Abstract
There has been no long-term clinical follow-up data of survivors or victims of sudden cardiac death (SCD). The Taiwan multi-center sudden arrhythmia death syndrome follow-up and clinical study (TFS-SADS) is a collaborative multi-center study with median follow-up time 43 months. In this cohort, the clinical characteristics of these SADS patients were compared with those with ischemic heart disease (IHD). In this SCD cohort, around half (42%) were patients with IHD, which was different from Caucasian SCD cohorts. Among those with normal heart, most had Brugada syndrome (BrS). Compared to those with SADS, patients with IHD were older, more males and more comorbidities, more arrhythmic death, and lower left ventricular ejection fraction. In the long-term follow-up, patients with SADS had a better survival than those with IHD (p < 0.001). In the Cox regression analysis to identify the independent predictors of mortality, older age, lower LVEF, prior myocardial infarction and history of out-of-hospital cardiac arrest were associated with higher mortality and beta blocker use and idiopathic ventricular fibrillation or tachycardia (IVF/IVT) with a better survival during follow-up. History of prior MI was associated with more arrhythmic death. Several distinct features of SCD were found in the Asia–Pacific region, such as higher proportion of SADS, poorer prognosis of LQTS and better prognosis of IVF/IVT. Patients with SADS had a better survival than those with IHD. For those with SADS, patients with channelopathy had a better survival than those with cardiomyopathy.
Similar content being viewed by others
Introduction
Sudden cardiac death (SCD) describes an unexpected death from a cardiac cause within a short time period, generally less than 1 h from the onset of symptoms. SCD is one of the most common causes of death and a major and disastrous complication of cardiovascular diseases. SCD is often attributed to ventricular arrhythmia1,2,3,4. Several diseases linked to SCD have been reported5. In older populations, ischemic heart disease (IHD) which includes coronary artery disease (CAD) (chronic coronary artery obstruction) and myocardial infarction (MI) (acute coronary artery obstruction) account for the most majority of SCD5,6. However, in younger populations, SCD is usually caused by genetic diseases such as inherited arrhythmogenic cardiomyopathies including hypertrophic cardiomyopathy (HCMP), dilated cardiomyopathy (DCMP) and arrhythmogenic right ventricular cardiomyopathy (ARVC), and inherited cardiac ion channel diseases including Brugada syndrome (BrS), congenital long QT syndrome (LQTS), short QT syndrome (SQTS), catecholaminergic polymorphic ventricular tachycardia (CPVT) and idiopathic ventricular fibrillation or tachycardia (IVF/IVT). These inherited cardiac diseases predisposing to SCD are collectively known as sudden arrhythmia death syndromes (SADS)1,7,8,9,10.
Understanding the epidemiology and clinical characteristics of SCD and SADS allows the implementation of comprehensive and appropriate strategies for the prevention and treatment of SCD and SADS. The information of the long-term follow-up and outcomes of SCD and SADS victims is largely unknown, especially in the Asia–Pacific region. Whether the clinical characteristics of SCD due to IHD and those due to SADS are different is also unknown. The Taiwan SADS follow-up and clinical study (TFS-SADS) is a multi-center study that aims to collect comprehensive clinical data of SCD and SADS in Taiwan, which include disease entity, patient characteristics, long-term follow-up information and predictors of survival. In this study, we first described the data from the TFS-SADS, which provided the opportunity to look at and compare the clinical characteristics, long-term follow-up and outcome data of patients with different causes of SADS and SCD in the Asia–Pacific region.
Methods
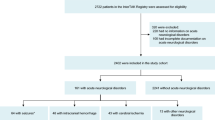
This was a multi-center retrospective cohort study monitoring patients of SCD and SADS in Taiwan. Victims or survivors of aborted SCD or SADS were enrolled in TFS-SADS from Jan. 2005 to Dec. 201611 with median follow-up time 43 months. The specific objectives of this TFS-SADS were to determine factors associated with SCD and to study the clinical characteristics and predictors of outcomes of SCD and compare them between groups of different causes of SCD (inherited SADS or IHD) in Taiwan. At the end of this study, a total of 730 patients were enrolled and all patients were followed by their individual physicians in cardiology out-patient clinics. The demographic data, baseline characteristics, primary cardiac diagnosis, use of antiarrhythmic drugs and other cardiovascular medications, report of coronary angiography, results of electrophysiological study, echocardiographic data including left ventricular ejection fraction (LVEF) and clinical outcomes were collected. The study was approved by the Institutional Review Board of the National Taiwan University Hospital (No. 201705122RINC and No. 202107079RINC), informed consent is waived by IRB. The majority of the patients (627/730, 85.9%) underwent implantable cardioverter defibrillator (ICD) implantation, and thus this patient population represented a high risk SADS or SCD population.
