Abstract
Nausea and vomiting of pregnancy (NVP) is a common condition reported however inconclusively among pregnancies after assisted conception. The study objective was thus to explore whether NVP is associated to mode of conception or other in vitro fertilization (IVF)-related variables. This nested matched cohort study, originating from the BASIC-project, was conducted at the Uppsala University Hospital in Sweden between 2010 and 2016. IVF pregnancies (n = 210) and age and parity-matched women with spontaneous pregnancies (n = 420) comprised the study sample. The study outcome was self-reported NVP at gestational week 17. IVF treatment and pregnancy data were obtained after scrutinization of the medical records. NVP with or without medications was not associated with mode of conception (chi-square test, p = 0.889), even after adjusting for potential confounders. In a subgroup analysis among IVF pregnancies, NVP without medication was more frequently seen in the group who received cleavage stage embryos vs blastocysts (chi-square test, p = 0.019), exhibiting a marginally significant but strongly increased effect even after adjustment [crude RRR 3.82 (95% CI 1.23–11.92) and adjusted RRR 3.42 (95% CI 0.96–12.11)]. No difference in the rate of NVP with or without medication between women that underwent fresh and frozen/thawed embryo transfers as well as IVF or ICSI was observed. Conception through IVF is not associated with NVP. Transfer of a blastocyst may decrease the risk of developing NVP and further, large-scale prospective studies are required to validate this finding.
Similar content being viewed by others
Introduction
Nausea and vomiting of pregnancy (NVP) is one of the most common conditions during the gestational period1. Hyperemesis gravidarum (HG) is the most severe form of NVP, a pregnancy complication characterized by vomiting, excessive loss of body fluid, weight loss above 5% of pre-pregnancy body weight, electrolyte disturbances and ketonuria. HG usually emerges in 0.3–3.6% of all pregnancies1, whereas NVP may affect as much as 35–91% of pregnant women1 and may have severe consequences on maternal and offspring well-being as well as the healthcare system2,3,4,5. Although the exact cause of NVP and HG remains unknown, several hypotheses have been proposed indicating a multifactorial etiology. Some studies have examined the potential involvement of a Helicobacter pylori infection during pregnancy6, while others focused on the role of elevated estrogens7 and human chorionic gonadotropin (hCG) levels in HG-affected pregnancies8; however, study findings still remain controversial. Risk factors associated to increased risk for HG are thought to be prior history of HG9, young age at pregnancy, primiparity, carrying a female fetus, black or Asian ethnic origin, parathyroid or thyroid dysfunction, and diabetes mellitus type 110.
Pregnancy-related nausea and vomiting, including hyperemesis gravidarum may be accompanied by maternal physical and psychological distress both on the short but also on the long run. Women who are not able to manage excessive stress during pregnancy, depending on either the pregnancy itself as a stressful condition or anxiety due to other reasons such as earlier trauma, may tend to avoid the intolerable situation, by somatization of distress to gastrointestinal symptoms such as nausea and vomiting11. In particular, a higher prevalence of sleep disorders, post-traumatic stress disorder, depression, and anxiety in women suffering from prolonged NVP and HG has been demonstrated12,13,14,15. On the other side, psychiatric manifestations including higher level of anxiety have been reported among infertile couples compared to fertile couples16. Individuals that undergo treatment with assisted reproductive technologies (ART) including IVF are unsurprisingly distressed and depressed due to both infertility and uncertainty about the treatment and its results17. In fact, it has been demonstrated that women who underwent IVF-treatment experienced more psychological stress and anxiety compared to women with spontaneous pregnancies18,19 as well as greater controlling parenting behaviors and emotional bond to the child19,20.
Currently, the studies concerning NVP and HG that include IVF populations are limited and with inconclusive findings. One of these studies evaluated the prevalence of NVP in singleton and twin IVF pregnancies and demonstrated an increased NVP risk in the first trimester of pregnancy among twin but not singleton pregnancies21. Two other studies explored maternal characteristics among pregnant women with HG in order to estimate the incidence of the condition and identify related risk factors and reported increased risk for HG in ART conceived pregnancies22,23. However, the vast majority of studies included a mixed study population comprising pregnancies conceived after IVF, ovarian stimulation or intrauterine insemination, and focused mostly on HG instead of NVP. The question thus of whether there is an association between IVF and NVP remains unanswered.
