Abstract
Retrograde transpubic screw fixation is a common procedure for the treatment of anterior pelvic ring fractures. With its sparing surgical approach and significant pain relief after screw fixations allowing early mobilisation, it has gained importance especially in the treatment of insufficiency fractures in elderly patients. However, positioning of transpubic screw osteosynthesis is not always possible due to narrowness and curvature of the screw corridor. The aim of the present study was to evaluate availability and length of the screw corridor using a 3D statistical model of the pelvic ring consisting out of 150 uninjured pelves. Virtual bore probes with a diameter of 7.5 mm were analysed as to accessibility, length and grey value distribution in Hounsfield Unit (HU). A transpubic corridor with a diameter of ≥ 7.5 mm was available in 185 of 300 investigated superior pubic rami with mean screw length of 131.7 mm. Accessibility of the screw corridor was higher in males than in females. However, screw length showed no systematic differences between the sexes or ethnicities. Analysis of the grey value distribution demonstrated the strongest bone to be located at the lateral ilium and the supraacetabular region.
Similar content being viewed by others
Introduction
Retrograde transpubic screw fixation is a frequently used surgical procedure for the treatment of fractures of the anterior pelvic ring1,2,3,4. It is a minimally invasive procedure which can be used in minimally or non-displaced fractures of the superior pubic ramus. In cases with displacement of fracture fragments, retrograde screw osteosynthesis can be performed after closed or open reduction5. Alternatively, a reduction manoeuvre utilizing a provisional screw can be used6. The latter method has gained importance especially in the treatment of geriatric patients with fragility fractures of the pelvic ring due to its sparing surgical approach, significant pain reduction after stabilisation and subsequent early mobilisation of the patient7,8,9,10,11. As the number of geriatric fractures increases, percutaneous fixation methods become more relevant12,13,14,15.
Several biomechanical studies have investigated the stability of screw osteosynthesis of the anterior pelvic ring16,17. Various clinical studies and case series have demonstrated low complication rates and good to excellent clinical results1. However, some concerns regarding this method are remaining. Positioning of the retrograde transpubic screw is not always possible without affecting the acetabular joint surface due to the curvature of the screw corridor. Proximity of crucial neurovascular structures such as the ilioinguinal and genitofemoral nerves and the obturator and the external pudendal artery around the entry point, as well as the external iliac vessels passing just proximal the superior pubic ramus with direct contact to the bone, can be critical and limiting for the procedure18. Further, not in every patient a screw with an adequate diameter can be placed due to narrowness of the screw corridor19,20,21. In addition, screw loosening, backing out and pseudarthrosis are described as potential complications during follow-up1,22,23.
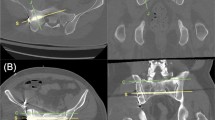
The aim of the present study was the evaluation of the potential screw corridor for positioning a screw with a diameter of 7.3 mm, as well as the analysis of the local bone stock within the screw corridor. Figure 1 shows the status after bilateral retrograde transpubic screw fixation of bilateral superior pubic rami fractures and an additional posterior fixation in a trauma patient with pelvic ring fracture.
Bilateral retrograde transpubic screw fixation in a patient pelvic ring fracture after traffic accident (a) ap view (b) inlet view (c) outlet view. This figure was generated using the software Sectra PACS (Version 22.1, Linköping, Sweden; www.medical.sectra.com).
Material and methods
Analysis was performed based on a 3D statistical model of the pelvic ring comprising of 150 CT scans of uninjured adults (100 Europeans: 51 male, 49 female, average age 60.0 ± 13.1 years; 50 Japanese: 30 male, 20 female, average age 74.3 ± 17.5 years). Average image resolution of the raw data was 0.7 × 0.7 × 0.6 mm. CT scans had been acquired for indications not related to the musculoskeletal system prior to the start of the study. The study was approved by the local ethics committee (Ethikkommission Bundesland Salzburg, Austria). Informed consent was obtained from all patients, data acquisition, processing and analysis were in accordance with all legal regulations and guidelines.