The diagnoses of BrS, LQTS, SQTS and CPVT were according to the continuously updated guidelines from American Heart Association/American College of Cardiology (AHA/ACC) and European Society of Cardiology (ESC)1,12,13. The diagnosis of HCMP, ARVC or DCMP was according to the criteria of cardiac imaging studies including echocardiography, cardiac computed tomography (CT) or magnetic resonance imaging (MRI)14,15,16,17. The presence of coronary artery disease was documented by coronary angiography with the presence of at least one coronary stenosis more than 70% of the luminal diameter. The primary outcome was all-cause death. The secondary outcome was cardiovascular death which included arrhythmic and heart failure death. Arrhythmic death was defined as sudden death with witnessed or ICD-interrogated ventricular arrhythmia1. Heart failure death was defined as cardiovascular death other than arrhythmic death, which was usually associated cardiac pumping or circulatory failure.
Statistical analysis
Continuous data were expressed as mean ± standard deviation (SD). The comparison was conducted by independent two-sample Student’s t-test for the continuous variables, and the chi-square test for the categorical variables. The cumulative mortalities or event rates were shown as survival curves in different groups by Kaplan–Meier method. The survival curves were compared using the log-rank test. The multivariable Cox proportional-hazards regression analysis was used to identify the predictors of survival, and hazard ratios (HRs) and their 95% confidence intervals (CIs) were calculated. The factors included in the multivariable model were those factors significant in the univariable analyses included age, gender, LVEF > 35%, Primary diagnosis (included prior MI, history of SCD), amiodarone or beta blocker use.
Survival analyses were also stratified by the presence or absence of IHD. In those SADS, the analysis was further stratified by the presence or absence of cardiomyopathy. All tests were two sided, and a significance value of p < 0.05 was used. All statistical analyses were carried out using the SPSS 23.0 (SPSS Inc. USA).
Ethics, consent and permissions
The study was approved by the Institutional Review Board of the National Taiwan University Hospital (No. 201705122RINC and No. 202107079RINC), informed consent is waived by IRB. This is a retrospective cohort and the delinked medical data were collected for analyses without consents from the participants.
Results
Baseline characteristics
Table 1 shows the primary diagnoses of all the enrolled patients. Among them, 42% (305/730) were patients with ischemic heart disease (IHD). This result was similar to our previous report that in the Asia–Pacific region, the proportion of SCD due to IHD was lower compared to that in the Caucasian populations in which nearly 80% of the SCD patients were due to IHD11,18,19.
For those patients with SCD not caused by IHD, the majority were caused by genetic diseases such as inherited arrhythmogenic cardiomyopathies or cardiac ion channel diseases (channelopathy). For comparison with those caused by IHD, they were collectively called as SADS in the present study. In those patients with non-IHD or SADS, around one third had normal structure heart and the other two thirds had cardiomyopathy (HCMP, ARVC and DCMP). Among all the SADS patients with normal structure heart, most of the patients had BrS, compatible with previous reports that BrS was the most common cause of SCD in patients with SCD and normal structure heart in the Asia–Pacific region20,21.
The comparison of clinical characteristics between those with IHD and SADS is shown in Table 2. Patients with IHD were older (66.1 vs. 51.3 year-old, p < 0.001) and had a male predominance (80% vs 68%, p = 0.001) and more comorbidities such as diabetes (34% vs 13%, p < 0.001), hyperlipidemia (40% vs 14%, p < 0.001), chronic kidney disease (38% vs 21%, p < 0.001), more death due to arrhythmia (3% vs 1%, p = 0.010) and heart failure (7% vs 4%, p = 0.043), higher mortality (22% vs 7%, p < 0.001), more use of amiodarone (58% vs 30%, p < 0.001) and poorer LVEF (43% vs 55%, p < 0.001). In patients with SADS, the comparison of clinical characteristics between patients with cardiomyopathy and those with normal structure heart patients is shown in Table 3. Patients with cardiomyopathy were older and more of them had chronic kidney disease and death due to heart failure, and had a poor left heart ejection fraction. So, those SADS patients with a normal heart were younger, and could be considered as the population of SCD in the young.
