancies (11/31) and other infectious conditions (10/31). Among other infectious conditions abscesses (4/31), bacterial meningitis (2/31), and one case each of pneumonia with empyema (1/31), cryptococcal meningitis (1/31), chronic otitis media (1/31) and suppurative lymphadenitis (1/31), were found. Benign tumors (3/31), unspecific lymphadenopathy (3/31) and undefined (4/31) were also found.
Impact of malnutrition and immunosuppression on disease severity
The patients with malnutrition had a statistically significant higher prevalence of TB than those without malnutrition (76% vs 40%, respectively, p = 0.012). The malnourished patients were significantly younger (median 4 y vs 11 y, p = 0.003)). The patients with malnutrition had a trend towards more severe sites of infection (76% vs 50%) and higher mortality (36% vs 16%), however both trends were not statistically significant.
Among the malnourished patients, the final diagnosis was EPTB (13/17); peritonitis (4/17), meningitis (4/17), adenitis (2/17), disseminated TB (2/17), pulmonary TB with concomitant adenitis (1/17), and non-TB (4/17); hematological malignancies (2/17), lymphoma (1/17) and bacterial meningitis (1/17).
Immunosuppression in some form was present in 33 patients (55%). The group of immunosuppressed did not differ significantly with age, gender, disease site severity or mortality when compared to patients without immunosuppression. However, there was a trend towards increased mortality (32% vs 10%, p = 0.078) in the immunosuppressed group.
Among the immunosuppressed patients, the final diagnosis was EPTB (19/33), malignancies (10/33), unspecific lymphadenopathy (2/33) and infectious conditions (2/33).
Mortality
The mortality did not differ significantly between the TB (23%) and non-TB (21%) groups. TB meningitis (3/10), TB pleuritis (2/10), TB peritonitis (1/10) caused mortality in the TB group, and lymphoma (2/10), hematological malignancy (1/10) and cryptococcal meningitis (1/10) in the non-TB group. Severe-TB and hospitalization were significantly associated with increased mortality by using chi-square. However, a logistic regression analysis of various factors associated with mortality did not find any variables to be statistically significant.
Diagnostics tests
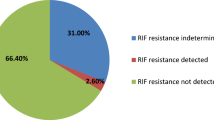
Table 3 shows the performance of all diagnostic tests for different samples. The MPT64 test performed better than Mtb culture, GeneXpert and ZN staining, with a sensitivity of 92%. No samples were positive with ZN staining. Specificity of the MPT64 test was lower than the other diagnostic tests, but acceptable at 88%.
Table 4 shows the 95% C.I., sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy for all tests. The MPT64 test had a comparable PPV to GeneXpert, but a higher NPV than both Mtb culture and GeneXpert. The accuracy of the MPT64 test was higher than the other test. FNAC had a comparable sensitivity and specificity to the MPT64 test.
Of the 30 TB cases, 26 had samples that were analyzed with the MPT64 test. Only 2 (8%) were negative; both of these tests were performed on ascites, giving a sensitivity of 75% (6/8) for ascites. One of these samples was positive for both Mtb culture and GeneXpert, and this is the only sample that had a discordant result of MPT64 and Mtb culture/GeneXpert. All remaining 24 TB cases examined with the MPT64 test were positive.
Table 5 show the correlation between diagnostic tests and findings on FNAC and cytology. The MPT64 test had a good correlation with positive findings on FNAC. The MPT64 test also had a better correlation with cytology findings compatible with TB than Mtb culture and GeneXpert.
An independent reading of the immunostaining of 20 slides was performed by LS to assess the quality of the reading of the test. There was agreement on 11 positive MPT64 slides, 2 had a discordant result, and 7 slides were labelled by LS as inconclusive. Only 1/7 was also marked as inconclusive by the local pathologists.
Discussion
This was a real-life study in the high TB and HIV prevalence setting where the MPT64 test was implemented in the routine EPTB diagnostics and used by the clinicians. The MPT64 test had a sensitivity of 92%, and performed far better than conventional tests such as Mtb culture and the WHO recommended GeneXpert in children with varied EPTB presentations. This is the second study where we have shown that the test is implementable in a basic pathology laboratory facility in a low-resource setting7. The results are consistent with results in the more controlled setting and shows that the MPT64 test can help in diagnosing pediatric EPTB5.