The primary aim of the present study was therefore to explore the association between mode of conception, IVF or spontaneous, and NVP in a prospective cohort of pregnant women receiving prenatal care at a Swedish University Hospital. Our secondary aim was to explore whether different IVF modalities including fertilization method, fresh or frozen-thawed embryo transferred, and stage of transferred embryo differ regarding the occurrence of NVP.
Materials and methods
Study population
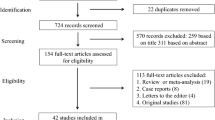
The study design is that of a nested matched cohort study originating from the BASIC study. The BASIC-study is a population-based longitudinal study investigating biological correlates of mood and anxiety disorders during pregnancy and the postpartum period24, conducted at the department of Obstetrics and Gynecology at Uppsala University Hospital in Sweden between 2010 and 2019. For the present sub-study, approximately 3200 pregnancies were included between January 2010 and September 2016.
All women attending the routine ultrasound examination around gestational week 17 in Uppsala County were invited to participate in the project. Upon invitation, written and oral information was given, and written consent was obtained from women who chose to participate. A self-administered structured questionnaire containing questions on personal history, sociodemographic data and variables related to pregnancy was filled in upon inclusion. Exclusion criteria were: (1) women whose personal data were protected, (2) women who had pathologic pregnancies diagnosed during the routine ultrasound, (3) women who were unable to communicate adequately in Swedish and (4) women younger than 18 years old. About 22% of pregnant women in Uppsala County participated in the project. For the particular matched cohort study further exclusion criteria comprised twin pregnancies and pregnancies conceived through egg donation.
Exposure
All participating women in the BASIC cohort were asked upon enrollment whether they had conceived through fertility treatment or not. In case of fertility treatment, further information was collected by scrutinizing the participants’ medical records. In total, 210 women who had undergone IVF/ICSI (intracytoplasmic sperm injection) treatment preceding the index pregnancy comprised the exposed group. Two, for each case, age and parity-matched women with spontaneously conceived pregnancies without history of infertility, were randomly selected from the BASIC cohort and comprised the non-exposed group (n = 420).
Outcome
The main outcome of the study, NVP at GW17, was divided into three groups: (1) absence of NVP, (2) NVP without medication, and (3) NVP with medication. To assess NVP severity, use of antiemetic drugs was utilized as a proxy. NVP was assessed by asking women whether they experienced any kind of nausea in the index pregnancy at GW 17; “Have you experienced any nausea during this pregnancy?” (yes/no), and “Did you receive any medication against nausea of pregnancy?” (yes/no).
Covariates
Information about sociodemographic and pregnancy related characteristics was gathered upon inclusion through questionnaires; age at delivery (years), body mass index (BMI) before pregnancy (kg/m2), parity (primiparity/multiparity), education level (university/secondary school or lower), employment status (full-time or part-time job, studies/maternal leave, sick leave/unemployment), smoking before pregnancy (no/yes), alcohol consumption three months before pregnancy (never/at least once a week/more than once a week), chewing tobacco right before pregnancy (no/yes), depression history (previous depression/contact with psychiatrist or not), delivery fear (no/yes), comorbidities (i.e. migraine, hypertension, diabetes, metabolic disease, allergy, irritable bowel syndrome, alcohol/drug addiction, chronic pain or other disease), and gender of the newborn (male/female). IVF-treatment related information was also recorded such as infertility diagnosis (unexplained/male factor/tubal factor/anovulation/endometriosis/other), male infertility (no/yes), method of conception (IVF/ICSI/combined IVF and ICSI), fresh/frozen-thawed treatments, stage of embryo transferred (cleavage stage/blastocyst), main medicine during IVF treatment (recombinant-FSH or human menopausal used in fresh cycles/hormone replacement therapy or unstimulated cycle used in frozen thawed cycles), ovarian hyperstimulation syndrome (OHSS) in fresh IVF cycles (no/yes), sperm donation (no/yes), number of prior IVF stimulations (1, 2, 3 or more), number of prior embryo transfers (1, 2, 3 or more), number of embryos simultaneously transferred (single/double embryo transfer).