Among these SCD victims, 85.9% (n = 627) of the patients received ICD implantation, but not all of the patients, because the majority of indication of ICD implantation was a secondary prevention because of the national health insurance reimbursement policy.
Long-term follow up of patients with SCD
This is a long-term follow-up study of SADS population. We have the opportunity to compare the outcome of patients with different etiologies of SCD, e.g., comparing the outcome of patients with IHD and that of those with hereditary cardiac diseases or SADS.
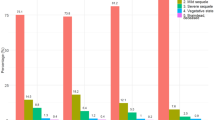
We first compared the long-term survivals of patients with non IHD or SADS and those with IHD and the result is shown in Fig. 1. In general, those with SADS had a better survival than those with IHD (p < 0.001).
We then compared the survivals of all the patients according to the primary diagnosis and the result is shown in Fig. 2. Interestingly, the survivals of patients with different etiologies of SCD were significantly different from one another (p < 0.001). Between different etiologies of SCD, patients with prior MI, DCMP and LQTS had the worst outcome (p < 0.001 for those with MI or DCMP or LQTS vs. others). The patients with LQTS had a poorer survival as those with prior MI or DCMP, although they had a normal heart.
Among those patients with hereditary cardiac diseases or SADS (channelopathy and cardiomyopathy), we found patients with IVF/IVT had the most favorable outcome (Supplementary Fig. S1) (p = 0.007). Again, patients with DCMP and LQTS had the least favorable outcome (Supplementary Fig. S2) (p = 0.015). We further dichotomized those SADS patients into those with a normal heart (channelopathy) and those with cardiomyopathy (HCMP, ARVC and DCMP) and compared the long-term survivals of these two groups (Supplementary Fig. 3). We found a significant difference of survival between these two groups. SADS patients with cardiomyopathy had a poorer survival than those with normal heart (p = 0.001).
Independent predictors of long-term survivals for patients with SCD
We first used multivariable Cox regression analysis to investigate the independent predictors of mortality for patients with SCD. For the entire study population, we found older age, lower LVEF, history of prior MI and history of out-of-hospital cardiac arrest (OHCA) (borderline statistically significant) were associated with higher mortality during follow-up (HR 2.565 [95% CI 1.679–3.920], p < 0.001; HR 0.592 [95% CI 0.386–0.906], p = 0.016; HR 1.827 [95% CI 1.163–2.870], p = 0.009; HR 1.523 [95% CI 0.996–2.327], p = 0.052). Patients with IVF/IVT had a better survival (Hazard ratio (HR) 0.137 [95% CI 0.019–1.004], p = 0.050).
Interestingly, we also found beta blocker use was also associated with a better survival (Hazard ratio (HR) 0.614 [95% CI 0.407–0.926], p = 0.020). To identify specific populations which might benefit from beta blocker use. We did analyses in subgroups. As expected, for those patients with IHD, use of beta blocker was associated with a better outcome (HR 0.621, p = 0.056) (Fig. 3), but only borderline statistically significant. However, use of beta blocker was not associated with a better outcome for those SADS patients (HR 0.602, p = 0.180) (Fig. 4).
We also used multivariable Cox regression analysis to investigate the independent predictors of mortality for patients with hereditary cardiac diseases or SADS (channelopathy and cardiomyopathy). We found older age and lower LVEF were associated with higher mortality during follow-up (HR 3.472 [95% CI 1.566–7.695], p = 0.002 for age > 65 years, and HR 2.315 [95% CI 1.025–5.208], p = 0.043 for LVEF < 35%, respectively).
Because these patients were susceptible to ventricular arrhythmia, we also looked at the predictors of death due to ventricular arrhythmia. Among the total of 730 patients at the end of follow-up, 13 were died of arrhythmic death. We found history of prior MI was the only independent predictor of arrhythmic death (HR 3.778 [95% CI 1.270–11.243], p = 0.017) (Supplement Table S1). Age older than 65 years and LQTS were also associated with arrhythmic death with borderline significant p values (HR 3.046 [95% CI 0.996–9.316, p = 0.051 and HR 3.877 [95% CI 0.858–17.509], p = 0.078, respectively] (Supplement Table S1).
