Abstract
Risk factors associated with mortality in invasive pneumococcal disease remain unclear. The present work is a meta-analysis of studies that enrolled only patients with invasive pneumococcal disease and reported on mortality. Potentially eligible reports were identified from PubMed, CHAHL, and Web of Science, comprising 26 reports in total. Overall mortality for invasive pneumococcal disease was reported as 20.8% (95% confidence interval (CI) 17.5–24%). Factors associated with mortality were age (odds ratio (OR) 3.04, 95% CI 2.5–3.68), nursing home (OR 1.62, 95% CI 1.13–2.32), nosocomial infection (OR 2.10, 95% CI 1.52–2.89), septic shock (OR 13.35, 95% CI 4.54–39.31), underlying chronic diseases (OR 2.34, 95% CI 1.78–3.09), solid organ tumor (OR 5.34, 95% CI 2.07–13.74), immunosuppressed status (OR 1.67, 95% CI 1.31–2.14), and alcohol abuse (OR 3.14, 95% CI 2.13–4.64). Mortality rates with invasive pneumococcal disease remained high, and these findings may help clinicians provide appropriate initial treatment for this disease.
Similar content being viewed by others
Introduction
Streptococcus pneumoniae commonly colonizes the upper airway asymptomatically, and is the cause of approximately 25–50% of cases of community-acquired pneumonia and meningitis1. The most severe form of pneumococcal infection, invasive pneumococcal disease (IPD), includes bacteremic pneumonia, meningitis, and septicemia with significant morbidity and mortality. In the United States of America, data from the Centers for Disease Control and Prevention showed 9.6 cases of IPD per 1,00,000 persons in all age groups2. In England and Wales, an IPD incidence of 7 per 1,00,000 persons in all age groups was reported, increasing to 21 per 1,00,000 among persons ≥ 65 years old3. The case fatality rate of IPD may reach 15–20% in adults and 30–40% in the elderly4.
A marked reduction in the rate of IPD due to pneumococcal conjugate vaccine and protein conjugate vaccine 13 serotypes has been reported for individuals ≥ 55 years old, with a much smaller decline in those 17–54 years old5. In the prospective international observational study, the overall mortality rate of pneumococcal bacteremia was 17%6. Although various articles have discussed risk factors for mortality from IPD, an overview has been lacking. This study was therefore designed to clarify prognostic factors contributing to death due to IPD.
Methods
Overview
The study protocol followed the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group statement and was registered to the University Hospital Medical Information Network (ID: UMIN000041377)7, 8. The need for institutional review board approval was waived because of the systematic review nature of this research. H.C. and M.M. independently performed the searching process and data extraction, and subsequently built consensus results.
Search of the literature
Three major databases (Medline, CHAHL, and Web of Science) were searched on July 30, 2020. The two reviewers independently extracted and recorded data for a predefined checklist including the following items: study characteristics (i.e., country and year of study), characteristics of the cohort, and case definitions. The following search formula was used: (“invasive pneumococcal disease” OR “pneumococcal infection” OR “Streptococcus pneumoniae infection” OR “pneumococcal bacteremia”) AND (“mortality” OR “death”) AND (“odds ratio” OR “relative risk” OR “hazard ratio”).
Inclusion and exclusion criteria
No restrictions were placed on article types or publication language. To be included, a study had to include: 1) patients with IPD; 2) data outlining risk factors for 30-day mortality or in-hospital mortality after multivariable regression analysis; and 3) no restrictions on vaccination.
Exclusion criteria were as follows: (1) patients < 15 or > 65 years old only; (2) risk factors assessed by univariable analysis only; (3) risk factors assessed in categories of subgroup only; or (4) patients with human immunodeficiency virus (HIV) infection only.
Definitions
IPD was defined as an illness occurring in association with the isolation of S. pneumoniae from a normally sterile body specimen including blood, cerebrospinal fluid, peritoneal, pleural or synovial fluid, or abscess aspirates or tissue specimens/swabs obtained intraoperatively, but excluding bronchoalveolar lavage. Immunosuppressed status was defined as HIV infection, splenectomy, hematological malignancy, autoimmune disorder, presence of a transplant, or cancer chemotherapy within 4 weeks before the onset of bacteremia. Septic shock was defined as sepsis-induced hypotension, persisting despite adequate fluid resuscitation, along with the presence of hypoperfusion abnormalities or organ dysfunction9.
