Abstract
Given the unclear preference criteria for regorafenib in treating refractory metastatic colorectal cancer (mCRC), this study aimed to construct an algorithm in selecting right patients for regorafenib. This was a multicenter retrospective cohort study. Patients with pathology confirmed mCRC and administered with regorafenib for > 3 weeks were enrolled. Patients with good response were defined to have progression-free survival (PFS) of ≥ 4 months. The Kaplan–Meier plot was used to analyze survival. A Cox proportional hazards model was used to analyze univariate and multivariate prognostic factors and was visualized using forest plot. A clustering heatmap was used to classify patients according to responses. The decision tree and nomogram were used to construct the approaching algorithm. A total of 613 patients was analyzed. The median PFS and overall survival (OS) were 2.7 and 10.6 months, respectively. The partial response and stable disease rate are 2.4% and 36.4%. The interval between metastasis (M1) and regorafenib, metastatic status (number, liver, and brain), and CEA level were independent prognostics factors of PFS that classifies patients into three groups: good, bad and modest-1/modest-2 group with PFS > = 4 months rates of 51%, 20%, 39% and 30%, respectively. Results were used to develop the decision tree and nomogram for approaching patients indicated with regorafenib. The preference criteria for regorafenib in treating patients with refractory mCRC are small tumor burden (CEA), slow growth (interval between metastasis and regorafenib) and poor/scanty spread (metastatic status: number and sites of metastasis): The 3S rules.
TRIAL registration ClinicalTrials.gov Identifier: NCT03829852; Date of first registration (February 11, 2019).
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the leading cancer worldwide1,2,3,4. Approximately 20% of patients with CRC present with stage IV (metastatic CRC (mCRC)), and approximately 80% present with stage I–III. Unfortunately, approximately 40% of patients with stage I–III finally progress to mCRC5. Despite the advancement of biochemotherapy for the treatment of mCRC, the median overall survival (OS) remains at 30–36 months6,7,8,9,10. Before the availability of new agents, the more precise strategy in selecting the right biochemotherapy for the right patients remains the cornerstone for mCRC treatment.
Treatment of mCRC may consist of chemotherapy, precision cancer medicines, and immunotherapy or some combination that is often determined by genomic testing of the cancer2,6,9,10,11,12,13,14,15,16,17. Some patients might be only treated with precision cancer agents or immunotherapy16,17 and might avoid chemotherapy at initial treatment. Systemic agents for mCRC consist of chemotherapy based on a fluoropyrimidine (5-FU), oxaliplatin, and irinotecan (in combination or in sequence) and monoclonal/targeted agents targeting BRAF mutation18,19,20, NTRK fusion oncoprotein21,22, vascular endothelial growth factor (VEGF) and epidermal growth factor receptor (EGFR) (in patients with RAS and BRAF wild-type tumors)23,24 as well as anti-programmed death-1 (PD-1)/ anti-programmed death ligand-1 (PD-L1) agents targeting patients with microsatellite instability-high (MSI-H) or with high tumor mutation burden16,17. Unfortunately, majority of patients finally develop drug resistance and thereby require late-line agents such as regorafenib25,26 and TAS-10227,28,29.
These two agents are the late-line therapeutic options for patients. Sadly, the PR rate of both regorafenib and TAS-102 is approximately 1%–3%, comprising 60% of patients who did not respond to these agents. To date, several studies6,25,26,27,28,30,31,32,33 try to prove the sequence of regorafenib and TAS-102 for the treatment of refractory mCRC, and majority of them point out that their sequences did affect the OS33,34,35,36. However, a key difference was observed between regorafenib and TAS-102. TAS-102 is a traditional chemotherapy37,38,39 and regorafenib15,25,26,29,31,40,41 is a multiple oncogenic receptor tyrosine kinases inhibitor25,26,30,31,42. In a systematic review and network meta-analysis comparing regorafenib and TAS-102 showed similar OS and progression-free survival (PFS). In the subgroup analysis, regorafenib was associated with a lower all-grade toxicity for anemia, neutropenia and thrombocytopenia. On contrast, regorafenib was associated with higher all-grade hand foot skin reaction (HFSR). In addition, regorafenib was associated with a lower grade 3 to 5 toxicity for anemia and neutropenia, but regorafenib showed a higher grade 3–5 HFSR and fatigue compared with TAS-10233. Its efficacy was further proven in the IMblaze370 study, showing that atezolizumab with or without cobimetinib versus regorafenib in a previously treated mCRC did not differ43. Thus, the question is not the efficacy of regorafenib, but who is the right patient for regorafenib. To the best of our knowledge, no consensus or strategy exists in selecting the right patient for regorafenib administration.