Discussion
This is the first long-term follow-up study of SCD victims and also the first follow-up study of SADS victims in the Asia–Pacific region. So far the demographics, clinical features and long-term outcome of SADS or SCD have not been well characterized in the Asia–Pacific region. We identified several predictors of survival for patients with SCD or SADSs. These results may provide useful information in risk stratification.
Most of the previous SCD studies are cross-sectional and focused on postmortem examination22,23,24,25,26. Here we first described the clinical characteristics and follow-up information of survivors and victims of SADS or SCD in the Asia–Pacific region. The study on survivors or victims of SCD provides additional information regarding the future care of these patients, but not only the information about the distribution or percentage of various causes of SADS as revealed in previous cross-sectional studies22,23,24,25,26.
Etiology of SCD in the Asia–Pacific region and comparison with those of Caucasian population
Several distinct clinical features have been found in the survivors and victims of SCD in the present study, compared to those of the Caucasian populations. In our Asian SCD population, 37% (156/425) of them are BrS or normal heart, the percentage of which is higher compared to that of Caucasian SCD populations27,28. LQTS or CPVT is less common. Previously we had shown that the percentage of IHD was lowered in our SCD population, compared to that of Caucasian populations11,27,28. In this expanded population with a longer follow-up, we still had a similar finding.
This phenomenon may reflect different incidences of SCD in patients with IHD in different ethnic populations. It has been reported that the incidence of coronary deaths occurring outside of the hospital or in emergency rooms was lower in western populations29. Furthermore, in a survey of sudden death of adults in Japan in 1996, sudden death due to IHD was more in Western countries than in Japan30. Therefore, it is possible that the lower percentage of IHD in the present SCD population may represent a lower incidence of SCD in patients with IHD in the Asia–Pacific region.
In the patients with normal heart, in addition to BrS, there was also a higher proportion of patients with IVF or IVT. We believe that some of them might have Brugada syndrome or CPVT since resting or even provocative ECG of these two syndromes might be normal and challenges exist for a definite diagnosis. In this scenario, genetic test may help. However, the rate of sodium channel mutation (SCN5A) mutation is low in Asian patients with BrS31,32 and the rate of background mutations in ryanodine receptor 2 gene (RYR2) or calsequestrin 2 gene (CASQ2) are substantially high33, which sometimes make the definite diagnosis of BrS and CPVT even more difficult. Finally, a similar result has been reported that the percentage of IVF or IVT was as high as up to 44.1% in a survey of unexplained sudden cardiac death in Korea34. Therefore, it is still possible that the percentage of IVF or IVT is higher among the causes of SCD in the Asian populations.
Predictors of long-term survival for SADS patients
Our study also reveals several unique predictors of survival in the long-term follow-up of SADS or SCD victims, which has never been reported before. More care should be given and more frequent follow-up should be delivered to those with risk factors of mortality. The information of predictor of survival or mortality also provides the opportunity of early warning and explanation to the families and possibly a stronger persuasion of a genetic test for the at-risk family members.
As expected, for the entire SCD population, older age, history of MI and lower LVEF were associated with higher mortality. Use of beta blocker was associated with a better survival. In the subgroup analysis, use of beta blocker was associated with a better survival in those with IHD but not in those with non-IHD or SADS. However, it has been shown that use of beta blocker prolonged the survivals of patients with DCMP, HCMP or LQTS35,36,37,38,39. In our SADS population, patients with BrS and IVF accounted for a significant proportion of the population, who may not benefit from use of beta blocker. This may explain why use of beta blocker was not associated with a better survival in our SADS population.
Our study also first shows that patients with SADS had a better survival than those with IHD. And, in those with SADS, patients with a normal heart had a better survival than those with cardiomyopathy, in which those with DCMP had the worst outcome. The reason is straightforward, since patients with IHD or DCMP were generally older and had poorer LV function, and more comorbidities such as hypertension, diabetes or hyperlipidemia. Furthermore, even though a great progress in the technology of percutaneous coronary intervention, the mortality of patients with IHD, especially those with impaired left ventricular systolic function still keeps in a constantly high level40. And, for those with DCMP, in addition to susceptibility to SCD, they might also develop progressive deterioration of cardiac function, which might increase the incidence of both cardiac and non-cardiac deaths. Finally, the better survival of SADS patients with a normal heart indicates that SADS with a normal heart is a treatable disease if early prevention and treatment with ICD are given to those at-risk patients.