Outcomes
Potential prognostic factors were defined in this study as any clinical information related to mortality such as age, sex, underlying diseases, focus of infection, and place of infection acquisition. Risk factors for 30-day and in-hospital mortalities were analyzed separately if > 3 articles were found in each subgroup.
Quality assessment
Two reviewers independently assessed the methodological quality of selected studies using the Newcastle–Ottawa Scale quality assessment to evaluate the quality of observational studies. Disagreements among reviewers were discussed, with agreement reached by consensus10.
Statistics
All analyses were performed using Review Manager version 5.3 (Cochrane Collaboration, Oxford, UK). Figures illustrated using Review Manager were adjusted as necessary. Prognostic factors for 30-day and in-hospital mortality rates were merged because of their similarity after meta-analysis. Heterogeneity evaluated using I2 statistics was interpreted as follows: I2 = 0%, no heterogeneity; I2 > 0% but < 25%, minimal heterogeneity; I2 ≥ 25% but < 50%, mild heterogeneity; I2 ≥ 50% but < 75%, moderate heterogeneity; and I2 ≥ 75%, strong heterogeneity11.
Results
Study search
Of these 26 articles identified, 2 demonstrated data from two independent populations (Fig. 1). Our analysis thus eventually extracted data from 16 countries for 27,742 patients with IPD, of whom 5810 died.
Characteristics of included studies
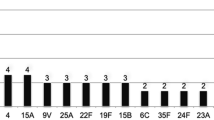
The 26 articles were published between 2000 and 2020, reported from Spain and the United States (n = 3 each), Canada, Japan, Israel, South Korea, the Netherlands, the United Kingdom, and Taiwan (n = 2 each), and 6 other countries (n = 1 each)6, 12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36. Two articles from Sweden and Georgia were multi-country studies compromising patients from 5 and 10 countries (Table 1). Twenty-one studies assessed either only adults or only adults plus adolescents ≥ 15 years old. Six studies included patients with IPD at any age. Six studies included only patients with HIV infection. Only two studies discussed status of HIV infection separately and the remaining four studies classified HIV as one condition defining an immunosuppressed status. Eight studies did not discuss the status of pneumococcal conjugate vaccination, seven studies revealed missing data for vaccination status, and nine studies discussed vaccination status (vaccination rates, 0–54.5%). No study identified a relationship between vaccination and mortality in multivariable analysis. Thirteen studies discussed in-hospital mortality as an outcome, twelve studies discussed 30-day mortality rates, and one study discussed 28-day mortality rate. The median in-hospital mortality was 23.0% (95% confidence interval (CI) 17.2–27.2%) and the median 30-day mortality rate was 18.9% (95% CI 13.9–23.9%). The overall mortality rate from IPD included in this study was 20.8% (95% CI 17.5–24.0%). Median Newcastle–Ottawa Scale score was 6, suggesting that most studies were of acceptable quality.
Meta-analysis
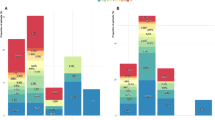
According to a random-model meta-analysis, study participants > 64 years old were at higher risk of in-hospital or 30-day mortality compared to those < 65 years old in subgroups (odds ratio (OR) 3.33, 95% CI 2.58–4.31, P < 0.001 and OR 2.65, 95% CI 2.07–3.39, P < 0.001, respectively) (Fig. 2). The total effect of age > 64 years old was a high risk for overall mortality (OR 3.04, 95% CI 2.50–3.68, P < 0.001, I2 = 37.2%). The I2 statistic of 37.2% suggested mild heterogeneity of this model. No heterogeneity between in-hospital mortality and 30-day mortality comparisons was revealed (P = 0.21).
Patients in a state of septic shock on admission demonstrated higher risks of in-hospital and 30-day mortality (OR 19.92, 95% CI 4.97–79.82, P < 0.001 and OR 7.24, 95% CI 1.30–40.33, respectively, P = 0.02) (Fig. 3). The total effect of septic shock was a high risk for overall mortality (OR 13.35, 95% CI 4.54–39.31, P < 0.001, I2 = 0%). The I2 statistic of 0% suggested no heterogeneity for this model. No heterogeneity between in-hospital mortality and 30-day mortality comparisons was revealed (P = 0.37).