Statistics
Analyses were carried out with the Statistical Package for the Social Sciences (IBM SPSS Statistics, version 26) and the level of statistical significance was set at 0.05. Maternal characteristics were first tested for normality. Univariate differences in sociodemographic data between exposed and non-exposed group were examined by using chi-square test for categorical variables and the Mann–Whitney U-test for continuous variables. To assess differences in sociodemographic and pregnancy-related data between NVP groups, in the entire study population as well as in the exposed group only, the chi-square test was utilized for categorical variables and the Kruskal–Wallis test for continuous variables. Furthermore, NVP and IVF-modalities were further explored in a subgroup analysis comprising only the exposed group. A multinomial logistic regression analysis was performed first on the entire study population, with NVP as the dependent variable and mode of conception as the independent variable. Relative Risk Ratios (RRR) and 95% Confidence Intervals (95% CI) before and after adjustment for possible confounders were calculated. Women having conceived spontaneously constituted the reference group. The covariates for adjustment were selected a priori based on background knowledge and were further assessed with a Directed Acyclic Graph (DAG) (Supplementary Figure). We regarded employment status and education level both as equal proxies of the individual socioeconomic status, and therefore chose only one variable to include in the DAG and multinomial logistic regression model (i.e., education level). Furthermore, chewing tobacco was not adjusted for due to the great overlap with smoking and to the high rate of missingness (i.e., 54.8%). As a result, the covariates included in the model were: BMI before pregnancy, education level, smoking before pregnancy, alcohol consumption three months before pregnancy, depression history and comorbidities. Further, in the subgroup of exposed women, the effect of IVF modalities on NVP was explored in multinomial logistic regression analysis; the independent variable studied was selected based on statistically significant results of univariate analyses. The multivariate model included all the covariates described above, as well as age at delivery and parity. Lastly, we performed a sensitivity analysis by excluding treatments performed with the use of donated sperm and explored the exposure groups in relation to the study outcome.
Ethical approval
The study was approved by the Regional Ethical Review Board in Uppsala (Dnr 2009/171), part of the national Swedish ethical review authority. All research was performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all the participants.
Results
Table 1 presents sociodemographic and pregnancy-related characteristics in IVF pregnancies and matched spontaneous conceptions. The median age at delivery of the study population was 34.0 years old and 2/3 of study participants were primipara. Compared to spontaneous pregnancies, women who conceived through IVF reported less frequently alcohol consumption before pregnancy (38.4% vs 48.7%, p = 0.032), but more frequently comorbidities (59.1% vs 49.9%, p = 0.029). The vast majority of study participants had a university degree (83.9%). No other differences on sociodemographic and clinical characteristics were observed between the two groups.
Table 2 presents sociodemographic and pregnancy-related characteristics of the study sample by nausea group. NVP, with or without medication, was not associated with mode of conception (p = 0.889). A higher percentage of women without NVP were primipara compared to women with NVP either requiring medication or not (80.5% vs. 60.9% vs. 62.3%, p < 0.001). A higher proportion of women with NVP requiring medication or not reported history of depression compared to women in the non-NVP group (69.6% and 63.4% vs. 46.2%, p < 0.001). Lastly, a lower percentage of women with NVP not requiring medication reported smoking before pregnancy in comparison to the other outcome groups. After performing a multinomial logistic regression analysis, it was confirmed that the association between mode of conception and NVP severity was not statistically significant; women conceiving through IVF exhibited a crude relative risk ratio (RRR) of 0.92 (95% CI 0.63–1.36) for NVP without medication and a crude RRR of 1.01 (95% CI 0.56–1.83) for NVP with medication, relative to spontaneously conceiving women. The associations remained unchanged even after adjustment for various covariates (i.e., the likelihood of suffering from NVP without medication and NVP with medication among women conceiving with IVF were adjusted RRR 0.69 (95% CI 0.37–1.29) and adjusted RRR 0.78 (95% CI 0.28–2.16), respectively, compared to women conceiving spontaneously given that the other covariates were held constant).