Our study also provides the opportunity to specifically look at and compare the survivals of patients with each different cause of SCD. Patients with history of MI, DCMP and LQTS had the worst outcome and patients with IVF or IVT had the best outcome. The long-term survival rate of LQTS was as low as those with DCMP or those with a prior MI, which was really out of expectation and has never been reported before. In the Caucasian registry, it has been reported that LQTS was a potentially lethal cardiac channelopathy with a 1% to 5% annual risk of LQTS-triggered syncope, aborted cardiac arrest, or sudden cardiac death41. Although the case number is not high in the present study, we first show that the annual rate of mortality was around 5% for the Asian LQTS patients, which reached the the upper limit of the reported SCD rate (1–5%). The percentage of beta blocker use was similar in our LQTS population (50%) compared to that reported in the Caucasian population (58%)41 and it is not likely that the high rate of mortality in our LQTS patients is due to low rate of beta blocker use.
LQTS is rare in the Asia–Pacific region. Therefore, most of the LQTS patients were recognized by the presentation of aborted SCD and therefore most of them are symptomatic and the treatment with ICD is based on a secondary prevention attempt. In the Caucasian LQTS registry41, symptomatic patients accounted for only 25% of the total study population. That may be the reason why the prognosis of LQTS may be poorer in the Asian LQTS registry since most recruited LQTS patients are symptomatic or have a history of aborted SCD.
Arrhythmia death despite ICD treatment represents a devastating medical condition in which although there is ICD shock treatment, the patients still die due to refractory heart failure, respiratory failure or failure to convert to sinus rhythm42. This population represents the non-ICD treatable and most dangerous population and needs more attention. Our study first identified the risk factors of arrhythmia death in the SCD survivors. We found patients with history of MI, older age and LQTS were probably more susceptible to arrhythmic death. Therefore, the follow-up and treatment should be more scrutinized in these patients, such as more frequent ICD interrogation to detect non-sustained ventricular arrhythmia, more aggressive medical treatment or higher dose of beta blocker, and avoid drugs that predispose to ventricular arrhythmia (class I anti-arrhythmic drugs)1,13,18. For those with prior MI and history of SCD or ventricular arrhythmia, early and more frequent stress test to detect subtle myocardial ischemia, institution of early coronary intervention, and more intensive statin treatment may be warranted43,44,45.
Conclusions
Several distinct features of SCD were found in the Asia–Pacific region, such as higher proportion of SADS, poorer prognosis of LQTS and better prognosis of IVF/IVT. Patients with SADS had a better survival than those with IHD. For those with SADS, patients with channelopathy had a better survival than those with cardiomyopathy.
Statement
All methods were carried out in accordance with relevant guidelines and regulations.
Limitations
Our study has limitations. First, because of the high screen rate of echocardiography and ECG in our pediatric patients, SCD due to congenital heart disease and Wolf-Parkinson-White syndrome are absent in our SADS population. Second, the case numbers of some diseases, especially channelopathy such as LQTS, CPVT and SQTS are relatively low and a higher power of statistical analysis could only be obtained by joint analyses.
Abbreviations
- ARVC:
-
Arrhythmogenic right ventricular cardiomyopathy
- BrS:
-
Brugada syndrome
- CAD:
-
Coronary artery disease
- CPVT:
-
Catecholaminergic polymorphic ventricular tachycardia
- CT:
-
Computed tomography
- DCMP:
-
Dilated cardiomyopathy
- HCMP:
-
Hypertrophic cardiomyopathy
- HR:
-
Hazard ratio
- ICD:
-
Implantable cardioverter-defibrillator
- IHD:
-
Ischemic heart disease
- IVF/VT:
-
Idiopathic ventricular fibrillation or tachycardia
- LVEF:
-
Left ventricular ejection fraction
- LQTS:
-
Long QT syndrome
- MI:
-
Myocardial infarction
- MRI:
-
Magnetic resonance imaging
- OHCA:
-
Out of hospital cardiac arrest
- SADS:
-
Sudden arrhythmia death syndromes
- SCD:
-
Sudden cardiac death
- SD:
-
Standard deviation
- SQTS:
-
Short QT syndrome
- TFS-SADS:
-
Taiwan sudden arrhythmia death syndrome study
- VT:
-
Ventricular tachycardia
- VF:
-
Ventricular fibrillation
References
Priori, S. G. et al. ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur. Heart J. 36, 2793–2867 (2015).
