Abstract
Left ventricular hypertrophy (LVH) is considered a cardiac condition with life-threatening complications. Detected LVH is a strong predictor of cardiovascular diseases and death. This condition is normally diagnosed at offices. We aimed to determine the prevalence and associated factors of electrocardiographic-LVH (ECG-LVH) among adults in a Thai rural community. A cross-sectional study was conducted in Na-Yao rural community of Thailand in 2020. A total of 638 individuals aged ≥ 20 years were interviewed using standardized structured questionnaires related to demographic information, risk behaviors, comorbidities and anthropometric measurements. LVH was determined by Sokolov-Lyon and Cornell criteria based on the collected electrocardiograms. The prevalence of ECG-LVH among adults was 6.6%. The factors independently associated with ECG-LVH were being male (AORs 2.04, 95% CI 1.05–3.98), history of diabetes mellitus (AORs 1.01, 95% CI 1.01–1.02), and hypertensive crisis ≥ 180/110 mmHg (AORs 7.24, 95% CI 1.31–39.92). However, resting heart rate was negatively associated with ECG-LVH (p < 0.05). Our data emphasized that LVH was one of the significant health problems among adults in a rural community. This condition could lead to severe complications. Thus, effective detection and public health interventions should be provided at the community level.
Similar content being viewed by others
Introduction
Left ventricular hypertrophy (LVH) is considered a cardiac condition secondary to both structural and functional adaptation of the heart leading to many life-threatening complications like myocardial ischemia, left ventricular (LV) dysfunction, heart failure and even sudden cardiac death1,2,3,4. Several studies reported that the potential risk factors of LVH included being male5,6, high blood pressure7,8, insulin resistance9 and obesity10. Detecting and monitoring LVH, a strong predictor of cardiovascular diseases and death11, is crucial. Regression of LVH could reduce the risk of adverse outcomes12.
Approximately one half of the Thai population resides in rural areas where the characteristics of healthcare infrastructure and providers differ from those of urban settings especially in remote rural areas. In Thailand, a related study among adults in an urban setting in 2000 reported a prevalence of LVH at approximately 13%13. However, only limited information is available on the prevalence of and factors potentially responsible for LVH among adults in remote rural communities. The required information is essential to focus on preventing problems. Even though echocardiography is a gold standard to detect LVH, the technology is unavailable to use in those remote areas and also requires more specialists to complete the process. However, ECG criteria for LVH have been illustrated as strong independent predictors of cardiovascular morbidity and mortality in the general population3,14. Thus, this study aimed to determine the prevalence and associated factors of electrocardiographic-LVH (ECG-LVH) among adults in a remote rural community in central Thailand.
Methods
Study designs and subjects
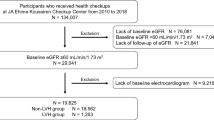
The study was conducted in a remote rural area, 150 km from Bangkok: Na-Ngam community at the border area of Chachoengsao Province, central Thailand. The remote rural community houses approximately 3500 adults. A cross-sectional survey was conducted between January and February 2020. Information on people in the rural area was retrieved from the National Population Registry to determine the sampling frame. The registered population was selected using a random sampling which proportionated about 20% of population. The individuals residing in the area during the study were included. The inclusion criteria comprised adults aged at least 20 years old. Subjects were excluded from the study if they were pregnant (or suspected) or could not answer the questionnaires.
Data collection
The investigators provided information sheets and informed subjects of the objectives and methods of the study including the interview questionnaire and ECG test. Written informed consent was obtained before conducting the study. When subjects could not read the information sheet, the investigators would read and describe the information to them. Additionally, subjects could use their fingerprint on the consent form to confirm their agreement. The duration of the questionnaire process, ECG testing and anthropometric measurement was approximately 30 min. Face-to-face interviews were performed using standardized questionnaires provided by well-trained interviewers. The questionnaire, used to identify the associated factors of ECG-LVH among adults in a rural community, covered information on demographic characteristics and self-reported comorbidity including history of hypertension (HT) and history of diabetes mellitus (DM), smoking and alcohol consumption. Smoking status was divided in three categories including current smoker, exsmoker and never15.