Table 3 presents pregnancy and IVF-treatment characteristics in relation to NVP in the exposed group. We could not find any significant difference in the rate of NVP with or without medication between women that underwent fresh and frozen/thawed embryo transfers or in the prevalence of OHSS in fresh IVF cycles. The same applied when testing differences between NVP groups in relation to fertilization by IVF or ICSI. However, we observed a significant difference between embryo stage and the study outcome; women with NVP non-requiring medication had received more often cleavage stage embryos compared to women without NVP and women with NVP requiring medication (93.5% vs. 78.9% vs. 75.0%, p = 0.019). All findings remained unchanged after the sensitivity analysis performed. Lastly, we calculated the effect estimate of embryo stage on NVP. It was estimated that the relative risk for NVP without medication of cleavage stage embryos relative to blastocysts was increased by a factor of 3.82 and 3.42, before and after the adjustment for relevant covariates [i.e., crude RRR 3.82 (95% CI 1.23–11.92) and adjusted RRR 3.42 (95% CI 0.96–12.11) respectively].
Discussion
Main findings and comparison to other studies
In the present study, no significant association between mode of conception and NVP could be demonstrated. Furthermore, NVP was not associated to different IVF modalities such as fertilization method, stimulation protocol, or use of cryopreservation. On the contrary, the developmental stage of the embryo transferred was associated with the occurrence of NVP since NVP without medication was more often present in pregnancies after cleavage stage embryo transfer.
Similar findings were reported in the study by Bordi et al.25 who assessed the effects of ART on maternal and perinatal outcomes in twin pregnancies. In this study, no significant difference in the prevalence of HG between ART and spontaneous pregnancies was observed. However, this study had HG and not NVP as main study outcome. On the contrary, Roseboom et al.23, demonstrated a higher rate of ART conceived pregnancies among women suffering from HG, while Nurmi et al.22, found an increased incidence of HG among ART conceived pregnancies. However, both studies comprised ART pregnancies which included IVF and other assisted reproductive techniques besides IVF, while only IVF-conceived pregnancies were included in our study. Subsequently, a mixed population could affect the interpretation of the findings, since it is unclear whether the observed association is due to the impact of infertility or due to the treatment method. Furthermore, our study assessed the whole spectrum of NVP and was not restricted to women with HG. These differences in study design may partly explain the different results observed.
Interestingly, the rate of NVP not requiring medication in our study was higher among pregnancies after cleavage stage embryo transfer compared to pregnancies resulting from blastocyst transfer. In the IVF treated group, information about the stage of embryo transferred was available for 146 women, the majority of whom had received cleavage-stage embryos (n = 128, 87.7%). The rate of blastocyst transfers during that period was lower compared to current trends. It is however in agreement with the global trend during that period. In accordance with our data, national statistics of treatments performed in Sweden in 2012 demonstrated that 87.4% of fresh transfers and 62.7% of frozen transfers were done with embryos in cleavage stage, which have thereafter gradually been replaced by blastocysts, first in frozen-thawed and afterwards even in fresh cycles. In 2016, the percentage of cleavage stage embryos transferred was 74% for fresh and 18% for frozen-thawed cycles26. Nevertheless, this finding should be interpreted with caution due to the missing rate of information and the low rate of blastocyst transfers during that time-period.
Mechanisms proposed behind the development of NVP comprise the presence of an on-going gastric H-pylori infection6, as well as increased levels of hCG and estradiol27. In particular, higher levels of hCG positively correlate with NVP incidence, an association that has been consistently reported in molar and multiple gestations27. The hCG-vomiting effect has been attributed to a stimulatory effect of the upper gastrointestinal tract secretions7 and a triggering of the nausea and vomiting reflex in the brain stem28. The association between hCG and NVP could not however be verified by all studies probably due to variation in either the biologic activity of hCG or the individual susceptibility to the hCG hormone27. Concerning estradiol, the mechanism associating it to HG is thought to be mediated by the increased gastric fluid content and slower gastrointestinal transit which may exacerbate nausea and vomiting7. In fact, cigarette smoking during pregnancy is associated with lower levels of hCG and estradiol29, and it is thus not surprising that a lower rate of self-reported NVP without medications has been observed among smokers in our study.
Strengths and limitations
The population-based prospective design and the large number of background variables constitute the main strengths of this study. Furthermore, the utilization of two age and parity matched controls for each exposed woman originating from the same cohort is also a strength of the study. We chose to match the two groups for age and parity since both younger age and nulliparity have been consistently reported as risk factors for NVP10,22,30. Additionally, only IVF treated women were included in order to increase the specificity of the findings.
