Abstract
To assess the effect from individual component in combinations of steroid, ascorbic acid, and thiamine on outcomes in adults with sepsis and septic shock with component network meta-analysis (NMA). We searched PubMed, EMBASE, and the Cochrane Library Central Register of Controlled Trials from 1980 to March 2021 for randomized controlled trials (RCT) that studied the use of glucocorticoid, fludrocortisone, ascorbic acid, and thiamine in patients with sepsis and septic shock. Citations screening, study selection, data extraction, and risk of bias assessment were independently performed by two authors. The primary outcome was short-term mortality. Secondary outcomes were longer-term mortality, time to resolution of shock and duration of mechanical ventilation. Thirty-three RCTs including 9898 patients presented on short-term mortality. In additive component NMA, patients on ascorbic acid alone (RR 0.74, 95% CI 0.57–0.97) or the combination of glucocorticoid and fludrocortisone (RR 0.89, 95% CI 0.80–0.99) had lower short-term mortality, but only the latter was associated with improved long-term mortality (RR 0.89, 95% CI 0.82–0.98). The use of glucocorticoid or the combination of glucocorticoid, ascorbic acid and thiamine hastened resolution of shock. Component NMA showed glucocorticoid (MD − 0.96, 95% CI − 1.61 to − 0.30) but not ascorbic acid or thiamine shortened the time to resolution of shock. Glucocorticoid shortened the duration of mechanical ventilation (MD − 1.48, 95% CI − 2.43 to − 0.52). In adults with sepsis and septic shock, the combination of glucocorticoid and fludrocortisone improved short-term and longer-term mortality. Glucocorticoid shortened the time to resolution of shock and duration of mechanical ventilation. There was no strong evidence supporting the routine use of thiamine and ascorbic acid, but they were associated with minimal adverse effects.
Similar content being viewed by others
Introduction
Multiple studies have shown the value of steroid in sepsis and septic shock in terms of hastening the shock reversal1,2,3,4. Since the publication of the before-after study by Marikl et al., the addition of ascorbic acid and thiamine to hydrocortisone has drawn much attention in the field5. Subsequent randomized controlled trials on the use of this triple therapy yielded conflicting results. Furthermore, there was only one study comparing hydrocortisone alone with the triple therapy6. Therefore the optimal treatment agent or combinations in patients with sepsis and septic shock remains unclear.
Network meta-analysis (NMA) calculates the combination of direct and indirect estimates of effects and allows comparison of multiple intervention with improved precision. The model was further improved by Welton et al. who proposed the component network meta-analysis (CNMA) in 2009 for multicomponent interventions7. CNMA considers separate effect for each of the different component in an intervention8. As a relatively new methodology, CNMA has started to gain its acceptance in the medical community but largely limited in the field of psychiatry7,9,10,11. The aim of this systematic review and NMA/CNMA was to evaluate the use of steroids (including glucocorticoid and fludrocortisone), ascorbic acid, and thiamine in adult patients with sepsis and septic shock.
Methods
We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension statement for reporting network meta-analyses (PRIMSA-NMA) (Supplementary material Table 1). 12 The protocol for this review was registered in the International Prospective Register of Systematic Reviews (CRD42020216665).
Data sources and searches
We searched PubMed, EMBASE, and the Cochrane Library Central Register of Controlled Trials from 1980 to March 2021 for potentially relevant studies published in English. Our PubMed search strategy is presented in Supplementary Material Table 2. Reference lists of the relevant articles, conference proceedings, and systematic reviews were also reviewed. We included randomized controlled trials (RCT) of adult patients with sepsis and septic shock investigating the use of glucocorticoid (including hydrocortisone, dexamethasone, and methylprednisolone), fludrocortisone, ascorbic acid and thiamine. Sepsis and septic shock were defined by the individual authors in the included studies. We excluded studies comparing the methods of administration (e.g. bolus vs. infusion) of steroid. We excluded studies enrolling healthy volunteers or animals and studies which excluded patients with septic shock.