Our sample size is small with 30 EPTB patients in total. It is therefore difficult to make a good assessment of performance for different sites of disease. A recent study in Zanzibar found a sensitivity of the MPT64 test of 100% for pediatric TB adenitis7. In our study the risk for false negative MPT64 test results was low, which highlights its potential role as a confirmatory test for EPTB, adding sensitivity and timeliness to Mtb culture. As only 16 non-TB samples was assessed by the MPT64 test, the specificity (88%) could have been both under- or overestimated. Three non-TB samples had an uncertain MPT64 result, and were removed from the analysis of specificity. A conclusive result on these samples could have both increased or decreased the specificity of the MPT64 test.
The quality assessment performed by LS shows that many slides (7/20) were labelled as inconclusive by an outside pathologist from a Norwegian university hospital. 5/7 were labelled as uncertain due to poor quality of the slide. However, the pathologists in Mbeya Zonal Referral Hospital that had assessed over 250 MPT64 slides stained locally, did not report this ambiguity. This underlines that the result of the MPT64 test is dependent on the reader, and familiarity with local variations in staining patterns and artifacts.
Mtb culture performed poorer than the MPT64 test, but the assessment of its performance could have been affected by the number of contaminated samples. 10 Mtb culture samples were contaminated, of which 7 among TB patients. The overall sensitivity of Mtb culture on 22 samples was 45%. The transportation of samples to the Central Tuberculosis Reference Laboratory in Dar es Salaam could have affected the performance of Mtb culture both positively and negatively. However, being necessary for drug susceptibility testing, the long turn-around time and poor sensitivity of the test makes it less feasible as a stand-alone test. The poorer sensitivity of Mtb culture of 13% for EPTB samples is confirmed in our Zanzibar study7. Mtb culture remains an important diagnostic test despite its limitations and efforts should be made to improve the method through better laboratory facilities.
GeneXpert had a lower sensitivity of 31% as compared to Mtb culture (45%). Two samples (20%) were Mtb culture positive and GeneXpert negative. In previous studies GeneXpert has been shown to have a comparable, but slightly lower sensitivity than Mtb culture for various EPTB samples1,2. The advantage of GeneXpert compared to Mtb culture is the turn-around time, and in this study the reduced risk of inconclusive or contaminated results. A positive test result is very useful due to the high specificity, but the risk of false negatives is high, reducing its role as a stand-alone test for EPTB. The cost of GeneXpert when not subsidized is also a source for sustainability concerns20.
FNAC performed excellent in this study with a sensitivity of 90% and a specificity of 95%. These findings support the use of this simple test for diagnosis of EPTB. FNAC is simple, can be performed decentralized, slides can be prepared and sent to a central laboratory. However, due to the small sample size in our study (10 TB and 21 non-TB samples), the results should be interpreted with caution. FNAC has been shown to be unspecific in other settings, and diseases such as sarcoidosis, non-tuberculous mycobacteria and other granulomatous conditions can mimic TB3. The MPT64 antigen detection test can be used as a confirmatory test in cases where there is a suspicion for other granulomatous conditions. The pathologists did not report a suspicion of any non-TB granulomatous conditions in this study, which is similar to the results from Zanzibar. The MPT64 test had a correlation of 100% with positive FNAC results in our study. One FNAC sample did not show typical features of TB adenitis, but was MPT64 positive. The results from Zanzibar also supports a potential use of MPT64 as a confirmatory test, separating TB from non-TB related necrosis in lymphadenitis.
Cytological findings in cell smears of the effusions lacked both specificity and sensitivity to diagnose EPTB. The MPT64 test was positive in 14/16 TB cases that had effusions sampled, indicating the utility of the test in various types of samples. However, due to a small sample size, the results need to be validated in further studies.
The superior performance of MTP64 compared to Mtb culture and GeneXpert can be attributed to the paucibacillary nature of EPTB, and the potential role of antigen accumulation as a central part of EPTB pathogenesis. Antigen accumulation, rather than the bacillary load has been described as the central phenomenon in TB pathogenesis and tissue destruction21,22.
Accounting for the fact that Mtb culture is an imperfect gold standard, the MPT64 test was compared to a composite reference standard (CRS). We have included response to treatment to TB treatment as a part of the CRS to mimic real life practice. However, response to treatment is not conclusive as especially Rifampicin is fairly wide-spectred and would treat many conventional bacterial infections. The CRS accounted for this uncertainty by labeling patients with grades of certainty of their diagnosis; confirmed, probable, possible. The use of a CRS comes with a risk of misclassification bias. The MPT64 test was implemented and used by the clinicians, and some patients were started on TB treatment on the basis of their MPT64 result. If MPT64 had a tendency of being false positive in other infectious conditions, these patients could have been misclassified as TB cases. However, only two TB adenitis cases have been labelled as TB cases on the basis of response to treatment. One of these cases was MPT64 positive, and the other had a missing MPT64 test result.