Residence in a nursing home and nosocomial infection were associated with higher risks of mortality compared to community-acquired infection (OR 1.62, 95% CI 1.13–2.32, P = 0.009 and OR 2.10, 95% CI 1.52–2.89, P < 0.001, respectively) (Fig. 4).
Non-community-acquired infection showed a higher risk of mortality than community-acquired infection (OR 1.87, 95% CI 1.47–2.38, P < 0.001, I2 = 10.1%). The I2 statistic of 10.1% suggested minimal heterogeneity of this model.
Underlying chronic diseases also showed a risk of mortality (Figure S1). Liver disease, chronic kidney disease, and cardiovascular disease were frequently discussed (OR 2.73, 95% CI 1.57–4.76, P < 0.001; OR 2.99, 95% CI 2.09–4.27, P < 0.001; and OR 1.65, 95% CI 1.25–2.19, P < 0.001, respectively). The total effect of underlying chronic disease on mortality was 2.34 (95% CI 1.78–3.09, P < 0.001). The I2 statistic of 72.9% suggested strong heterogeneity for this model.
Immunosuppressed status was a prognostic factor for mortality from IPD (OR 1.51, 95% CI 1.24–1.84, P < 0.001, I2 = 47%) (Figure SS2. Only two studies discussed HIV infection separately (OR 4.28, 95% CI 1.98–9.24, P < 0.001, I2 = 0%). Four studies discussed solid organ tumor as a risk factor for mortality (OR 5.34, 95% CI 2.04–13.74, P = 0.003, I2 = 79%) (Figure S3. Alcohol abuse also increased mortality from IPD (OR 3.14, 95% CI 2.13–4.64, P < 0.001) (Figure S4).
Discussion
Despite the wide adoption of pneumococcal conjugate vaccination, the overall mortality rate from IPD has remained high, at 20.8%. This meta-analysis revealed older age (> 64 years old), septic shock, immunosuppressed status, underlying chronic diseases, solid organ tumor, alcohol abuse, nursing home, and nosocomial infection were prognostic factors for mortality from IPD. These results appear useful in understanding prognostic factors for mortality due to IPD because of the solid methodology in accordance with the MOOSE statement, with statistical power supported by more than 27,000 subjects.
Aging is a major risk factor for the development of virtually every lung disease, increasing both morbidity and mortality, while morbidities and mortalities from other prevalent diseases have declined or remained stable37. The conventional nuclear family model is becoming increasingly uncommon, and the majority of elder care is provided by relatives, albeit with varying patterns of involvement and responsibility across family structures38. Residence in a nursing home and nosocomial infection have been associated with the progression of aging. Comorbidity also plays an important role in affecting mortality. This study identified underlying chronic diseases, solid organ tumor, and immunosuppressed status as important factors to clinical progress.
Septic shock is a frequent complication of pneumococcal infection and causes high rates of morbidity and mortality39. The presence of septic shock on admission was the most strongly associated with risk of mortality among those factors. Unlike prognostic factors that cannot be changed, such as age, facility, and underlying diseases, outcomes might be improved with medical intervention for septic shock. Alcohol abuse is another preventable risk factor for pneumococcal disease, particularly among young adults40. This study also revealed alcohol abuse as a risk factor for mortality. Pneumococcal vaccination with PCV13 or PPV23 in adults is cost-effective and should be considered a priority for decision-makers41, and status of vaccination varied widely among studies (0–54.5%). Pneumonia vaccination was another effective means of preventing IPD, but much work remains to be done to increase the acceptance of pneumonia vaccination.
Limitations
Several limitations to this study must be considered when interpreting the results. Given the nature of the disease in question, only a limited number of prospective studies were able to be enrolled. There posed a substantial risk for selection bias, due to the nature of observational study and risk factors analyzed in this manuscript were selected post-hoc. Second, the definition of mortality in articles as in-hospital or 30-day mortality was merged together in some risk factors, due to limited numbers of articles. Third, prognostic factors for mortality differed markedly between articles. Fourth, the forms of vaccine status for studies included in this meta-analysis varied. Fifth, the effects of serotype and antibiotic resistance were not discussed in the present investigation.
Conclusion
IPD still shows high mortality rates and the presence of septic shock represents one of the most important prognostic factors for mortality in IPD. Unlike prognostic factors that cannot be changed, such as age, facility, and underlying diseases, early intervention for septic shock might improve the mortality in IPD.