The 3D statistical model was computed using the software Amira (Amira version 6.0.0, FEI, Hillsboro, OR, USA) as previously described by our group24. The usage of a statistical model, consisting out of more than 300.000 homologous surface triangles, allowed for a landmark-based definition of the individual screw corridor.
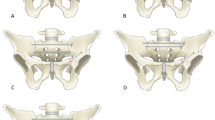
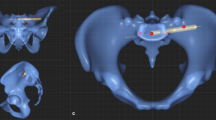
Thus, virtual screw positioning was performed by defining entry and exit point of the screw on the 3D surface models using Amira software. The overall mean model and each of the 150 individual computer models were oriented in a way allowing for a direct view into the screw corridor, described as gun barrel view25 (Fig. 2a). In a second step, orientation was adjusted so that the maximum diameter of the screw corridor was displayed (Fig. 2b). The landmarks defining entry and exit point of the virtual screw were positioned in the region of the pubic tubercle and the posterior ilium in the center of the projected corridor (Fig. 2c). Between those two landmarks, a virtual bore probe with a diameter of 7.5 mm was placed in order to simulate screw positioning. Length and local grey values of the virtual bore probe were analyzed in 1 mm steps26. The corridor’s dimensions were defined to allow screw positioning if that bore probe with a diameter of 7.5 mm would not affect surrounding cortical bone along the corridor except for the entry and exit points. Affecting cortical bone was defined by exceeding a threshold of 400 HU27,28,29. This calculation was performed on the overall mean model and on both pubic ramus of all bone models resulting in a total of 300 individual bore probes available for evaluation. In case of perforation of cortical bone, except for the entry and exit points, the screw corridor was judged as not accessible and the sample was excluded from length analysis. In all samples with an available screw corridor, screw length was measured. For further evaluation of the local bone stock, the pattern of bone stock distribution of every single sample with an available screw corridor was normalized to the average screw length and graphically visualized.
(a) Orientation of the 3D model in so-called gun barrel view25, (b) screw corridor (marked in red), (c) marked screw entry point in the center of the corridor (green dot). This figure was generated using the software Amira (Version 6.0.0, FEI, Hillsboro, OR, USA; www.fei.com).
The excluded samples were analyzed regarding the exact localization of undesired cortical perforation and categorized in three groups: perforation along the superior pubic ramus (group 1), perforation of the acetabular joint surface (group 2), perforation along the superior pubic ramus and of the acetabular joint surface (group 3).
Statistical analysis was performed applying Mann–Whitney-U test for independent samples and Pearsons’s Chi-Square analysis using the software SPSS (IBM SPSS Statistics 24, IBM, Armonk, NY, USA). Level of significance was set to a = 0.05.
Ethical approval
All methods were carried out in accordance with the relevant guidelines and regulations. CT data were used retrospectively and anonymized with patient’s informed consent and approval of the local ethics committee (Ethikkommission Bundesland Salzburg, Austria).
Results
A transpubic corridor with a diameter of ≥ 7.5 mm was available in 185 of 300 investigated superior pubic rami (61.7%; 110 male (67.9%), 75 female (54.3%)). Pearsons’s Chi-Square analysis showed no statistically significant relation between sex and availability of screw corridor (Chi-Square(1) = 7.205; p = 0.10). Mean length of the corridor was measured with 131.7 mm (standard deviation ± 10.7 mm). Mean length in the male samples was 131.5 mm (± 10.2 mm), and 132.1 mm (± 11.5 mm) in the female samples. No relevant sex-related difference in screw length was observed with p = 0.651. With respect to ethnicity, no statistically significant difference was shown neither regarding availability of the screw corridor nor the screw length with a mean screw length of 131.6 mm in Europeans and 131.9 mm in Japanese (p = 0.844) (Table 1).
The local grey value distribution of the included samples showed a consistent pattern with a peak at the first cortex perforation in the area of pubic tubercle. Low HU values were seen along the superior pubic ramus, while higher values with an intermediate peak were present in the subchondral bone around the acetabulum with at least a peak of high HU values passing the cortical bone of the lateral ilium. Figure 3 displays the grey value distribution along the screw corridor.