Koplan, B. A. & Stevenson, W. G. Ventricular tachycardia and sudden cardiac death. Mayo Clin. Proc. 84, 289–297 (2009).
John, R. M. et al. Ventricular arrhythmias and sudden cardiac death. Lancet (London, England) 380, 1520–1529 (2012).
Al-Khatib, S. M. et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 72, e91–e220 (2018).
Srinivasan, N. T. & Schilling, R. J. Sudden cardiac death and arrhythmias. Arrhythmia Electrophysiol. Rev. 7, 111–117 (2018).
Zipes, D. P. & Wellens, H. J. Sudden cardiac death. Circulation 98, 2334–2351 (1998).
Koplan, B. A. & Stevenson, W. G. Sudden arrhythmic death syndrome. Heart 93, 547–548 (2007).
Bezzina, C. R., Lahrouchi, N. & Priori, S. G. Genetics of sudden cardiac death. Circ. Res. 116, 1919–1936 (2015).
Refaat, M. M., Hotait, M. & London, B. Genetics of sudden cardiac death. Curr. Cardiol. Rep. 17, 606 (2015).
Mak, C. M. et al. Sudden arrhythmia death syndrome in young victims: A five-year retrospective review and two-year prospective molecular autopsy study by next-generation sequencing and clinical evaluation of their first-degree relatives. Hong Kong Med. J. = Xianggang yi xue za zhi 25, 21–29 (2019).
Tsai, C. T., Huang, S. K., Lin, J. L. & Lai, L. P. Distinct clinical features in the recipients of the implantable cardioverter defibrillator in Taiwan: A multicenter registry study. Pacing Clin. Electrophysiol. 26, 2083–2090 (2003).
Priori, S. G. et al. Executive summary: HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. Heart Rhythm 10, e85-108 (2013).
Pedersen, C. T. et al. EHRA/HRS/APHRS expert consensus on ventricular arrhythmias. Heart Rhythm 11, e166–e196 (2014).
Marcus, F. I. et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: Proposed modification of the Task Force Criteria. Eur. Heart J. 31, 806–814 (2010).
Elliott, P. M. et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 35, 2733–2779 (2014).
Bozkurt, B. et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: A scientific statement from the American Heart Association. Circulation 134, e579–e646 (2016).
Mathew, T. et al. Diagnosis and assessment of dilated cardiomyopathy: A guideline protocol from the British Society of Echocardiography. Echo Res. Pract. 4, G1-g13 (2017).
Caputo, M. L. et al. Temporal trends and long term follow-up of implantable cardioverter defibrillator therapy for secondary prevention: A 15-year single-centre experience. Int. J. Cardiol. 228, 31–36 (2017).
Chen, T. E., Wang, C. C., Chang, S. H., Yeh, S. J. & Wu, D. Implantable cardioverter defibrillator therapy: Ten years experience in a medical center. Chang Gung Med. J. 31, 81–90 (2008).
Hiraoka, M. Brugada syndrome in Japan. Circ. J. 71, A61–A68 (2007).
Kamakura, S. Epidemiology of Brugada syndrome in Japan and rest of the world. J. Arrhythmia 29, 52–55 (2013).
Veerakul, G. & Nademanee, K. What is the sudden death syndrome in Southeast Asian males?. Cardiol. Rev. 8, 90–95 (2000).
Mellor, G. et al. Clinical characteristics and circumstances of death in the sudden arrhythmic death syndrome. Circ. Arrhythm. Electrophysiol. 7, 1078–1083 (2014).
Risgaard, B. Sudden cardiac death: A nationwide cohort study among the young. Dan. Med. J. 63, B5321 (2016).
Lewis, M. E. et al. Estimated incidence and risk factors of sudden unexpected death. Open Heart 3, e00321 (2016).
Hai, J. J. et al. Incidence and predictors of sudden arrhythmic death or ventricular tachyarrhythmias after acute coronary syndrome: An Asian perspective. Heart Rhythm 14, 81–87 (2017).