The self-reported information regarding the outcome and a number of covariates should be considered as a limitation, along with a higher missing rate on certain IVF-related variables. Moreover, a larger study sample could have contributed to an even better study power, especially when examining IVF characteristics in the exposed group. Since no prior reports existed regarding the occurrence of NVP in IVF treated women, no power calculation could be performed a priori. The latter explains why this study should be treated as an exploratory study in the field. Regarding classification of NVP into subgroups, it should be kept in mind that, despite our attempt to assess disease severity based on antiemetic medication use, other aspects such as psychological factors may influence the woman’s self-perceived symptoms27. The higher education of participants in the BASIC project, compared with those residing in Uppsala County, as well as the relatively low participation rate in the BASIC study should be taken into account in terms of generalizability of study results.
Conclusion
Conception mode was not associated with NVP development in our study. Interestingly, cleavage stage embryo transfer was associated with a higher occurrence of NVP without medication. The developmental stage of the transferred embryo may therefore affect NVP development and should be thus taken into account when planning an IVF treatment cycle, especially among women with prior NVP history. Future research with large-scale studies is needed in order to validate our study findings and further examine the possible effect of transferred embryo stage on NVP.
Data availability
The data that support the findings of this study are available upon reasonable request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.
References
Einarson, T. R., Piwko, C. & Koren, G. Quantifying the global rates of nausea and vomiting of pregnancy: A meta analysis. J. Popul. Ther. Clin. Pharmacol. 20, e171-183 (2013).
Erick, M., Cox, J. T. & Mogensen, K. M. ACOG Practice Bulletin 189: Nausea and vomiting of pregnancy. Obstet. Gynecol. 131, 935 (2018).
Gazmararian, J. A. et al. Hospitalizations during pregnancy among managed care enrollees. Obstet. Gynecol. 100, 94–100 (2002).
Gargollo, P. C. & Jayanthi, R. Great expectations: The dream versus the reality of urinary continence and bladder exstrophy. J. Urol. 203, 46–47 (2020).
Havnen, G. C. et al. Women’s perspectives on the management and consequences of hyperemesis gravidarum—A descriptive interview study. Scand. J. Prim. Health Care 37, 30–40 (2019).
Li, L. et al. Helicobacter pylori infection is associated with an increased risk of hyperemesis gravidarum: A meta-analysis. Gastroenterol. Res. Pract. 2015, 278905 (2015).
Verberg, M. F. G., Gillott, D. J., Al-Fardan, N. & Grudzinskas, J. G. Hyperemesis gravidarum, a literature review. Hum. Reprod. Update 11, 527–539 (2005).
Derbent, A. U. et al. First trimester maternal serum PAPP-A and free β-HCG levels in hyperemesis gravidarum. Prenat. Diagn. 31, 450–453 (2011).
Agmon, N., Sade, S., Pariente, G., Rotem, R. & Weintraub, A. Y. Hyperemesis gravidarum and adverse pregnancy outcomes. Arch. Gynecol. Obstet. 300, 347–353 (2019).
Fiaschi, L., Nelson-Piercy, C. & Tata, L. J. Hospital admission for hyperemesis gravidarum: A nationwide study of occurrence, reoccurrence and risk factors among 8.2 million pregnancies. Hum. Reprod. 31, 1675–1684 (2016).
Buckwalter, J. G. & Simpson, S. W. Psychological factors in the etiology and treatment of severe nausea and vomiting in pregnancy. Am. J. Obstet. Gynecol. 186, S210-214 (2002).
Kjeldgaard, H. K., Eberhard-Gran, M., Benth, J. Š & Vikanes, Å. V. Hyperemesis gravidarum and the risk of emotional distress during and after pregnancy. Arch. Womens Ment. Health 20, 747–756 (2017).
Iliadis, S. I., Axfors, C., Johansson, S., Skalkidou, A. & Mulic-Lutvica, A. Women with prolonged nausea in pregnancy have increased risk for depressive symptoms postpartum. Sci. Rep. 8, 15796 (2018).
Yıldırım, E. & Demir, E. The relationship of hyperemesis gravidarum with sleep disorders, anxiety and depression. J. Obstet. Gynaecol. 39, 793–798 (2019).
Mitchell-Jones, N. et al. Psychological morbidity associated with hyperemesis gravidarum: A systematic review and meta-analysis. BJOG 124, 20–30 (2017).