In our multicenter retrospective study in Taiwan, a large-scale cohort was used to explore the prognostic markers of refractory mCRC after the regorafenib treatment. Significant prognostic markers were used to determine an easy and more precise guide to select the right patients for regorafenib, leading to more survival and avoiding unnecessary HFSR.
Results
Patient characteristics
Patients’ baseline characteristics are shown in Table 1. A total of 613 patients were enrolled for analysis. The mean age of patients was 61.4 years, and the mean body mass index was 23.4 kg/m2. About 76.3% of patients had good performance status (Eastern Cooperative Oncology Group (ECOG) 1 and 2), 2.4% had not only one location of primary tumor, and 77.8% had a left-sided mCRC. About 59.4% of patients had more than one metastatic site. In patients with available gene testing, the mutation rates of KRAS, NRAS, BRAF, and MSI-H were 46.5%, 5.9%, 2.9%, and 3.1%, respectively.
Treatment efficacy
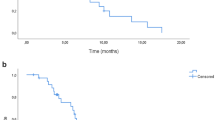
Patients administered with regorafenib had a median PFS of 2.7 months (95% confidence internal (CI), 2.4–3.1) (Fig. 1a). Patients administered with regorafenib had a median OS of 10.6 (95% CI, 9.3–11.8) months (Fig. 1b). The response rate is shown in Supplemental Table 1. For the overall study population, PR, SD, progressive disease (PD) and non-assessable rates were 2.4% (n = 15), 36.4% (n = 223), 53.8% (n = 330), and 7.3% (n = 45), respectively. The impact of the initial regorafenib dosage on response is listed in Supplemental Table 2, the initially standard dosage did not significantly impact on regorafenib efficacy. The disease control rate (DCR) is not different between those with < 160 mg than with 160 mg (40.2% vs. 37.9%).
Prognostic factors for PFS and OS from univariate and multivariate analyses
To clarify the potential prognostic factors in the treatment of refractory mCRC by regorafenib, a Cox proportional hazards model was used. The forest plot in Fig. 2 summarizes the univariate (Fig. 2a) and multivariate (Fig. 2b) analyses of prognostic factors to predict the PFS (The data is shown in Supplemental Table 3). The forest plot in Fig. 3 presents univariate (Fig. 3a) and multivariate (Fig. 3b) analyses of prognostic factors in predicting OS (The data is shown in Supplemental Table 4).
In univariate analysis according to PFS, ECOG, primary colectomy, interval between M1 and regorafenib, pathology (Carcinoma vs adenocarcinoma), number of metastatic sites, liver metastasis, brain metastasis, and CEA high (≥ 50 ng/mL) were identified as significant prognostic factors in predicting PFS. After controlling for other potential confounding factors, interval between M1 and regorafenib, number of metastatic sites, liver metastasis, brain metastasis, and CEA high (≥ 50 ng/mL) remained as independent prognostic factors. The reprehensive KM survival plots by independently significant factors are shown in Fig. 1. Patients with ≥ 3 metastatic sites had a poor PFS than those with < 3 metastatic sites (2.2 vs. 3.1 months, P < 0.001) (Fig. 1c). Patients without liver metastasis had a better PFS than those with liver metastasis (4.1 vs. 2.3 months, P < 0.001) (Fig. 1d). Patients with interval between metastasis (M1) and regorafenib of ≥ 19.13 months had a good PFS than those with < 19.13 months (3.3 vs. 2.4 months, P < 0.001) (Fig. 1e). Patients with CEA of ≥ 50 ng/mL had poor PFS than those with lower CEA levels (2.3 vs. 3.6 months, P < 0.001) (Fig. 1f).
In univariate analysis according to OS, BMI, ECOG, location, primary colectomy, interval between M1 and regorafenib, pathology (carcinoma vs adenocarcinoma), number of metastatic sites, liver metastasis, brain metastasis, and CEA high (≥ 50 ng/mL) were identified as significant prognostic factors in predicting OS. After controlling for other potential confounding factors, ECOG, interval between M1 and regorafenib, pathology (carcinoma vs adenocarcinoma), number of metastatic sites, liver metastasis, brain metastasis, and CEA high (≥ 50 ng/mL) remained as independent prognostic factors.
The clustering heatmap
In the attempt to classify patients taking regorafenib into different groups according to response, a total of 552 patients with PFS of ≥ 4 months or those with event (PD) of < 4 months were used to create the clustering heatmap. The rationale in selecting the cut-off level of 4 months with scientific aspect based on median PFS of 2 months in CORRECT trial25. It means patient apply twice, indicating a true response to regorafenib. Then, the response was good if PFS was ≥ 4 months and bad if PFS was < 4 months. Significant prognostic factors in multivariate Cox proportional hazards model analysis were used in the clustering heatmap (2). Both the row and column clustering were arranged. The k-means cluster is 4. The clustering heatmap is shown in the middle of Fig. 4. Patients were grouped into three major groups: good, modest, and bad. The modest group is further classified into modest-1 and modest-2 groups. The PFS > = 4 months rates in the good and bad groups were 51% and 20%, respectively. The PFS > = 4 months rates in the modest-1 and modest-2 groups are 39% and 30%, respectively. The statical results are shown at the top and bottom in Fig. 4. The characteristics of patients in the bad group were large burden (CEA > = 50 ng/mL) and rapid growth (short interval between M1 and regorafenib) and poor/scanty spread (multiple metastatic sites and liver metastasis). The carton-like score used to demonstrate differences among groups is listed at the bottom in Fig. 4.