Study selection and data extraction
Two authors (KF and SA) independently screened citations and abstracts in duplicate and independently. All references judged potentially relevant were evaluated for full-text eligibility. Discrepancies were solved by consensus with the third author (GN). When relevant data or information were missing, we attempted to contact the authors of the studies.
Outcome measures
The primary outcome was the short-term mortality (< 90 days). The secondary outcomes were longer term mortality (≥ 90 days), time to resolution of shock and duration of mechanical ventilation. Tertiary outcomes included the ICU length of stay, hospital length of stay and adverse events (including secondary infections, gastrointestinal bleeding, delirium, hyperglycemia, hypernatremia, and any potential complications related to ascorbic acid and thiamine).
Risk of bias assessment
Two authors (SA and GN) independently assessed the risk of bias of included studies. We assessed the risk of bias of the RCT using the revised Cochrane risk-of-bias tool for randomized trials13. In case of disagreement for the attribution of risk of bias, it was solved by discussion and consensus with the third author (KF).
Statistical analysis and quality of evidence
We performed a random effect NMA and additive CNMA using a frequentist framework. Additive CNMA allows each component to have it separate effect thus the total effect of an intervention is equal to the sum of individual component effect9. We calculated the mean differences (MD) for continuous outcomes and risk ratios (RR) for dichotomous outcomes. Where data were not available, we converted the median and interquartile range to mean and standard deviations using a published equation14. We also ranked the treatment using the P-score which was based on the frequentist point estimates and their standard errors15. We assessed the assumption of transitivity by comparing the distribution effect modifier across studies. Potential inconsistency in the random effect model was assessed by node-splitting method design-by-treatment model16. Publication bias was investigated using the Egger’s test and comparison-adjusted funnel plots. We performed sensitivity analysis by limiting to 3 categories: (1) studies with low risk of bias, (2) studies recruiting > 50% of patients dependent on inotrope/ vasopressor (because of the difference in the proportion of patients with septic shock across studies), (3) studies recruiting patients after 2016 (because of the major practice change after the publication of the 2016 Surviving Sepsis Campaign)17. Lastly, (3) we also performed sensitivity analysis by excluding studies using high dose glucocorticoid (≥ 400 mg/day hydrocortisone or equivalent, according to previous literature18). Since the dose of glucocorticoid were weight-based in some studies1,2,19,20,21,22,23, the dose would be calculated based on a 60 kg man in the analysis. The NMA was performed using the package ‘netmeta’ (version 1.3–0) in R (version 4.0.3, The R Foundation for Statistical Computing).
We applied the modified Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach for network meta-analysis24,25. The contributions of all direct estimates to the network estimates were evaluated from the contribution matrix26. We rated down the quality of evidence when intransitivity was present, or when there was incoherence between direct and indirect estimates. When both direct and indirect evidence were available, we chose the higher of the two quality ratings for the NMA estimate24.
Results
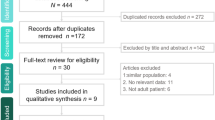
Literature search
The initial search yielded 2563 citations; 69 proved potentially eligible after reviewing the full-text articles. Thirty-four studies met our inclusion criteria, representing 9,992 patients (Supplemental Information Fig. 1). The characteristics of the included studies are shown in Supplemental Information Table 3. Trial sample size ranged from 27 to 3713. Results of the individual studies can be found in Supplemental Information Table 4 to Table 14.
Risk of bias and quality of evidence
There were 12 studies adjudicated at low risk of bias in all domains. The summary of risk of bias assessment is shown in Supplemental Information Fig. 2.