Fallahzadeh, H., Zareei Mahmood Abadi, H., Momayyezi, M., Malaki Moghadam, H. & Keyghobadi, N. The comparison of depression and anxiety between fertile and infertile couples: A meta-analysis study. Int. J. Reprod. Biomed. (Yazd.) 17, 153–162 (2019).
Mahlstedt, P. P. The psychological component of infertility. Fertil. Steril. 43, 335–346 (1985).
Shih, F.-F. et al. Comparison of pregnancy stress between in vitro fertilization/embryo transfer and spontaneous pregnancy in women during early pregnancy. J. Nurs. Res. 23, 280–289 (2015).
McMahon, C. A. et al. Age at first birth, mode of conception and psychological wellbeing in pregnancy: Findings from the parental age and transition to parenthood Australia (PATPA) study. Hum. Reprod. 26, 1389–1398 (2011).
Wang, Y.-M., Shu, B.-C., Fetzer, S. & Chang, Y.-J. Parenting style of women who conceived using in vitro fertilization: A meta-analysis. J. Nurs. Res. 22, 69–80 (2014).
Jahangiri, F. et al. Correlation between depression, anxiety, and nausea and vomiting during pregnancy in an in vitro fertilization population: A pilot study. J. Psychosom. Obstet. Gynaecol. 32, 113–118 (2011).
Nurmi, M., Rautava, P., Gissler, M., Vahlberg, T. & Polo-Kantola, P. Incidence and risk factors of hyperemesis gravidarum: A national register-based study in Finland, 2005–2017. Acta Obstet. Gynecol. Scand. https://doi.org/10.1111/aogs.13820 (2020).
Roseboom, T. J., Ravelli, A. C. J., van der Post, J. A. & Painter, R. C. Maternal characteristics largely explain poor pregnancy outcome after hyperemesis gravidarum. Eur. J. Obstet. Gynecol. Reprod. Biol. 156, 56–59 (2011).
Axfors, C. et al. Cohort profile: The Biology, Affect, Stress, Imaging and Cognition (BASIC) study on perinatal depression in a population-based Swedish cohort. BMJ Open 9, e031514 (2019).
Bordi, G. et al. The influence of ovulation induction and assisted conception on maternal and perinatal outcomes of twin pregnancies. Eur. Rev. Med. Pharmacol. Sci. 21, 3998–4006 (2017).
Q-IVF—Årsrapporter. https://www.medscinet.com/qivf/arsrapporter.aspx. Accessed 11 Mar 2020.
Chandra, K. K., Magee, L. L. & Koren, G. G. Discordance between physical symptoms versus perception of severity by women with nausea and vomiting in pregnancy (NVP). BMC Pregnancy Childbirth 2, 5 (2002).
Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 189: Nausea and vomiting of pregnancy. Obstet. Gynecol. 131, e15–e30 (2018).
Tan, P. C., Tan, N. C. & Omar, S. Z. Effect of high levels of human chorionic gonadotropin and estradiol on the severity of hyperemesis gravidarum. Clin. Chem. Lab. Med. 47, 165–171 (2009).
Ioannidou, P., Papanikolaou, D., Mikos, T., Mastorakos, G. & Goulis, D. G. Predictive factors of hyperemesis gravidarum: A systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 238, 178–187 (2019).
Acknowledgements
We would like to thank the statistician Natasa Kollia for her invaluable support regarding the selection of the study population.
Funding
Open access funding provided by Uppsala University. The authors received no specific funding for this work. However, the BASIC study was supported by the Swedish Research Council (Grant numbers 523-2014-2342, 523-2014-07605 and 521-2013-2339) and the Uppsala University Hospital. EE has a part-time research position funded by Uppsala University Hospital (Grant no. ALF 1040530/2019). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
F.B. and E.E. have contributed to the conception and design of the study, acquisition, analysis and interpretation of data, and have drafted and revised the article for important intellectual content. S.I. has contributed to acquisition and interpretation of data and has revised the article for important intellectual content. All authors have approved the submitted version of the article to be published.
Corresponding author
Ethics declarations
Competing interests
EE has received lecture fee from Gedeon Richter and research grant from Ferring outside the submitted work. The other authors have no conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bazargani, F., Iliadis, S.I. & Elenis, E. Mode of conception in relation to nausea and vomiting of pregnancy: a nested matched cohort study in Sweden. Sci Rep 11, 9039 (2021). https://doi.org/10.1038/s41598-021-88575-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88575-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.