The clustering heatmap (k-means = 4) was used to classify patients into good, bad, modest 1, and modest 2 groups according to significantly independent prognostic factors by PFS > = 4 months or not. (Top) Pie charts represent the distribution of patients with good and bad responses in four groups. (Middle) Clustering heatmap visualizes the different groups’ distribution of independent prognostic factors. (Bottom) Independent prognostic factors were classified into three patterns of cancer behaviors: growth rate, metastasis ability, and tumor burden. It was used to score the grouped patients. Abbreviations: ad, adenocarcinoma; HR, hazard ratio; CI, confidence interval.
Decision tree analysis to develop predictive algorithms
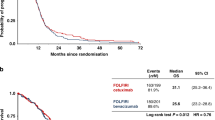
The critical role of patients with PFS > = 4 months is shown in Fig. 5a,b. Patients with PFS > = 4 months significantly had good PFS and OS, comparing to those with PFS < 4 months. The decision tree based on Chi-square Automatic Interaction Detector (CHARD) was used to develop the predictive algorithms. A total of 552 patients with PFS > = 4 months or those with event (PD) at < 4 months was used to create a decision tree (Fig. 5c) (Decision tree with variable statistics is listed in supplemental Fig. 1). The significant prognostic factors for PFS in multivariate Cox proportional hazards model analysis were used in the decision tree. Patients were divided into four groups. The same term was used to describe these groups: good, modest-1, modest-2, and bad. The PFS > = 4 months rates in the good, modest-1, modest-2 and bad group were 54.1% ((78 + 35)/ (142 + 67)), 39.0%, 30.0% ((22 + 25)/ (69 + 89)) and 13.6%, respectively. The PFS > = 4 months rate in the decision tree is similar to that of the clustering heatmap. However, it is can be easily incorporated into clinical practice.
Kaplan–Meier curves for (a) progression-free survival (PFS); (b) overall survival (OS) by patient with PFS > = 4 months or not. (c) The decision tree in predicating the priority right of regorafenib for the treatment of refractory metastatic colorectal cancer according to liver metastasis, CEA, and interval between M1 and regorafenib. (d) The prognostic nomogram for OS of patients after regorafenib.
Prognostic nomogram
Our previous algorithms would be partially validated for OS. The prognostic nomogram for OS of patients with mCRC after regorafenib was performed (Fig. 5d) (The 12-month calibration curve of the nomogram is shown in supplemental Fig. 2). In the nomogram for OS, each independent prognostic markers with a given value can be mapped to the points axis. The sum of these points can be referred to in the total points axis. The sum of these numbers is located on the total points axis, and a line is drawn downward to the survival axis to determine the likelihood of 6-month, 12 month and 18-month OS, respectively. The c-index was 0.674 and it was acceptable.
Discussion
To our knowledge, this is the first study that creates a strategy in selecting the right patients for the treatment of refractory mCRC with regorafenib using a large-scale post-market data. The flowchart representing a decision tree and prognostic nomogram are shown in Fig. 5c. Regorafenib could be considered in patients without liver metastasis and CEA of < 50 ng/mL or in those with liver metastasis, CEA < 50 ng/mL and interval between M1 and regorafenib > 25.6 months. Conversely, regorafenib might not be used with top priority in patients with liver metastasis, CEA of > = 50 ng/mL and interval between M1 and regorafenib of < 22.1 months.