Assessment of transitivity and inconsistency
Supplemental Information Table 15 shows the important trial and patient characteristics (Dosage of glucocorticoid, age, APACHE II, percentage of vasopressor/ inotrope dependence at baseline) across treatment comparisons for assessment of transitivity. On visual inspection the dosage of glucocorticoid, age, and APACHE II appeared similarly distributed across comparisons, although there was missing information. However, 2 out of 34 studies recruited less than 50% of patients dependent on vasopressors/ inotropes at baseline. Otherwise, the assumption of transitivity appeared to be valid. There was no significant incoherence detected by statistical testing nor visual inspection of direct and indirect estimates (Supplemental Information Table 16).
Primary outcome
Thirty-three studies representing 9,898 patients reported the short-term mortality (< 90 days)1,2,3,4,6,19,20,21,22,23,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49. The network geometry is shown in Supplemental Information Fig. 3. Patients on ascorbic acid alone, or the combination of glucocorticoid plus ascorbic acid, or the combination of glucocorticoid and fludrocortisone had lower short-term mortality (Fig. 1). Forest plot for components showed the use of ascorbic acid was associated with lower short-term mortality (Supplementary Fig. 4). There was no evidence of statistical heterogeneity (τ2 = 0, p = 927). The designment-by-treatment interaction model and node-splitting method did not detect any inconsistencies (Supplemental Information Table 17). There was no evidence of publication bias based on the funnel plot and Egger’s test (Supplemental Information Fig. 5).
Secondary outcomes
Longer term mortality
Seven studies including 6,322 patients presented the longer-term mortality (≥ 90 days)1,3,28,36,37,45,49. The network geometry is shown in Supplemental Information Fig. 6. The combination of glucocorticoid and fludrocortisone was associated with increased longer-term mortality compared with placebo (RR 0.89, 95% CI 0.82–0.98) (Supplemental Information Fig. 7). There was no statistically significant difference of individual components compared with placebo in reducing longer-term mortality (Supplementary Fig. 8).
Time to resolution of shock
Fourteen studies including 5063 patients presented the time to resolution of shock1,2,23,32,33,34,35,37,39,41,42,43,44,47. The network geometry is shown in Supplemental Information Fig. 9. Both glucocorticoid and the combination of glucocorticoid, ascorbic acid and thiamine shortened the time to resolution of shock compared with placebo (Fig. 2). Forest plot for components showed glucocorticoid shortened the time to resolution of shock with statistical significance (Supplemental Information Fig. 10) There was no evidence of publication bias (Supplemental Information Fig. 11).
Duration of mechanical ventilation
Based on the six studies which presented the duration of mechanical ventilation (network geometry as shown in Supplemental Information Fig. 12)2,33,34,37,45,47, patients on glucocorticoid had shorter duration of mechanical ventilation compared with placebo (Supplemental Information Fig. 13). Forest plot for components showed glucocorticoid shortened the duration of mechanical ventilation compared with placebo (Supplemental Information Fig. 14).
Tertiary outcomes
ICU and hospital length of stay
Network geometries on ICU and hospital stay were shown in Supplemental Information Fig. 15 and 16 respectively. There was no significant difference in ICU length of stay based on the data from 10 studies3,30,31,32,33,35,37,39,44,45 (Supplemental Information Fig. 17). Based on the 9 studies presenting hospital length of stay3,6,30,31,33,35,42,44,45, there was also no statistically significant difference in hospital length of stay (Supplemental Information Fig. 18) There was no evidence of publication bias in ICU length of stay (Supplementary Fig. 19).
Adverse events
The use of glucocorticoid or the combination of glucocorticoid and fludrocortisone was associated with increased risk of hyperglycemia. There was no difference in the incidence of secondary infections, gastrointestinal bleeding, delirium, and hypernatremia with the use of steroid as shown in the pooled data (Supplemental Information Fig. 20). One study reported the incidence of hypernatremia that was not amenable to statistical pooling, showing the lower risk of hypernatremia with hydrocortisone infusion compared with bolus injection50. Adverse events related to ascorbic acid or thiamine were uncommon (Supplemental Information Table 18).