In our study the prevalence of peritonitis (30%) and meningitis (20%) was higher than the usual distribution of pediatric EPTB sites. The severe presentations do not seem to be explained by a lack of BCG coverage, as BCG coverage was very good in our cohort. With concomitant malnutrition the severe presentations of TB peritonitis and meningitis is not surprising, but is not well documented in other studies23. Immunosuppression due to malnutrition, young age among the malnourished and recruitment as inpatients could have been contributing factors.
The prevalence of malnutrition was very high (29%). Malnutrition was more prevalent among the TB patients, as compared to the non-TB group, highlighting the need for a high level of clinical suspicion of not only pulmonary, but also extrapulmonary TB in this patient group. This is supported by a recent study in Ethiopia showing a higher incidence of malnutrition in adults with EPTB than in those with PTB24. From previous research it appears that malnutrition is a predictor of tuberculosis disease and is associated with worse outcomes23,25. In our study, 13/17 (76%) of the malnourished patients had EPTB, with peritonitis (4 patients) and meningitis (4 patients) being the most prevalent. Only 1/8 HIV infected patients had malnutrition, which reduces its potential impact on malnutrition in this study. Three of the malnourished patients had malignancies as their final diagnosis, which highlights that the malnourished patients in this study had serious concomitant diseases.
Both Mtb culture and GeneXpert performed poorer in the malnourished, with sensitivities of 30% and 25%, respectively. The MPT64 test had a sensitivity of 90%, but the results have to be interpreted with caution as only 10 samples were asessed. Also, surprisingly, the sensitivity of Mtb culture and GeneXpert did not improve in immunosuppressed patients (sensitivity of 38% and 28% respectively), where one would expect that the poor immune response of the host would lead to a greater bacterial load.
The mortality rate was equally high in the TB and non-TB group (23% vs 21%). However, these results could have been affected by the high number of patients lost to follow up in the non-TB group (13% vs 39%, TB versus non-TB group, respectively), masking a potential lower mortality rate in the non-TB group. When looking at mortality through the lens of malnutrition, one sees a trend towards increased mortality in this group with a mortality rate of 36%. A recent systematic review from Ethiopia found a double incidence of death in children < 5 y with severe acute malnutrition (SAM) and concomitant TB, and a high case fatality rate of SAM at 11.3%26. However, it is not specified if cases of EPTB are included in the review and their potential contribution to excess mortality. The contribution of TB to excess mortality in pediatric SAM is also reproduced in Zambia with a case fatality rate among children with SAM and TB of 56%. However, 94% of the TB cases in the Zambian study were pulmonary and the HIV prevalence was higher at 46.5% among SAM patients. The low number of EPTB cases in this study could point towards under detection27. Estimating the mortality rate of pediatric EPTB is challenging due to the lack of uniform case definitions and lack of standardized follow ups. Unfortunately, our small sample size reduces the strength of the analysis of contributing factors to mortality.
The trend of increased mortality was stronger in the group that included all causes of immunosuppression. In total, 10/61 patients died, of which 8 had immunosuppression. 6 patients that died had TB, 3 had malignancies. This highlights the need for a comprehensive evaluation of patients to ensure that various reasons of immunosuppression are considered.
Mbeya Zonal Referral Hospital is a tertiary referral hospital with laboratory services, radiology services and a histopathology lab. In this setting 51% of the presumptive EPTB cases were not classified as TB cases. In an even more resource constrained setting these patients could have been subject to a trial of TB treatment on suspicion of EPTB, leading to unnecessary treatment and diagnostic delay or even a wrong diagnosis. In our study the potential differential diagnosis ranged from benign conditions to life threatening conditions. 11/61 (18%) were diagnosed with malignancies and 10/61 (16%) with other infectious conditions. This highlights the need for diagnostic facilities and an awareness of differential diagnosis when examining patients with suspected pediatric EPTB. Under TB control programs only treatment for EPTB is free of cost, but all the diagnostic work-up incurs great financial burden on the patients. Diagnostic delay could have been a contributing factor to the high mortality. Early detection and timely referral of presumptive EPTB from local clinics to the tertiary hospital is probably needed to ensure a correct diagnosis and to reduce mortality.