The rationale for our approaching strategy based on the results of clarifying the potential prognostic factors for PFS via the univariate and multivariate Cox proportional hazards model for the treatment of refractory mCRC by regorafenib. The clustering heatmap visualization helps us understand the rationale. The end-point is the PFS of ≥ 4 months and patients were classified into good and bad responses (PFS > = 4 months vs PFS < 4 months). In Fig. 4, regorafenib could be considered in patients with low tumor growth rate (long interval between M1 and regorafenib), lower metastatic ability (less metastatic sites and without liver or brain metastasis), and low tumor burden (low CEA level). These patients were the good group, and the 4-month PFS rate is 51%. Conversely, regorafenib might not be indicated for patients with high tumor growth rate (short interval between M1 and regorafenib), high metastatic ability (more metastatic sites and/or with liver metastasis), and high tumor burden (high CEA level). These patients were in the bad group with a 4-month PFS rate of 20%. The 2.5-fold change of response rate was noted among patients in the good group as compared to those in the bad group. In addition, patients in the modest-1 and modest-2 groups have 4-month PFS rate of 39% and 30%, respectively. Then, the flowchart representing the decision tree and prognostic nomogram are easily applicable into clinical practice (Fig. 5c,d). Moreover, RAS and BRAF were not considered as prognostic markers, which are similar to those of previous literatures25,44. Moreover, 255 of 613 enrolled patients had microsatellite status reports, and the incidence of MSI-H was 3.1% and MSI-H status is not a significant prognostic factor in PFS and OS analyses. As compared with previous studies (subgroups analysis of CORRECT25 AND CONCUR26), the time from the first diagnosis of metastatic disease to randomization did not affect the efficacy of regorafenib, which is not similar to our findings. However, (K-)RAS and BRAF states did not interfere the regorafenib efficacy and were similar to our findings.
In our study, the median PFS and OS in patients taking regorafenib were 2.7 (95% CI, 2.4–3.1) and 10.6 (95% CI, 9.3–11.8) months, respectively. The PFS is similar to those of previous studies; however, the OS was longer than that of patients taking regorafenib in the CORRECT trial in which patients had a median OS of 6.4 (PFS, 1.9) months25 and in the REBECCA trial in which patients had a median OS of 5.5 (PFS, 2.7) months30. The CORRELATE trial, a real-world analysis of regorafenib effectiveness, showed a median OS of 7.6 months42. A trend toward longer OS in the late-run clinical studies was observed (CORRECT in 2013; REBECCA in 2016; CORRELATE in 2017 and our study in 2020). The longer OS observed in our study may be attributed to the addition of other salvage regimen, such as TAS-102 and challenge of previously active agents. A subgroup analysis of Taiwanese patients with mCRC in the CORRELATE trial showed a median OS of 11.6 months in 201845.
With the respect of an impact of dosage on regorafenib efficacy, the result is listed in the Supplemental Table 2. The initial dosage of 160 mg or not did not affect the PR and DCR rates. Our report is similar to those of previous studies. The initially standard dosage did not significantly impact on regorafenib efficacy. The PR and DCR were not different between those with < 160 mg than with 160 mg (PR: 2.8% vs. 2.0% and DCR: 37.9% vs. 40.2%). Similarly, with those in ReDOSE study31 studies, an escalation strategy has previously been shown to improve survival as compared with those of a standard-dose regimen.
In the previous papers about survival of peritoneal metastasis46,47, most of them reported that the survival of peritoneal metastasis was poor. In our study, abdominal/peritoneal metastasis (APM) was not a prognostic marker in the univariate analysis according to PFS and OS. The response rate was also not different between patients with APM or not (P-value = 0.407). For patients with APM, rates of PR, SD or PD were 1.1%, 44.3% and 54.5%, respectively. For patients without APM, rates of PR, SD, and PD were 2.9%, 38.3%, and 58.8%, respectively. In the PRODIGE 7 trial, the median OS was 41.7 months in the cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy group and 41.2 months in the cytoreductive surgery group (hazard ratio 1.00; stratified log-rank P-value = 0.99)48. It pointed out that selected patients with APM had the relative better OS. A reasonable explanation for our finding was that some patients with APM might die early in the course of disease. Patients who could receive regorafenib were somehow a relatively good subpopulation. The peritoneal cancer index score was a good tool in predicting the impact of peritoneal metastases burden on survival. The further study should be arranged to clarify the impact of peritoneal metastases burden on efficacy of regorafenib.
Several limitations were observed in our study. First, its retrospective design may have led to an inevitable selection bias. Second, patients who did not continued the treatment for > 3 weeks were excluded in the analysis during screening also leading to selection bias, e.g., patients with an intrinsically better prognosis were selected. Third, adverse effects reports were not provided, because not all patients in the study had detailed documented adverse effects. Fourth, patient’s preferred dosage or sequence with TAS-102 was also part of physician’s consideration when determining the treatment sequence and dosage. Finally, TAS-102 reimbursement was only partially permitted in Taiwan during the later parts of this study and most of patients did not receive TAS-102 before the use of regorafenib. Therefore, our proposed algorithm for selecting patients who will benefit most from regorafenib would be only applicated in patients with drug resistance to 5-FU, irinotecan, oxaliplatin, bevacizumab, and cetuximab/panitumumab (in RAS wild-type patients).
Conclusion
Regorafenib could be considered in patients without liver metastasis and CEA of < 50 ng/mL or in those with liver metastasis, CEA < 50 ng/mL and interval between M1 and regorafenib > 25.6 months. Conversely, regorafenib might not be used with top priority in patients with liver metastasis, CEA of > = 50 ng/mL and interval between M1 and regorafenib of < 22.1 months.