Analysis of the excluded samples showed that cortical perforation occurred predominantly at the acetabulum (group 2) in the male samples while in females the perforation was observed to be more often located at the pubic ramus and the acetabulum (group 3). Figure 4 and Table 2 show the distribution of the perforation site.
Mean local grey value distribution measured along the screw corridor showing a first cortical peak at the entry point, lower HU in the superior pubic ramus, slightly higher grey values in the periacetabular trabecular bone and a strong second cortical peak finally passing the cortex of the lateral ilium.
Samples with undesired cortical screw perforation, the figure shows distribution across the three defined zones in relation to sex; x-axis shows the area of cortical perforation (group 1 = perforation along the pubic ramus; group 2 = perforation of the acetabular joint surface; group 3 = perforation along the pubic ramus and the acetabular joint surface), y-axis shows the number of samples.
Discussion
In the present study, almost two thirds of individuals have sufficiently sized transpubic corridors to position a retro- or antegrade transpubic screw. There was no difference in sex or ethnicity concerning length of the corridor. Intermediate grey values were observed in the subchondral region adjacent to the acetabulum, and high grey values in the lateral cortex of the ilium.
Retrograde transpubic screw fixation is a frequently used method to treat fractures of the anterior pelvic ring30. Several studies have investigated the screw corridor. Suzuki et al. performed a CT-based evaluation of the screw corridor on 160 CT data sets regarding length and diameter of the corridor. They found a mean length of the corridor of 124.6 mm in men and 123.8 mm in women. Minimal diameters were 13.5 mm in men and 10.7 mm in women in this study20. In contrast, Attias et al. published in a study on 13 individual, CT-based computer models a mean maximum screw length of 173.5 mm and a mean maximum virtual diameter for a potential implant of 6.4 mm31. Puchwein et al. investigated the corridor length and diameter in 50 CT polytrauma scans (35 male, 15 female) without pelvic injuries. The corridor was always available with a mean length of 127.2 mm and mean minimal diameter of 14.6 mm32.
Several biomechanical studies compared retrograde screw osteosynthesis with plate osteosynthesis. Simonian et al. showed that with a 4.5 mm retrograde transpubic screw, stability is similar to a conventional 3.5 mm plate osteosynthesis33. Acklin et al. compared a 7.3 mm screw osteosynthesis with ten-hole plate osteosynthesis. By using six of the ten possible screw options, a significantly higher stability of the plate osteosynthesis was shown under cyclic loading17. Another study of the same group showed a similar stability for a 7.3 mm screw compared to two 3.5 mm screws in the same biomechanical test setup16.
The present study shows consistent results in measurements of the length of a retrograde transpubic screw in adult pelves without relevant sex- or ethnicity-related differences. In the literature, screw length is reported at significant variability with mean screw length measurements, i.e. between 124 mm20 and 174 mm31. In our study, we included only those pelves which allowed for the positioning of a screw reaching the cortex of the lateral ilium without cortical affection of the bone except from entry and exit point. Consequently, shorter screws ending medial to the acetabulum were excluded from analysis. This might have resulted in the observation of a relatively higher screw length as reported in other studies20,32.
Although there was no sex-related difference of the screw length observed, we could show that screw positioning was less frequently possible in females than in males. This might be related to a narrower corridor with greater curvature due to sex-related anatomical characteristics24. For the same anatomical reasons, the site of undesired cortical perforation in the excluded samples appears to be sex-related.
Analyzing the grey value distribution following the screw corridor, we observed the strongest bone, as expected, on site of the lateral ilium. But the analysis showed also higher HU in the trabecular bone of the periacetabular region. We conclude that, at least the periacetabular region should be reached with the screw thread to achieve a sufficient anchoring, even if the positioning of a bicortical screw is not possible without affecting the acetabular joint surface due to the individual anatomical configuration. The results of the grey value analysis suggest that a retrograde transpubic screw fixation might provide a higher stability than an antegrade fixation due to the strong cortical bone of the lateral ilium and therefore more sufficient anchoring of the screw thread. A biomechanical study on synthetic bone models by Osterhoff et al. showed no differences regarding construct survival and stability between ante- and retrograde transpubic screw fixation34. According to our results, biomechanical testing on human bones is needed for further investigation due to the uneven bone mass distribution with relevant differences in quality and thickness of both, the cancellous and the cortical bone over the pelvis which can be not fully reproduced with the synthetic bone model.