Connolly, S. J. et al. Canadian implantable defibrillator study (CIDS): A randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation 101, 1297–1302 (2000).
Investigators Tavida. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N. Engl. J. Med. 337, 1576–1583 (1997).
Gillum, R. F. Sudden cardiac death in Hispanic Americans and African Americans. Am. J. Public Health 87, 1461–1466 (1997).
Toyoshima, H. et al. Sudden death of adults in Japan. Nagoya J. Med. Sci. 59, 81–95 (1996).
Juang, J. M. et al. Unique clinical characteristics and SCN5A mutations in patients with Brugada syndrome in Taiwan. J. Formosan Med. Assoc. = Taiwan yi zhi 114, 620–626 (2015).
Tan, B. Y. et al. A Brugada syndrome proband with compound heterozygote SCN5A mutations identified from a Chinese family in Singapore. Europace 18, 897–904 (2016).
Landstrom, A. P. et al. Interpreting incidentally identified variants in genes associated with catecholaminergic polymorphic ventricular tachycardia in a large cohort of clinical whole-exome genetic test referrals. Circ. Arrhythmia Electrophysiol. 10, e004742 (2017).
Cho, J. G. et al. Clinical characteristics of unexplained sudden cardiac death in Korea. Jpn. Circ. J. 65, 18–22 (2001).
Hamada, M., Ikeda, S. & Shigematsu, Y. Advances in medical treatment of hypertrophic cardiomyopathy. J Cardiol 64, 1–10 (2014).
Weintraub, R. G., Semsarian, C. & Macdonald, P. Dilated cardiomyopathy. Lancet (London, England) 390, 400–414 (2017).
Ahn, J. et al. Effectiveness of beta-blockers depending on the genotype of congenital long-QT syndrome: A meta-analysis. PLoS ONE 12, e0185680 (2017).
Andries, G., Yandrapalli, S., Naidu, S. S. & Panza, J. A. Novel pharmacotherapy in hypertrophic cardiomyopathy. Cardiol. Rev. 26, 239–244 (2018).
Steinberg, C. Diagnosis and clinical management of long-QT syndrome. Curr. Opin. Cardiol. 33, 31–41 (2018).
Vedin, O. et al. Significance of ischemic heart disease in patients with heart failure and preserved, midrange, and reduced ejection fraction: A Nationwide cohort study. Circ. Heart Fail. 10, e003875 (2017).
Rohatgi, R. K. et al. Contemporary outcomes in patients with long QT syndrome. J. Am. Coll. Cardiol. 70, 453–462 (2017).
Aleong, R. G. & Sauer, W. H. Paradox of appropriate implantable cardioverter-defibrillator therapy: Saving lives but revealing an increased mortality risk. J. Am. Heart Assoc. 6, e007087 (2017).
Voss, F. et al. Safety of symptom-limited exercise testing in a big cohort of a modern ICD population. Clin. Res. Cardiol. 105, 53–58 (2016).
Chinnaiyan, K. M., Trivax, J., Franklin, B. A., Williamson, B. & Kahn, J. K. Stress testing in patients with implantable cardioverter-defibrillators: A preliminary report. Prev. Cardiol. 10, 92–95 (2007).
Bloom, H. L. et al. Statins decrease oxidative stress and ICD therapies. Cardiol. Res. Pract. 2010, 253803 (2010).
Acknowledgements
The work was supported by grant from the Ministry of Science and Technology (MOST) in Taiwan [110-2134-B-002-234]. The authors would like to express their thanks to the staff of Department of Medical Research for providing clinical data from National Taiwan University Hospital-integrated Medical Database (NTUH-iMD).
Author information
Authors and Affiliations
Contributions
P.S.H.: study design, analyses, conducting and manuscript preparation. J.F.C.: study design, analyses, W.C.K.: study design S.H.C.: study design. T.T.L.: study design. J.J.C.: analyses. F.C.C.: analyses. L.Y.L.: study design, analyses. L.P.L.: study design. J.L.L.: study design, planning. C.T.T.: study design, analyses, manuscript preparation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, PS., Cheng, JF., Ko, WC. et al. Unique clinical features and long term follow up of survivors of sudden cardiac death in an Asian multicenter study. Sci Rep 11, 18250 (2021). https://doi.org/10.1038/s41598-021-95975-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-95975-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.