In conclusion, the MPT64 test was implementable in the routine TB diagnostic setting in a tertiary hospital in a low-resource, high TB and HIV setting, and the test performance was better than routine diagnostic tests, including GeneXpert. However, this test cannot be implemented until a basic laboratory structure is available and health systems are strengthened. The method of immunostaining used in the MPT64 test is also useful for strengthening diagnosis of other diseases, especially cancers.
References
WHO. Automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB/RIF assay for the diagnosis of pulmonary and extra- pulmonary TB in adults and children. Policy update., (WHO, Geneva, WHO, 2013, 2013).
Kohli, M. et al. Xpert((R)) MTB/RIF assay for extrapulmonary tuberculosis and rifampicin resistance. Cochrane Database Syst. Rev. 8, CD012768. https://doi.org/10.1002/14651858.CD012768.pub2 (2018).
Purohit, M. & Mustafa, T. Laboratory diagnosis of extra-pulmonary tuberculosis (EPTB) in resource-constrained setting: State of the art, challenges and the need. J. Clin. Diagn. Res. 9, 1–6. https://doi.org/10.7860/JCDR/2015/12422.5792 (2015).
WHO. Global Tuberculosis Report 2019. (Geneva, WHO, 2019, 2020).
Purohit, M. R., Sviland, L., Wiker, H. & Mustafa, T. Rapid and specific diagnosis of extrapulmonary tuberculosis by immunostaining of tissues and aspirates with anti-MPT64. Appl. Immunohistochem. Mol. Morphol. 25, 282–288. https://doi.org/10.1097/PAI.0000000000000300 (2017).
Mahairas, G. G., Sabo, P. J., Hickey, M. J., Singh, D. C. & Stover, C. K. Molecular analysis of genetic differences between Mycobacterium bovis BCG and virulent M. bovis. J. Bacteriol. 178, 1274–1282. https://doi.org/10.1128/jb.178.5.1274-1282.1996 (1996).
Jorstad, M. D., Marijani, M., Dyrhol-Riise, A. M., Sviland, L. & Mustafa, T. MPT64 antigen detection test improves routine diagnosis of extrapulmonary tuberculosis in a low-resource setting: A study from the tertiary care hospital in Zanzibar. PLoS ONE 13, e0196723. https://doi.org/10.1371/journal.pone.0196723 (2018).
Senkoro, M. et al. Prevalence of pulmonary tuberculosis in adult population of Tanzania: A national survey, 2012. Int. J. Tuberc Lung Dis. 20, 1014–1021. https://doi.org/10.5588/ijtld.15.0340 (2016).
Ministry of Health, T. The National Tuberculosis and Leprosy Programme-Annual report for 2018. (Ministry of Health, Tanzania, The United Republic of Tanzania, 2018, 2018).
Tanzania, M. o. H. Tanzania HIV Impact Survey (THIS) 2016–2017: Final Report., (Ministry of Health, 2018).
Ministry of Health, C. D., Gender, Elderly and Children (MoHCDGEC) [Tanzania & Mainland], M. o. H. M. Z., Tanzania Food and Nutrition Centre (TFNC), National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS) [Zanzibar] and UNICEF. Tanzania National Nutrition Survey using SMART Methodology (TNNS) 2018. (2018).
Hemalatha, A., Shruti, P., Kumar, M. U. & Bhaskaran, A. Cytomorphological patterns of tubercular lymphadenitis revisited. Ann. Med. Health Sci. Res. 4, 393–396. https://doi.org/10.4103/2141-9248.133466 (2014).
Marais, S. et al. Tuberculous meningitis: A uniform case definition for use in clinical research. Lancet. Infect. Dis 10, 803–812. https://doi.org/10.1016/s1473-3099(10)70138-9 (2010).
Koh, W. J. Progression of tuberculous pleurisy: From a lymphocyte-predominant free-flowing effusion to a neutrophil-predominant loculated effusion. Tuberc Respir. Dis. (Seoul) 80, 90–92. https://doi.org/10.4046/trd.2017.80.1.90 (2017).
Valdes, L. et al. Diagnosing tuberculous pleural effusion using clinical data and pleural fluid analysis A study of patients less than 40 years-old in an area with a high incidence of tuberculosis. Respir. Med. 104, 1211–1217. https://doi.org/10.1016/j.rmed.2010.02.025 (2010).
Vaid, U. & Kane, G. C. Tuberculous peritonitis. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.TNMI7-0006-2016 (2017).