As a limitation of the study it must be mentioned that the investigation was performed on uninjured pelvis. In treatment of fractures of the anterior pelvic ring, an exact anatomical reduction is not always necessary. Consequently, the accessibility of the screw corridor might be positively influenced by the fracture itself allowing slightly more flexibility for screw placement. Our results might therefore report a rather pessimistic number of possible transpubic screws. Further, also the usage of screws with a smaller diameter has to be discussed as a smaller diameter might increase the accessibility of the screw corridor. In our study, we used a virtual screw with a diameter of 7.3 mm as this is the implant we use in daily clinical practice for transpubic screw positioning with good clinical1 and biomechanical16,17 results available.
In conclusion, the present study shows that positioning of a transpubic screw was possible in almost two thirds of the examined samples. Possibility of screw positioning depends on individual anatomical characteristics determining the dimensions of the screw corridor. Therefore, transpubic screw fixation has to be planned carefully preoperatively with respect to the patient’s individual anatomy. The highest HU values were found, beside the cortex of the lateral ilium, in the trabecular bone of the periacetabular region which makes us assume that screws anchored with the thread in those regions might provide the highest stability.
References
Rommens, P. M. et al. Minimal-invasive stabilization of anterior pelvic ring fractures with retrograde transpubic screws. Injury 51, 340–346 (2019).
McLachlin, S. et al. Biomechanical analysis of anterior ring fixation of the ramus in type C pelvis fractures. Eur. J. Trauma Emerg. Surg. 44(2), 185–190 (2018).
Rommens, P. M. Fragility Fractures of the Pelvis 1st edn. (Springer, 2017).
Rommens, P. M. Is there a role for percutaneous pelvic and acetabular reconstruction?. Injury 38(4), 463–477 (2007).
Weatherby, D. J., Chip Routt Jr, M. L. & Eastman, J. G. The retrograde-antegrade-retrograde technique for successful placement of a retrograde superior ramus screw. J. Orthop. Trauma 31(7), 224–229 (2017).
Mosheiff, R. & Liebergall, M. Maneuvering the retrograde medullary screw in pubic ramus fractures. J. Orthop. Trauma 16(8), 594–596 (2002).
Arduini, M. et al. Fragility fractures of the pelvis: Treatment and preliminary results. Aging Clin. Exp. Res. 27(Suppl 1), S61–S67 (2015).
Rommens, P. M. et al. Fragility fractures of the pelvis: Should they be fixed?. Acta Chir Orthop. Traumatol. Cech. 82(2), 101–112 (2015).
Rommens, P. M., Wagner, D. & Hofmann, A. Surgical management of osteoporotic pelvic fractures: A new challenge. Eur. J. Trauma. Emerg. Surg. 38(5), 499–509 (2012).
Rommens, P. M. & Hofmann, A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury 44(12), 1733–1744 (2013).
Winkelhagen, J. et al. Preliminary results of cannulated screw fixation for isolated pubic ramus fractures. Strategies Trauma Limb Reconstr. 7(2), 87–91 (2012).
Sullivan, M. P. et al. Geriatric fractures about the hip: divergent patterns in the proximal femur, acetabulum, and pelvis. Orthopedics 37(3), 151–157 (2014).
Kannus, P. et al. Low-trauma pelvic fractures in elderly Finns in 1970–2013. Calcif. Tissue Int. 97(6), 577–580 (2015).
Andrich, S. et al. Epidemiology of pelvic fractures in Germany: Considerably high incidence rates among older people. PLoS ONE 10(9), e0139078 (2015).
Breuil, V. et al. Outcome of osteoporotic pelvic fractures: An underestimated severity: Survey of 60 cases. Jt. Bone Spine 75(5), 585–588 (2008).
Acklin, Y. P. et al. Are two retrograde 3.5 mm screws superior to one 7.3 mm screw for anterior pelvic ring fixation in bones with low bone mineral density?. Bone Joint Res. 6(1), 8–13 (2017).