Sensitivity analysis
Sensitivity analysis performed on short-term mortality limiting to studies adjudicated with low risk of bias3,4,6,30,33,34,36,37,38,40,45,49 (Supplemental Information Fig. 21) and studies recruiting > 75% patients dependent on inotrope/ vasopressor1,3,4,6,19,23,27,28,30,31,32,33,34,35,36,37,38,40,41,42,43,44,45,46,47 showed similar results (Supplemental Information Fig. 22). In the sensitivity analysis on studies recruiting patients after 20166,37,38,39,40,41,42,43,44,45,46,47,48,49, the use of ascorbic acid did not reach statistical significance in additive CNMA and there was no data on the use of glucocorticoid and fludrocortisone (Supplemental Information Fig. 23). Sensitivity analysis performed on studies excluding high-dose glucocorticoid (≥ 400 mg/day hydrocortisone or equivalent) showed similar results (Supplemental Information Fig. 24–26)1,3,4,6,23,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49. None of studies reporting longer term mortality used high dose corticosteroid so sensitivity analysis was omitted.
P-score statistics on primary and secondary outcomes
Table 1 shows the P-scores of each intervention on short-term mortality, longer-term mortality, and time to resolution of shock. Ascorbic acid was ranked as the best treatment for short term mortality, whereas glucocorticoid plus fludrocortisone was ranked the first for longer-term mortality. Glucocorticoid was ranked the best in hastening the resolution of shock.
Discussion
The results of this NMA of 34 RCT offered evidence summary regarding the use of steroid, ascorbic acid, and thiamine in adult patients with sepsis and septic shock. Over the years, the interest of the researchers on sepsis changed from high-dose corticosteroid alone, to low dose corticosteroid, and to combination with fludrocortisone, and then to various septic cocktails. There were limited trials with head-to-head comparisons. Worries about their potential complications might limit the choice among these septic adjuncts as well. Clinicians would be eager to know the effect of individual component from the septic cocktail and the clinical benefits of each combination therapy. In this NMA, we found that two interventions were associated with improved short-term mortality, namely ascorbic acid and the combination of glucocorticoid and fludrocortisone. Only the effect of the latter translated into improved longer- term mortality. Glucocorticoid shortened the time to resolution of shock and the duration of mechanical ventilation, but not the ICU or hospital length of stay. Complications arising from these interventions were uncommon except for hyperglycemia associated with steroid use.
This systematic review had a number of strengths. While there had been systematic reviews evaluating the use of steroids, or thiamine in patients with septic shock51,52, this systematic review looked at the use of steroids, ascorbic acid, and thiamine together as an NMA. This study went one step further to dismantle the effect from individual components among various combinations of steroids, and ascorbic acid by CNMA. Another strength of this study was the independent risk of bias assessment where the reviewers were not involved in any of the included trials. There was comprehensive literature search and adherence to the PRISMA-NMA guideline.
Obviously, this meta-analysis could not address all the unresolved issues in the use of these adjunct therapy in the management of septic shock and there are several limitations in this study. Drawing a conclusion in meta-analysis is dependent on the availability and quality of the exist trials. The very assumption underlying a meta-meta-analysis is transitivity. While we believed that the patient characteristics and the use of steroid were reasonably comparable among studies, the understanding of diseases, ICU management strategy and the definition of sepsis and septic shock have been changing over the last thirty plus years when the recruited studies have been conducted. Ideally there should be head-to-head comparison between hydrocortisone, ascorbic acid, thiamine, septic cocktail, and the combination of hydrocortisone plus fludrocortisone. However, in practice, with the existing evidence and established guideline supporting the use of hydrocortisone, conducting another randomized controlled trial with ascorbic acid alone or thiamine alone might be contrary to the principle of equipoise.