Bielsa, S. et al. Comparison of polymorphonuclear- and lymphocyte-rich tuberculous pleural effusions. Int. J. Tuberc. Lung Dis. 17, 85–89. https://doi.org/10.5588/ijtld.12.0236 (2013).
Purohit, M. R., Mustafa, T., Wiker, H. G., Morkve, O. & Sviland, L. Immunohistochemical diagnosis of abdominal and lymph node tuberculosis by detecting Mycobacterium tuberculosis complex specific antigen MPT64. Diagn. Pathol. 2, 36. https://doi.org/10.1186/1746-1596-2-36 (2007).
Purohit, M. R., Mustafa, T., Wiker, H. G. & Sviland, L. Rapid diagnosis of tuberculosis in aspirate, effusions, and cerebrospinal fluid by immunocytochemical detection of Mycobacterium tuberculosis complex specific antigen MPT64. Diagn. Cytopathol. 40, 782–791. https://doi.org/10.1002/dc.21637 (2012).
Branigan, D. OPEN LETTER: Time to Lower the Price of Xpert Cartridges to US$ 5. https://msfaccess.org/open-letter-time-lower-price-xpert-cartridges-us (2019).
Hunter, R. L. The pathogenesis of tuberculosis-the Koch phenomenon reinstated. Pathogens https://doi.org/10.3390/pathogens9100813 (2020).
Mustafa, T., Phyu, S., Nilsen, R., Jonsson, R. & Bjune, G. A mouse model for slowly progressive primary tuberculosis. Scand. J. Immunol. 50, 127–136. https://doi.org/10.1046/j.1365-3083.1999.00596.x (1999).
Sinha, P. et al. Undernutrition and tuberculosis: Public health implications. J. Infect. Dis. 219, 1356–1363. https://doi.org/10.1093/infdis/jiy675 (2019).
Feleke, B. E., Feleke, T. E. & Biadglegne, F. Nutritional status of tuberculosis patients, a comparative cross-sectional study. BMC Pulm. Med. 19, 182. https://doi.org/10.1186/s12890-019-0953-0 (2019).
Jaganath, D. & Mupere, E. Childhood tuberculosis and malnutrition. J. Infect. Dis. 206, 1809–1815. https://doi.org/10.1093/infdis/jis608 (2012).
Wagnew, F., Worku, W., Dejenu, G., Alebel, A. & Eshetie, S. An overview of the case fatality of inpatient severe acute malnutrition in Ethiopia and its association with human immunodeficiency virus/tuberculosis comorbidity—A systematic review and meta-analysis. Int. Health 10, 405–411. https://doi.org/10.1093/inthealth/ihy043 (2018).
Munthali, T. et al. Tuberculosis caseload in children with severe acute malnutrition related with high hospital based mortality in Lusaka, Zambia. BMC Res. Notes 10, 206. https://doi.org/10.1186/s13104-017-2529-5 (2017).
Acknowledgements
We thank Prof. Harald G. Wiker for his efforts in developing the polyclonal antibody, Melissa Davidsen Jørstad for developing the questionnaires and routines used in the study, The National Tuberculosis and Leprosy Programme and the Central Tuberculosis Reference Laboratory at Muhimbili National Hospital in Dar es Salaam for supporting the study, Baylor College of Medicine Children´s Foundation Tanzania for recruitment of patients and their collaboration, Paul Mwanyika and Fausta Selemani Michael for their dedicated recruitment, treatment and follow up of patients in the Pediatric department in Mbeya Zonal Referral Hospital, Anthony Ambikile Nsojo in the Research department at Mbeya Zonal Referral Hospital for facilitating the study, the Histopathology unit at Mbeya Zonal Referral Hospital, pathologists Msafiri Marijani from Mnazi Mmoja Hospital and Innocent Mosha from Muhimbili National Hospital for their commitment to the patients and the study.
Author information
Authors and Affiliations
Contributions
T.M. performed the conceptualization, funding acquisition and developed the methodology, E.G. performed the data curation, formal analysis and writing of the article, M.N. performed data curation and investigations, L.T. and W.M. performed the investigations and sampling, L.S. helped develop the methodology and conducted the formal training of L.T. and W.M., E.N. and S.M. were responsible for the project management and helped in the conceptualization. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grønningen, E., Nanyaro, M., Sviland, L. et al. MPT64 antigen detection test improves diagnosis of pediatric extrapulmonary tuberculosis in Mbeya, Tanzania. Sci Rep 11, 17540 (2021). https://doi.org/10.1038/s41598-021-97010-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-97010-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.