Acklin, Y. P. et al. Biomechanical comparison of plate and screw fixation in anterior pelvic ring fractures with low bone mineral density. Injury 47(7), 1456–1460 (2016).
Wojahn, R. D. & Gardner, M. J. Fixation of anterior pelvic ring injuries. J. Am. Acad. Orthop. Surg. 27(18), 667–676 (2019).
Stevenson, A. J., Swartman, B. & Bucknill, A. T. Percutaneous internal fixation of pelvic fractures. Unfallchirurg 120(Suppl 1), 10–18 (2017).
Suzuki, T. et al. Anatomic study for pubic medullary screw insertion. J. Orthop. Surg. (Hong Kong) 16(3), 321–325 (2008).
Chen, K. N. et al. Differences of percutaneous retrograde screw fixation of anterior column acetabular fractures between male and female: A study of 164 virtual three-dimensional models. Injury 40(10), 1067–1072 (2009).
Gansslen, A. & Krettek, C. Retrograde transpubic screw fixation of transpubic instabilities. Oper. Orthop. Traumatol. 18(4), 330–340 (2006).
Starr, A. J. et al. Superior pubic ramus fractures fixed with percutaneous screws: What predicts fixation failure?. J. Orthop. Trauma 22(2), 81–87 (2008).
Arand, C. et al. 3D statistical model of the pelvic ring—A CT-based statistical evaluation of anatomical variation. J. Anat. 234(3), 376–383 (2019).
Quercetti, N. 3rd. et al. Gun barrel view of the anterior pelvic ring for percutaneous anterior column or superior pubic ramus screw placement. Eur. J. Orthop. Surg. Traumatol. 27(5), 695–704 (2017).
Gehweiler, D. et al. Computational anatomy of the dens axis evaluated by quantitative computed tomography: Implications for anterior screw fixation. J. Orthop. Res. 35(10), 2154–2163 (2017).
Lim Fat, D. et al. The Hounsfield value for cortical bone geometry in the proximal humerus—An in vitro study. Skelet. Radiol. 41(5), 557–568 (2012).
Aamodt, A. et al. Determination of Hounsfield value for CT-based design of custom femoral stems. J. Bone Joint Surg. Br. 81(1), 143–147 (1999).
Patrick, S. et al. Comparison of gray values of cone-beam computed tomography with hounsfield units of multislice computed tomography: An in vitro study. Indian J. Dent. Res. 28(1), 66–70 (2017).
Qoreishi, M., SeyyedHosseinzadeh, H. R. & Safdari, F. Clinical results of percutaneous fixation of pelvic and acetabular fractures: A minimally invasive internal fixation technique. Arch. Bone Jt. Surg. 7(3), 284–290 (2019).
Attias, N. et al. The use of a virtual three-dimensional model to evaluate the intraosseous space available for percutaneous screw fixation of acetabular fractures. J. Bone Jt. Surg. Br. 87(11), 1520–1523 (2005).
Puchwein, P. et al. Percutaneous fixation of acetabular fractures: computer-assisted determination of safe zones, angles and lengths for screw insertion. Arch. Orthop. Trauma Surg. 132(6), 805–811 (2012).
Simonian, P. T. et al. Internal fixation of the unstable anterior pelvic ring: A biomechanical comparison of standard plating techniques and the retrograde medullary superior pubic ramus screw. J. Orthop. Trauma 8(6), 476–482 (1994).
Osterhoff, G. et al. Antegrade versus retrograde screw fixation of anterior column acetabular fractures: A biomechanical in vitro study. Eur. J. Trauma Emerg. Surg. 29, 1–6 (2019).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
The study concept was developed by C.A., D.W., R.G.R., H.N., L.K. and P.M.R.. Data acquisition and processing was performed by H.N., L.K. and D.G.. Statistical analysis was done by C.A. and J.H. C.A. wrote the manuscript and prepared figures and tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arand, C., Wagner, D., Richards, R.G. et al. Anatomical evaluation of the transpubic screw corridor based on a 3D statistical model of the pelvic ring. Sci Rep 11, 16677 (2021). https://doi.org/10.1038/s41598-021-96219-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96219-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.