Despite the solid evidence on the use of glucocorticoid and fludrocortisone and a flourishing number of papers focusing the use of ‘septic cocktail’, guidelines on sepsis management such as the Surviving Sepsis Campaign have been slow to recognize the role of these agents. Since the publication of the two ‘positive’ trials form Annane28,36, no guidelines have been published to adopt such regimen. Based on the results from our NMA, the role of glucocorticoid and fludrocortisone should be re-emphasized, although further research is needed to clarify the role of glucocorticoid plus fludrocortisone in the era post-2016 Surviving Sepsis Campaign and its effect as compared with the septic cocktail. On the other hand, the results of the current NMA did not support the routine use of thiamine and ascorbic acid.
Conclusions
In adults with sepsis and septic shock, the combination of glucocorticoid and fludrocortisone improved short-term and longer-term mortality. Glucocorticoid shortened the time to resolution of shock and duration of mechanical ventilation but increased incidence of hyperglycemia. There was no strong evidence supporting the routine use of thiamine and ascorbic acid, but they were associated with minimal adverse effects.
Data availability
All data generated or analyzed during the present study are included in this published article and its supplementary information files.
References
Briegel, J. et al. Stress doses of hydrocortisone reverse hyperdynamic septic shock: A prospective, randomized, double-blind, single-center study. Crit. Care Med. 27(4), 723–732 (1999).
Cicarelli, D. D., Vieira, J. E. & Bensenor, F. E. Early dexamethasone treatment for septic shock patients: A prospective randomized clinical trial. Sao Paulo Med. J. 125(4), 237–241 (2007).
Sprung, C. L. et al. Hydrocortisone therapy for patients with septic shock. N. Engl. J. Med. 358(2), 111–124 (2008).
Gordon, A. C. et al. The interaction of vasopressin and corticosteroids in septic shock: A pilot randomized controlled trial. Crit. Care Med. 42(6), 1325–1333 (2014).
Marik, P. E., Khangoora, V., Rivera, R., Hooper, M. H. & Catravas, J. Hydrocortisone, vitamin C, and thiamine for the treatment of severe sepsis and septic shock: A retrospective before-after study. Chest 151(6), 1229–1238 (2017).
Fujii, T. et al. Effect of vitamin C, hydrocortisone, and thiamine vs hydrocortisone alone on time alive and free of vasopressor support among patients with septic shock: The VITAMINS randomized clinical trial. JAMA 323(5), 423–431 (2020).
Welton, N. J., Caldwell, D. M., Adamopoulos, E. & Vedhara, K. Mixed treatment comparison meta-analysis of complex interventions: Psychological interventions in coronary heart disease. Am. J. Epidemiol. 169(9), 1158–1165 (2009).
Rucker, G., Petropoulou, M. & Schwarzer, G. Network meta-analysis of multicomponent interventions. Biom. J. 62(3), 808–821 (2020).
Freeman, S. C. et al. Component network meta-analysis identifies the most effective components of psychological preparation for adults undergoing surgery under general anesthesia. J. Clin. Epidemiol. 98, 105–116 (2018).
Chu, C. S. et al. Cognitive effects and acceptability of non-invasive brain stimulation on Alzheimer’s disease and mild cognitive impairment: a component network meta-analysis. J. Neurol. Neurosurg. Psychiatry 92(2), 195–203 (2021).
Miklowitz, D. J. et al. Adjunctive psychotherapy for bipolar disorder: A systematic review and component network meta-analysis. JAMA Psychiat. 78(2), 141–150 (2021).
Hutton, B. et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann Intern Med. 162(11), 777–784 (2015).
Higgins, J. P. T. S. J., Savović, J., Page, M. J., Hróbjartsson, A., Boutron, I., Reeves, B. & Eldridge, S. A revised tool for assessing risk of bias in randomized trials. Cochrane database of systematic reviews. 10(Suppl 1), 297–31 (2016).
Wan, X., Wang, W., Liu, J. & Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 14, 135 (2014).
Rucker, G. & Schwarzer, G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med. Res. Methodol. 15, 58 (2015).