References
Drijkoningen, J. J. & Rohde, G. G. Pneumococcal infection in adults: burden of disease. Clin. Microbiol. Infect. 20(Suppl 5), 45–51 (2014).
Centers for Disease Control and Prevention. ABCs Report: Streptococcus pneumoniae, 2018. https://www.cdc.gov/abcs/reports-findings/survreports/spneu18.html (2018).
Chalmers, J. D., Campling, J., Dicker, A., Woodhead, M. & Madhava, H. A systematic review of the burden of vaccine preventable pneumococcal disease in UK adults. BMC Pulm Med. 16, 77 (2016).
Bonnave, C. et al. Adult vaccination for pneumococcal disease: a comparison of the national guidelines in Europe. Europ. J. Clin. Microbiol. Infect. Dis Clin. Microbiol. Infect. 38, 785–791 (2019).
Marrie, T. J., Tyrrell, G. J., Majumdar, S. R. & Eurich, D. T. Effect of age on the manifestations and outcomes of invasive pneumococcal disease in adults. Am. J. Med. 131, 100e1-100e7 (2018).
Yu, V. L. et al. An international prospective study of pneumococcal bacteremia: correlation with in vitro resistance, antibiotics administered, and clinical outcome. Clin. Infect Dis. 37, 230–237 (2003).
Cooperative organization for national medical schools in Japan. University hospital Medical Information Network (UMIN) Center. Available at: https://www.umin.ac.jp/ctr/. Accessed 1st Mar (2020).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283, 2008–2012 (2000).
Bone, R. C. et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee American college of chest physicians/society of critical care medicine. Chest 101, 1644–1655 (1992).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25, 603–605 (2010).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Farinas-Alvarez, C. et al. Prognostic factors for pneumococcal bacteremia in a university hospital. Europ. J. Clin. Microbiol. Infect. Dis. Clin. Microbiol. Infect. 19, 733–741 (2000).
Kalin, M. et al. Prospective study of prognostic factors in community-acquired bacteremic pneumococcal disease in 5 countries. J. Infect. Dis. 182, 840–847 (2000).
Fernández Guerrero, M. L. et al. Bacteremic pneumococcal infections in immunocompromised patients without AIDS: the impact of beta-lactam resistance on mortality. Int. J. Infect. Dis. 7, 46–52 (2003).
Maugein, J. et al. Clinical and microbiological epidemiology of Streptococcus pneumoniae bacteremia in eight French counties. Clin. Microbiol. Infect. 9, 280–288 (2003).
Neuman, M. I., Kelley, M., Harper, M. B., File, T. M. Jr. & Camargo, C. A. Jr. Factors associated with antimicrobial resistance and mortality in pneumococcal bacteremia. J. Emerg. Med. 32, 349–357 (2007).
Alanee, S. R. et al. Association of serotypes of Streptococcus pneumoniae with disease severity and outcome in adults: an international study. Clin. Infect. Dis. 45, 46–51 (2007).
Lin, S. H. et al. Comparison of clinical features, antimicrobial susceptibility, serotype distribution and outcomes of patients with hospital- and community-associated invasive pneumococcal disease. Int. J. Antimicrob. Agents. 36, 119–123 (2010).
Lujan, M. et al. Influence of pneumococcal serotype group on outcome in adults with bacteraemic pneumonia. Eur. Respir. J. 36, 1073–1079 (2010).
Mooiweer, E., Luijk, B., Bonten, M. J. & Ekkelenkamp, M. B. C-Reactive protein levels but not CRP dynamics predict mortality in patients with pneumococcal pneumonia. J. Infect. 62, 314–316 (2011).
Song, J. S. et al. Risk factors for 30-day mortality in adult patients with pneumococcal bacteraemia, and the impact of antimicrobial resistance on clinical outcomes. Epidemiol. Infect. 140, 1267–1276 (2012).
Kang, C. I. et al. Association of levofloxacin resistance with mortality in adult patients with invasive pneumococcal diseases: a post hoc analysis of a prospective cohort. Infection 41, 151–157 (2013).
Suzuki, H. et al. Morbidity and mortality among newly hospitalized patients with community-acquired pneumococcal bacteremia: a retrospective cohort study in three teaching hospitals in Japan. Geriatr. Gerontol. Int. 13, 607–615 (2013).