Material and methods
Patients
This was a multicenter retrospective cohort study based on patient data collected between August 2012 and January 2018 at Chang-Geng Medical Foundation Linkou Chang-Geng Memorial Hospital, Koo Foundation Sun Yat-Sen Cancer Center, and Taipei Veterans General Hospital, Taiwan. This study followed the Helsinki Declaration guidelines and was approved by the ethics committees and institutional review boards of the respective institutions. The requirement for informed consent was waived due to the retrospective nature of the study.
Patients with pathologically confirmed refractory mCRC and had been administered regorafenib for > 3 weeks were enrolled into the analysis. They were resistant to 5-FU, irinotecan, oxaliplatin, bevacizumab, and cetuximab/panitumumab (in RAS wild-type patients). Basic clinicopathologic parameters were recorded, including age, gender, tumor location, pathologic features (e.g., histological type, grade, RAS, BRAF, and MSI), and metastatic sites. The definition of APM generally refers to the metastatic involvement of the peritoneum. The right-sided CRC consist of cecum, ascending colon, hepatic flexure, and transverse colon and the left-sided CRC consist of splenic flexure, descending colon, sigmoid colon, rectosigmoid junction, and rectum. Both of the standard regimen (160 mg) or escalation strategy (< 160 mg) for initial regorafenib treatment were frequently implemented depending on the physician’s judgment and based on patient compliance and adverse effects.
Efficacy evaluation
The metastatic disease was evaluated based on the Response Evaluation Criteria in Solid tumor version 1.1. The best response was recorded after the treatment initiation, and the disease control rate was regarded as the proportion of patients with complete response (CR), partial response (PR), and stable disease (SD). We investigated OS (the time from regorafenib to the time of death caused by the disease) and PFS (the time from regorafenib to the time of disease progression observed by radiologic imaging or the time when intolerable adverse effects were observed).
Statistical analysis
Continuous data are expressed as mean ± standard deviation. Statistical comparisons were based on nonparametric tests. Correlations between clinicopathological variables and responses were analyzed using χ2 test or Fisher’s exact test. Survival was estimated using the Kaplan–Meier (KM) method. The Cox proportional hazards model was used for univariate and multivariate analyses to determine the prognostic impact on clinicopathological factors on survival end-points. Factors with P-value of < 0.10 in the univariate analysis were enrolled in the multivariable analysis. Significant prognostic factors in multivariate analyses using a Cox proportional hazards model were enrolled into the decision tree analysis. The forest plot was used to visualize the results.
The R program and complex heatmap package49 were used to generate clustering heatmap from significant prognostic factors in multivariate analyses using a Cox proportional hazards model. Good response group was defined as patients with PFS of ≥ 4 months, whereas bad response as patients with PD event and PFS of < 4 months. This clustering heatmap with k-means of 4 was used to visualize the clinical pattern of patients with good and bad responses to regorafenib49. The clustering was applied to grouping patients according to independent significant prognostic factors in multivariate analyses according to PFS. The decision tree with Chi-Square Automatic Interaction Detector model was drawn according to same independent significant prognostic factors in multivariate analyses according to PFS. The prognostic nomogram for OS of patients with mCRC after regorafenib was performed by using R software.
A two-sided P-value of < 0.05 was regarded as statistically significant. SPSS software was used for all statistical analyses, and the R program was also used.
Ethical approval
This retrospective study was conducted based on population-based data from Chang-Geng Medical Foundation Linkou Chang-Geng Memorial Hospital, Koo Foundation Sun Yat-Sen Cancer Center, and Taipei Veterans General Hospital, Taiwan. This study followed the Helsinki Declaration guidelines and was approved by “Chang Gung Medical Foundation Institutional Review Board”,” Institutional Review Board of the Koo Foundation Sun Yat-Sen Cancer Center” and “Institutional Review Board of the Taipei Veterans General Hospital”. The requirement for informed consent was waived due to the retrospective nature of the study by “Chang Gung Medical Foundation Institutional Review Board”,” Institutional Review Board of the Koo Foundation Sun Yat-Sen Cancer Center”, and “Institutional Review Board of the Taipei Veterans General Hospital”.
References
Global Burden of Disease Cancer, C. et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 3, 524–548. https://doi.org/10.1001/jamaoncol.2016.5688 (2017).
Van Cutsem, E. et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann. Oncol. 27, 1386–1422. https://doi.org/10.1093/annonc/mdw235 (2016).
Grothey, A., Sargent, D., Goldberg, R. M. & Schmoll, H. J. Survival of patients with advanced colorectal cancer improves with the availability of fluorouracil-leucovorin, irinotecan, and oxaliplatin in the course of treatment. J. Clin. Oncol. 22, 1209–1214. https://doi.org/10.1200/JCO.2004.11.037 (2004).