Higgins, J. P. et al. Consistency and inconsistency in network meta-analysis: Concepts and models for multi-arm studies. Res. Synth. Methods 3(2), 98–110 (2012).
Rhodes, A. et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 43(3), 304–377 (2017).
Gibbison, B. et al. Corticosteroids in septic shock: A systematic review and network meta-analysis. Crit. Care. 21(1), 78 (2017).
Sprung, C. L. et al. The effects of high-dose corticosteroids in patients with septic shock. A prospective, controlled study. N. Engl. J. Med. 311(18), 1137–1143 (1984).
Bone, R. C. et al. A controlled clinical trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 317(11), 653–658 (1987).
Luce, J. M. et al. Ineffectiveness of high-dose methylprednisolone in preventing parenchymal lung injury and improving mortality in patients with septic shock. Am. Rev. Respir. Dis. 138(1), 62–68 (1988).
Veterans Administration Systemic Sepsis Cooperative Study G. Effect of high-dose glucocorticoid therapy on mortality in patients with clinical signs of systemic sepsis. N. Engl. J. Med. 317(11), 659–665 (1987).
Oppert, M. et al. Low-dose hydrocortisone improves shock reversal and reduces cytokine levels in early hyperdynamic septic shock. Crit. Care Med. 33(11), 2457–2464 (2005).
Puhan, M. A. et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 349, g5630 (2014).
Balshem, H. et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 64(4), 401–406 (2011).
Salanti, G., Del Giovane, C., Chaimani, A., Caldwell, D. M. & Higgins, J. P. Evaluating the quality of evidence from a network meta-analysis. PLoS ONE 9(7), e99682 (2014).
Bollaert, P. E. et al. Reversal of late septic shock with supraphysiologic doses of hydrocortisone. Crit. Care Med. 26(4), 645–650 (1998).
Annane, D. et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 288(7), 862–871 (2002).
Meduri, G. U., Golden, E. & Umberger, R. Prospective double-blind randomized clinical trial on the effects of low-dose hydrocortisone infusion in patients with severe sepsis. Chest 136(4_MeetingAbstracts), 45S (2009).
Investigators, C. S. et al. Corticosteroid treatment and intensive insulin therapy for septic shock in adults: A randomized controlled trial. JAMA 303(4), 341–348 (2010).
Donnino, M. W. et al. Randomized, double-blind, placebo-controlled trial of thiamine as a metabolic resuscitator in septic shock: A pilot study. Crit. Care Med. 44(2), 360–367 (2016).
Zabet, M. H., Mohammadi, M., Ramezani, M. & Khalili, H. Effect of high-dose Ascorbic acid on vasopressor’s requirement in septic shock. J. Res. Pharm. Pract. 5(2), 94–100 (2016).
Gordon, A. C. et al. Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: The VANISH randomized clinical trial. JAMA 316(5), 509–518 (2016).
Tongyoo, S. et al. Hydrocortisone treatment in early sepsis-associated acute respiratory distress syndrome: Results of a randomized controlled trial. Crit. Care 20(1), 329 (2016).
Lv, Q. Q., Gu, X. H., Chen, Q. H., Yu, J. Q. & Zheng, R. Q. Early initiation of low-dose hydrocortisone treatment for septic shock in adults: A randomized clinical trial. Am. J. Emerg. Med. 35(12), 1810–1814 (2017).
Annane, D. et al. Hydrocortisone plus fludrocortisone for adults with septic shock. N. Engl. J. Med. 378(9), 809–818 (2018).
Venkatesh, B. et al. Adjunctive glucocorticoid therapy in patients with septic shock. N. Engl. J. Med. 378(9), 797–808 (2018).
Fowler, A. A. 3rd. et al. Effect of vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: The CITRIS-ALI randomized clinical trial. JAMA 322(13), 1261–1270 (2019).