Measurements
Body weight and height were measured using body composition monitor (OMRON model HBF-212, Kyoto, Japan) and stadiometer (DETECTO, St. Webb City, MO, USA), respectively. Body mass index (BMI) was categorized according to the Asia–Pacific BMI classifications, i.e., < 18.5 kg/m2, 18.5 to 22.9 kg/m2, 23.0 to 24.9 kg/m2, 25.0 to 29.9 kg/m2 and ≥ 30 kg/m216. The participants stood on the floor with Frankfort horizontal plane17, then neck circumference was measured at midway between the midcervical spine and midanterior neck to within 1 mm, with a plastic tape18. Neck circumference was categorized in two groups, i.e., ≥ 35.75 cm (men), ≥ 32.75 cm (women), < 35.75 cm (men) and < 32.75 cm (women)19. Blood pressure was measured using an automatic blood pressure monitor (OMRON, HEM-7120, Kyoto, Japan) by an operator trained in standardized technique following the 2019 Thai guidelines on the treatment of HT20. The participants were advised to avoid caffeine and smoking for at least 30 min before the measurement was performed. The participants were instructed to be stationary at least 5 min in a chair, with feet on the floor and arms supported at heart level. During the measurement, talking was prohibited. Two measurements were taken, and the average was recorded.
Procedure for recording a standard 12-lead electrocardiography was conducted by well-trained investigators using a Digital 3-channel Color Electrocardiograph (Model: EKG-903A3, Beijing, PR China). The participants were asked to lie down in a comfortable position in a private partition room. The head was well-supported, the back rested on the bed and pillows. The inner aspects of the participants’ wrists were placed close to, but not touching, their waist. The investigator applied the limb leads at both wrists and ankles of the participants, then applied the chest leads; V1 to V6. The calibration signal on the ECG machine was checked to ensure standardization as a paper speed of 25 mm/s and ECG size 1 mV/10 mm deflection21. The participants were asked to lie still and to breathe normally during the measurement. The 12-lead ECG was recorded and correctly labeled within the identification number.
ECG-LVH was defined as a Sokolow-Lyon voltage (SV1 + RV5/6) > 35 mm22, and the Cornell voltage criterion-based LVH was defined as R in aVL + SV3 ≥ 28 mm for men S in V3 + R in aVL > 20 mm for women23,24. The ECG was reviewed, interpreted, and results were confirmed by cardiologists of Phramongkutklao Hospital in Bangkok.
The participants received the results, descriptions of their ECG test and the recommendation of self-health management. The participants presenting ECG-LVH and other abnormal ECG would receive standard care under their healthcare coverage scheme. The list of participants with ECG-LVH and other abnormal ECG patterns was registered in the health database at the Health Promoting Hospital, the primary care unit in Na-Yao rural community.
Ethics consideration
This study was reviewed and approved by the Institutional Review Board, Royal Thai Army Medical Department, approval number R155q/62. The participants consented in agreement with the WMA Declaration of Helsinki–Ethical principles for medical research involving human subjects.
Statistical analysis
Demographic characteristics were determined using descriptive statistics. Prevalence of ECG-LVH was determined using descriptive statistics and reported as a percentage with 95% confidence interval (CI). Binary logistic regression analysis was used to determine the associated factors of ECG-LVH, and multicollinearity was tested. Multivariate logistic regression analysis was performed; then adjusted odds ratio (AOR) was presented with corresponding 95% CI. A p-value less than 0.05 was considered statistically significant. Data were analyzed using StataCorp. 2019, Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC.