Siegel, R. L. et al. Colorectal cancer statistics, 2017. CA Cancer J. Clin. 67, 177–193. https://doi.org/10.3322/caac.21395 (2017).
Weiser, M. R. AJCC 8th edition: colorectal cancer. Ann. Surg. Oncol. 25, 1454–1455. https://doi.org/10.1245/s10434-018-6462-1 (2018).
Walter, T. et al. Systematic review and network meta-analyses of third-line treatments for metastatic colorectal cancer. J. Cancer Res. Clin. Oncol. 146, 2575–2587. https://doi.org/10.1007/s00432-020-03315-6 (2020).
Kuipers, E. J. et al. Colorectal cancer. Nat. Rev. Dis. Primers 1, 15065. https://doi.org/10.1038/nrdp.2015.65 (2015).
Lu, H. J. et al. Primary tumor location is an important predictive factor for wild-type KRAS metastatic colon cancer treated with cetuximab as front-line bio-therapy. Asia Pac. J. Clin. Oncol. 12, 207–215. https://doi.org/10.1111/ajco.12469 (2016).
Yang, Y. H. et al. Comparison of cetuximab to bevacizumab as the first-line bio-chemotherapy for patients with metastatic colorectal cancer: superior progression-free survival is restricted to patients with measurable tumors and objective tumor response–a retrospective study. J. Cancer Res. Clin. Oncol. 140, 1927–1936. https://doi.org/10.1007/s00432-014-1741-0 (2014).
Teng, H. W. et al. BRAF mutation is a prognostic biomarker for colorectal liver metastasectomy. J. Surg. Oncol. 106, 123–129. https://doi.org/10.1002/jso.23063 (2012).
Guinney, J. et al. The consensus molecular subtypes of colorectal cancer. Nat. Med. 21, 1350–1356. https://doi.org/10.1038/nm.3967 (2015).
Salvatore, L. et al. Management of metastatic colorectal cancer patients: guidelines of the Italian Medical Oncology Association (AIOM). ESMO Open 2, e000147. https://doi.org/10.1136/esmoopen-2016-000147 (2017).
Liu, C. Y. et al. ER stress-related ATF6 upregulates CIP2A and contributes to poor prognosis of colon cancer. Mol. Oncol. 12, 1706–1717. https://doi.org/10.1002/1878-0261.12365 (2018).
Teng, H. W. et al. CIP2A is a predictor of poor prognosis in colon cancer. J. Gastrointest. Surg. 16, 1037–1047. https://doi.org/10.1007/s11605-012-1828-3 (2012).
Tai, C. C. et al. Comparing late-line treatment sequence of regorafenib and reduced-intensity FOLFOXIRI for refractory metastatic colorectal cancer. Am. J. Clin. Oncol. 43, 28–34. https://doi.org/10.1097/COC.0000000000000637 (2020).
Grothey, A. Pembrolizumab in MSI-H-dMMR advanced colorectal cancer—a new standard of care. N Engl J Med 383, 2283–2285. https://doi.org/10.1056/NEJMe2031294 (2020).
Andre, T. et al. Pembrolizumab in microsatellite-instability-high advanced colorectal cancer. N. Engl. J. Med. 383, 2207–2218. https://doi.org/10.1056/NEJMoa2017699 (2020).
Sullivan, R. J. et al. A phase Ib/II study of the BRAF inhibitor encorafenib plus the MEK inhibitor binimetinib in patients with BRAF(V600E/K)-mutant solid tumors. Clin. Cancer Res. 26, 5102–5112. https://doi.org/10.1158/1078-0432.CCR-19-3550 (2020).
Huijberts, S. C., van Geel, R. M., Bernards, R., Beijnen, J. H. & Steeghs, N. Encorafenib, binimetinib and cetuximab combined therapy for patients with BRAFV600E mutant metastatic colorectal cancer. Future Oncol. 16, 161–173. https://doi.org/10.2217/fon-2019-0748 (2020).
Shahjehan, F., Kamatham, S., Chandrasekharan, C. & Kasi, P. M. Binimetinib, encorafenib and cetuximab (BEACON Trial) combination therapy for patients with BRAF V600E-mutant metastatic colorectal cancer. Drugs Today (Barc) 55, 683–693. https://doi.org/10.1358/dot.2019.55.11.3035584 (2019).
Pietrantonio, F. et al. ALK, ROS1, and NTRK rearrangements in metastatic colorectal cancer. J Natl Cancer Inst 109. https://doi.org/10.1093/jnci/djx089 (2017).
Ardini, E. & Siena, S. Entrectinib approval by EMA reinforces options for ROS1 and tumour agnostic NTRK targeted cancer therapies. ESMO Open 5. https://doi.org/10.1136/esmoopen-2020-000867 (2020).