Harun, N. F. et al. Intravenous thiamine as an adjuvant therapy for hyperlactatemia in septic shock patients. Crit. Care Shock 22, 288–298 (2019).
Moskowitz, A. et al. Effect of ascorbic acid, corticosteroids, and thiamine on organ injury in septic shock: The ACTS randomized clinical trial. JAMA 324(7), 642–650 (2020).
Iglesias, J. et al. Outcomes of metabolic resuscitation using ascorbic acid, thiamine, and glucocorticoids in the early treatment of sepsis: The ORANGES trial. Chest 158(1), 164–173 (2020).
Wani, S. J. et al. Combination of vitamin C, thiamine and hydrocortisone added to standard treatment in the management of sepsis: Results from an open label randomised controlled clinical trial and a review of the literature. Infect. Dis. (Lond.) 52(4), 271–278 (2020).
Reddy, P. R., Samavedam, S., Aluru, N., Yelle, S. & Rajyalakshmi, B. Metabolic resuscitation using hydrocortisone, ascorbic acid, and thiamine: Do individual components influence reversal of shock independently?. Indian J. Crit. Care Med. 24(8), 649–652 (2020).
Mohamed, Z. U. et al. Vitamin C therapy for routine care in septic shock (ViCTOR) trial: Effect of intravenous vitamin C, thiamine, and hydrocortisone administration on inpatient mortality among patients with septic shock. Indian J. Crit. Care Med. 24(8), 653–661 (2020).
Hwang, S. Y. et al. Combination therapy of vitamin C and thiamine for septic shock: A multi-centre, double-blinded randomized, controlled study. Intensive Care Med. 46(11), 2015–2025 (2020).
Petsakul, S. et al. Effects of thiamine on vasopressor requirements in patients with septic shock: A prospective randomized controlled trial. BMC Anesthesiol. 20(1), 280 (2020).
Chang, P. et al. Combined treatment with hydrocortisone, vitamin C, and thiamine for sepsis and septic shock: A randomized controlled trial. Chest 158(1), 174–182 (2020).
Aisa-Alvarez, A. et al. Usefulness of antioxidants as adjuvant therapy for septic shock: A randomized clinical trial. Medicina (Kaunas) 56(11), 619 (2020).
Sevransky, J. E. et al. Effect of vitamin C, thiamine, and hydrocortisone on ventilator- and vasopressor-free days in patients with sepsis: The VICTAS randomized clinical trial. JAMA 325(8), 742–750 (2021).
Mirea, L. et al. Continuous administration of corticosteroids in septic shock can reduce risk of hypernatremia. Crit. Care 18(1), 1–82 (2014).
Rygard, S. L. et al. Low-dose corticosteroids for adult patients with septic shock: A systematic review with meta-analysis and trial sequential analysis. Intensive Care Med. 44(7), 1003–1016 (2018).
Qian, X., Zhang, Z., Li, F. & Wu, L. Intravenous thiamine for septic shock: A meta-analysis of randomized controlled trials. Am. J. Emerg. Med. 38(12), 2718–2722 (2020).
Author information
Authors and Affiliations
Contributions
K.F. conceived the study, performed the literature search, analyzed the data and drafted the manuscript. S.A. and G.N. did the acquisition of data and the revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fong, K.M., Au, S.Y. & Ng, G.W.Y. Steroid, ascorbic acid, and thiamine in adults with sepsis and septic shock: a systematic review and component network meta-analysis. Sci Rep 11, 15777 (2021). https://doi.org/10.1038/s41598-021-95386-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-95386-9
This article is cited by
-
Data visualisation approaches for component network meta-analysis: visualising the data structure
BMC Medical Research Methodology (2023)
-
The effectiveness of parenting program components on disruptive and delinquent behaviors during early and middle childhood: a component network meta-analysis
Journal of Experimental Criminology (2023)
-
Vitamin C for ≥ 5 days is associated with decreased hospital mortality in sepsis subgroups: a nationwide cohort study
Critical Care (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.