Results
Characteristics of study participants
A total of 638 adults residing in a rural community were enrolled in the present study. Of all participants, 198 (31.1%) were male. The average age of the participants was 56.9 ± 13.0 years. Most participants obtained their highest education level from primary school accounting for 69.3%. In all, 560 (87.8%) applied the universal health coverage scheme. In terms of comorbidities, 37.9 and 11.1% of participants reported having a history of HT and DM, respectively. Average BMI among all study participants was 25.0 ± 4.4 kg/m2. Demographics of the study participants are presented in Table 1.
Prevalence of ECG-LVH among adults in a Thai rural community
A total of 42 adults (6.6%, 95% CI 4.7% to 8.5%) were identified to have ECG-LVH. The prevalence of ECG-LVH among males was 10.7% (95% CI 6.3–15.0%) while the prevalence was 4.8% (95% CI 2.8–6.8%) among females. The prevalence of ECG-LVH was 7.0% (95% CI 3.8 to 10.3%) and 11.4% (95% CI 3.7 to 19.1%) among adults reporting a history of HT and DM, respectively.
Factors associated with ECG-LVH among adults in a Thai rural community
Table 2 shows the univariate logistic regression analysis for factors associated with ECG-LVH among adults in this community. After adjusting for potential confounders, factors independently associated with ECG-LVH were identified and presented in Table 3. Male participants were associated with ECG-LVH (AOR 2.0, 95% CI 1.1 to 4.0). Participants reporting a history of DM were associated with ECG-LVH (AOR 1.01, 95% CI 1.01 to 1.02). Our findings indicated that adults with high blood pressure level revealing hypertensive crisis (SBP ≥ 180 mmHg or DBP ≥ 110 mmHg) were associated with ECG-LVH (AOR 7.2, 95% CI 1.3 to 39.9). A dose response relationship between resting heart rate (HR) and negative association with ECG-LVH was identified (p < 0.05). An increase in neck circumference tended to relate to ECG-LVH; however, without association (AOR 1.6, 95% CI 0.8–3.2).
Discussion
Our data demonstrated the prevalence of ECG-LVH among adults residing in a Thai rural community was 6.6%. ECG-LVH was significantly associated with being male, history of DM, hypertensive crisis (SBP ≥ 180 mmHg, DBP ≥ 110 mmHg) and resting HR. To our knowledge, this was the first report on the prevalence and risk factors of ECG-LVH in a general Thai populations residing in a rural community. The prevalence of ECG-LVH among participants in the present study was relatively low when compared with other reports in both rural and urban settings. A related study among Thai people aged ≥ 30 years in an urban area in 2000 reported that the prevalence of ECG-LVH was 13%13. However, the prevalence of ECG-LVH among adults in a rural farm setting in Rivers State of Nigeria was 16.4%5. These wide gaps from the present study may be related to the fact that African populations tended to have a high ventricular mass when compared with other ethnics25.
Our finding reported that the prevalence of ECG-LVH among males was significantly higher than that identified among females. This finding was compatible with other related studies5,6,7,13; however, other studies reported a higher prevalence of ECG-LVH among females26. Although being male was an associated risk factor for ECG-LVH, LVH was a greater risk factor for cardiac death among females than among males27. Strong evidence was observed that ECG-LVH was a risk predictor of cardiovascular events including coronary heart disease, stroke and sudden cardiac death2,3,8,28,29,30. When LVH continued to progress, the prevalence of patients with cardiovascular diseases and their complications were more likely to increase. Thus, early detection, prevention and treatment of modifiable cardiovascular risk factors in a general population residing in a community should be implemented as effective interventions.
We found that study participants reported a history of DM related to ECG-LVH. Similarly, the NOMAS cohort study among a multi-ethnic population in the US showed that DM was independently associated with increased risk of LVH25. One recent study in the UK demonstrated a relationship existed between cardiac steatosis and LV geometric remodeling among patients with DM; however, the causality of this relationship will need to be investigated in the future4. Furthermore, related studies using murine models reported that cardiac steatosis, where superfluous triglyceride accumulates in the myocyte, led to cardiomyopathy31,32.