Heinemann, V. et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol. 15, 1065–1075. https://doi.org/10.1016/S1470-2045(14)70330-4 (2014).
Venook, A. P. et al. Effect of first-line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients with KRAS wild-type advanced or metastatic colorectal cancer: a randomized clinical trial. JAMA 317, 2392–2401. https://doi.org/10.1001/jama.2017.7105 (2017).
Grothey, A. et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 381, 303–312. https://doi.org/10.1016/S0140-6736(12)61900-X (2013).
Li, J. et al. Regorafenib plus best supportive care versus placebo plus best supportive care in Asian patients with previously treated metastatic colorectal cancer (CONCUR): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 16, 619–629. https://doi.org/10.1016/S1470-2045(15)70156-7 (2015).
Pfeiffer, P. et al. TAS-102 with or without bevacizumab in patients with chemorefractory metastatic colorectal cancer: an investigator-initiated, open-label, randomised, phase 2 trial. Lancet Oncol. 21, 412–420. https://doi.org/10.1016/S1470-2045(19)30827-7 (2020).
Kuboki, Y. et al. TAS-102 plus bevacizumab for patients with metastatic colorectal cancer refractory to standard therapies (C-TASK FORCE): an investigator-initiated, open-label, single-arm, multicentre, phase 1/2 study. Lancet Oncol. 18, 1172–1181. https://doi.org/10.1016/S1470-2045(17)30425-4 (2017).
Yoshida, Y. et al. Combination of TAS-102 and bevacizumab as third-line treatment for metastatic colorectal cancer: TAS-CC3 study. Int. J. Clin. Oncol. https://doi.org/10.1007/s10147-020-01794-8 (2020).
Adenis, A. et al. Survival, safety, and prognostic factors for outcome with Regorafenib in patients with metastatic colorectal cancer refractory to standard therapies: results from a multicenter study (REBECCA) nested within a compassionate use program. BMC Cancer 16, 412. https://doi.org/10.1186/s12885-016-2440-9 (2016).
Bekaii-Saab, T. S. et al. Regorafenib dose-optimisation in patients with refractory metastatic colorectal cancer (ReDOS): a randomised, multicentre, open-label, phase 2 study. Lancet Oncol. 20, 1070–1082. https://doi.org/10.1016/S1470-2045(19)30272-4 (2019).
van de Velde, C. J. et al. EURECCA colorectal: multidisciplinary management: European consensus conference colon & rectum. Eur. J. Cancer 50, 1e1–1e34, https://doi.org/10.1016/j.ejca.2013.06.048 (2014).
Abrahao, A. B. K., Ko, Y. J., Berry, S. & Chan, K. K. W. A comparison of regorafenib and TAS-102 for metastatic colorectal cancer: a systematic review and network meta-analysis. Clin. Colorectal. Cancer 17, 113–120. https://doi.org/10.1016/j.clcc.2017.10.016 (2018).
Masuishi, T. et al. Regorafenib versus trifluridine/tipiracil for refractory metastatic colorectal cancer: a retrospective comparison. Clin. Colorectal. Cancer 16, e15–e22. https://doi.org/10.1016/j.clcc.2016.07.019 (2017).
Moriwaki, T. et al. Propensity score analysis of regorafenib versus trifluridine/tipiracil in patients with metastatic colorectal cancer refractory to standard chemotherapy (REGOTAS): a Japanese Society for Cancer of the colon and rectum multicenter observational study. Oncologist 23, 7–15. https://doi.org/10.1634/theoncologist.2017-0275 (2018).
Cho, S. K., Hay, J. W. & Barzi, A. Cost-effectiveness analysis of regorafenib and TAS-102 in refractory metastatic colorectal cancer in the United States. Clin. Colorectal. Cancer 17, e751–e761. https://doi.org/10.1016/j.clcc.2018.08.003 (2018).
Mayer, R. J. et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N. Engl. J. Med. 372, 1909–1919. https://doi.org/10.1056/NEJMoa1414325 (2015).
Cleghorn, S. TAS-102 for metastatic refractory colorectal cancer. Lancet Oncol. 16, e314. https://doi.org/10.1016/S1470-2045(15)70246-9 (2015).
Yoshino, T. et al. TAS-102 monotherapy for pretreated metastatic colorectal cancer: a double-blind, randomised, placebo-controlled phase 2 trial. Lancet Oncol. 13, 993–1001. https://doi.org/10.1016/S1470-2045(12)70345-5 (2012).
Chen, H. M. et al. Reduced-intensity FOLFOXIRI in treating refractory metastatic colorectal cancer: a pilot study. Am. J. Clin. Oncol. 40, 260–265. https://doi.org/10.1097/COC.0000000000000137 (2017).