Rudnick, W. et al. Pneumococcal vaccination programs and the burden of invasive pneumococcal disease in Ontario, Canada, 1995–2011. Vaccine. 31, 5863–5871 (2013).
Regev-Yochay, G. et al. A nationwide surveillance of invasive pneumococcal disease in adults in Israel before an expected effect of PCV7. Vaccine. 31, 2387–2394 (2013).
Cohen, C. et al. Streptococcus pneumoniae Serotypes and Mortality in adults and adolescents in South Africa: analysis of national surveillance data, 2003–2008. PLoS ONE 10, e0140185 (2015).
Hanada, S. et al. Host factors and biomarkers associated with poor outcomes in adults with invasive pneumococcal disease. PLoS ONE 11, e0147877 (2016).
Askim, A. et al. Epidemiology and outcome of sepsis in adult patients with Streptococcus pneumoniae infection in a Norwegian county 1993–2011: an observational study. BMC Infect. Dis. 16, 223 (2016).
Hughes, G. J., Wright, L. B., Chapman, K. E., Wilson, D. & Gorton, R. Serotype-specific differences in short- and longer-term mortality following invasive pneumococcal disease. Epidemiol. Infect. 144, 2654–2669 (2016).
Wagenvoort, G. H. et al. Risk and outcomes of invasive pneumococcal disease in adults with underlying conditions in the post-PCV7 era The Netherlands. Vaccine 34, 334–340 (2016).
Kim, J. H. et al. Adult invasive pneumococcal disease in the Republic of Korea: Risk medical conditions and mortality stratified by age group. Int. J. Infect. Dis. 74, 136–144 (2018).
Lee, H. Y. et al. Invasive pneumococcal disease caused by ceftriaxone-resistant Streptococcus pneumoniae in Taiwan. J. Microbiol. Immunol. Infect. 51, 500–509 (2018).
Regev-Yochay, G. et al. Pneumococcal meningitis in adults after introduction of PCV7 and PCV13, Israel, July 2009-June 2015(1). Emerg. Infect. Dis. 24, 1275–1284 (2018).
Houseman, C. et al. Decreasing case fatality rate following invasive pneumococcal disease, North East England, 2006–2016. Epidemiol 147, e175 (2019).
Lemay JA, Ricketson LJ, Zwicker L, Kellner JD. Homelessness in Adults with Invasive Pneumococcal Disease (IPD) in Calgary, Canada. Open Forum Infect Dis. 6, ofz362 (2019).
Man MY, Shum HP, Yu JSY, Wu A, Yan WW. Burden of pneumococcal disease: 8-year retrospective analysis from a single centre in Hong Kong. Hong Kong Med J. 26, 372-381 (2020).
Chen, H. et al. Declined functional status prolonged hospital stay for community-acquired pneumonia in seniors. Clin. Int. Aging. 15, 1513–1519 (2020).
Roberto, K. A. & Blieszner, R. Diverse family structures and the care of older persons. Can. J. Aging. 34, 305–320 (2015).
Garcia-Vidal, C. et al. Pneumococcal pneumonia presenting with septic shock: host- and pathogen-related factors and outcomes. Thorax 65, 77–81 (2010).
Grau, I. et al. Smoking and alcohol abuse are the most preventable risk factors for invasive pneumonia and other pneumococcal infections. Int. J. Infect. Dis. 25, 59–64 (2014).
Porchia, B. R., Bonanni, P., Bechini, A., Bonaccorsi, G. & Boccalini, S. Evaluating the costs and benefits of pneumococcal vaccination in adults. Exp. Rev. Vaccines. 16, 93–107 (2017).
Funding
None.
Author information
Authors and Affiliations
Contributions
H.C. conceived of and designed the study; H.C. and H.M. undertook comprehensive research; H.C., H.M., and N.H. analyzed the data; H.C., H.M., N.H., Y.H., N.K., and T.K. wrote and revised the paper. Y.H., N.K., and T.K. did critical reviews of the whole manuscript. All authors gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, H., Matsumoto, H., Horita, N. et al. Prognostic factors for mortality in invasive pneumococcal disease in adult: a system review and meta-analysis. Sci Rep 11, 11865 (2021). https://doi.org/10.1038/s41598-021-91234-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91234-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.