Tsai, Y. J. et al. Adjuvant FOLFOX treatment for stage III colon cancer: how many cycles are enough?. Springerplus 5, 1318. https://doi.org/10.1186/s40064-016-2976-9 (2016).
Ducreux, M. et al. Safety and effectiveness of regorafenib in patients with metastatic colorectal cancer in routine clinical practice in the prospective, observational CORRELATE study. Eur. J. Cancer 123, 146–154. https://doi.org/10.1016/j.ejca.2019.09.015 (2019).
Eng, C. et al. Atezolizumab with or without cobimetinib versus regorafenib in previously treated metastatic colorectal cancer (IMblaze370): a multicentre, open-label, phase 3, randomised, controlled trial. Lancet Oncol. 20, 849–861. https://doi.org/10.1016/S1470-2045(19)30027-0 (2019).
Tabernero, J. et al. Analysis of circulating DNA and protein biomarkers to predict the clinical activity of regorafenib and assess prognosis in patients with metastatic colorectal cancer: a retrospective, exploratory analysis of the CORRECT trial. Lancet Oncol. 16, 937–948. https://doi.org/10.1016/S1470-2045(15)00138-2 (2015).
Yeh, K. H. et al. Real-world evidence of the safety and effectiveness of regorafenib in patients with metastatic colorectal cancer (mCRC) from Taiwan: a subgroup analysis from the prospective, observational CORRELATE study. Ann. Oncol. 29, ix35-ix36, https://doi.org/10.1093/annonc/mdy431.023 (2018).
Franko, J. et al. Treatment of colorectal peritoneal carcinomatosis with systemic chemotherapy: a pooled analysis of north central cancer treatment group phase III trials N9741 and N9841. J. Clin. Oncol. 30, 263–267. https://doi.org/10.1200/JCO.2011.37.1039 (2012).
Markman, M. Intraperitoneal hyperthermic chemotherapy as treatment of peritoneal carcinomatosis of colorectal cancer. J. Clin. Oncol. 22, 1527; author reply 1529, https://doi.org/10.1200/JCO.2004.99.263 (2004).
Quenet, F. et al. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy versus cytoreductive surgery alone for colorectal peritoneal metastases (PRODIGE 7): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 22, 256–266. https://doi.org/10.1016/S1470-2045(20)30599-4 (2021).
Gu, Z., Eils, R. & Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 32, 2847–2849. https://doi.org/10.1093/bioinformatics/btw313 (2016).
Acknowledgements
We thank: Bayer’s financial support of our investigator-initiated research and Uccello Ying Shiuan Li, Meng-Ting, Lin for providing scientific support.
Funding
This work was supported by Taiwan Clinical Oncology Research Foundation, sponsored by Bayer Taiwan Co., Ltd. Pharmaceuticals, Ministry of Science and Technology, Taiwan (109-2314-B-075-081-MY3, to H.W.T) and Taipei Veterans General Hospital (110 DHA0100397, V110C-189, V109C-151 to H.W.T).
Author information
Authors and Affiliations
Contributions
HC.H., KC. H., WS.C., JK.J., SH.Y., HS.W., SC.C., YT.L., CC.L., HH.L., SC.H., HH.C., TS.Y., CC.C., C.Y., HW.T. HC.H., KC. H., WS.C., JK.J., SH.Y., HS.W., SC.C., YT.L., CC.L., HH.L., SC.H., HH.C., TS.Y., CC.C., C.Y., HW.T. conceived and developed the study, HC.H., KC. H.,HW.T. supervised the acquisition of the data, analyzed and interpreted the data. WS.C., JK.J., SH.Y., HS.W., SC.C., YT.L., CC.L., HH.L., SC.H., HH.C., TS.Y., CC.C., C.Y. assisted in collecting clinical information about the patients and helped to interpret the data. HC.H., KC. H.,HW.T. critically reviewed the manuscript.All authors edited and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
Hao-Wei Teng, Hung-Chih Hsu, Kuo-Cheng Huang received a research grant in this PI initiated clinical investigation trial from Bayer Taiwan Co., Ltd (Bayer was not involved in the study design, data interpretation, and manuscript preparation and review.) Wei-Shone Chen, Jeng-Kai Jiang, Shung-Haur Yang, Huann-Sheng Wang, Shih-Ching Chang, Yuan-Tzu Lan, Chun-Chi Lin, Hung-Hsin Lin, Sheng-Chieh Huang, Hou-Hsuan Cheng, Tsai-Sheng Yang, Chien-Chih Chen, Yee Chao has no actual or potential competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hsu, HC., Huang, KC., Chen, WS. et al. Preference criteria for regorafenib in treating refractory metastatic colorectal cancer are the small tumor burden, slow growth and poor/scanty spread. Sci Rep 11, 15370 (2021). https://doi.org/10.1038/s41598-021-94968-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-94968-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.