Regarding related reports in a rural community7,33, we found that ECG-LVH was linked to high blood pressure level, especially SBP ≥ 180 mmHg or DBP ≥ 110 mmHg. The finding was consistent with the related study of Tangjatuporn et al. reporting that 20% of patients with uncontrolled blood pressure were identified as presenting ECG-LVH7. Our study revealed that adults with high blood pressure as hypertensive crisis had a strong risk associated with ECG-LVH (AOR 7.2, 95% CI 1.3 to 39.9). High blood pressure increases LV wall stress triggering both neurohumoral activation and mechanical stress pathways. When these processes are not prohibited, hypertensive heart disease including cardiac arrythmias, heat failure and coronary heart disease will occur34,35. Furthermore, we found that 6 (75%) of a total of 8 participants with hypertensive crisis were unaware of HT. Our data suggested that effective community interventions such as HT screening and modified risk factors of uncontrolled blood pressure among adults with HT should be provided in rural settings19.
Related evidence has demonstrated that resting HR is a predictor of cardiovascular events including death36,37. However, our study reported that resting HR was negatively associated with ECG-LVH, significantly. Similarly, related studies in Egypt and Greece reported that LVH was reversely related to HR38,39. Additionally, the finding from the OGHMA study in Japan reported that each 10 beats/min increase in resting HR was associated with reduced development of ECG-LVH, especially among males40. Nevertheless, the temporal relationship between resting HR and developing ECG-LVH in the present study could not be proved due to the cross-sectional design.
The study employed a cross-sectional survey which could make it difficult to establish a cause-and-effect relationship between associated factors and ECG-LVH. Another limitation was the small sample size in the study; thus, the association between the well-known risk factors such as obesity and outcome could not be presented. When the study was conducted, the young adults especially those aged less than 40 years were unavailable to participate because most people in this age group (20 to 39 years) worked in the other areas. Thus, the prevalence of ECG-LVH in this community may have been overestimated. However, social desirability bias might also have existed in the study due to face-to-face interview, although the interviewers were well-trained and used standardized surveys.
The study identified a few modifiable risk factors for ECG-LVH which would be advantageous implementing prevention strategies at the community level. Adults, especially those residing in rural areas should be targeted to increase health literacy and raise awareness about LVH, its complications and adjust their modifiable risk factors especially controlling blood pressure. Authorities in rural communities such as healthcare workers at health promoting hospitals should provide HT and DM screening to identify potential risk factors for LVH. Then adults with HT or DM should be invited to receive a continuous care under the universal health coverage scheme for blood pressure, glycemic control and LVH early detection. Our study may not be generalized to the whole country but may reflect the real experience of adults residing in rural communities in Thailand.
Conclusion
Our data emphasized that ECG-LVH was a significant health issue among adults residing in a rural community in Thailand. Effective public health interventions, especially controlling blood pressure and raising awareness of HT status, should be provided in the community to reduce risks of ECG-LVH. The modifiable risk factors for ECG-LVH should be attenuated to inhibit the progression of cardiovascular events including coronary heart disease and cardiac mortality.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available because the data set contains sensitive identifying information. Because ethical restrictions have been placed, the data sets are available from the corresponding author on reasonable request.
Abbreviations
- ECG-LVH:
-
Electrocardiographic-left ventricular hypertrophy
- LV:
-
Left ventricular
- HT:
-
Hypertension
- DM:
-
Diabetes mellitus
- HR:
-
Heart rate
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- OR:
-
Odds ratio
- AOR:
-
Adjusted odds ratio
- 95% CI:
-
95% Confidence interval
References
Lazzeroni, D., Rimoldi, O. & Camici, P. G. From left ventricular hypertrophy to dysfunction and failure. Circ. J. 80, 555–564 (2016).
Verdecchia, P. et al. Sudden cardiac death in hypertensive patients. Hypertension (Dallas) 73, 1071–1078 (2019).
Kannel, W. B. Left ventricular hypertrophy as a risk factor: The Framingham experience. J. Hypertens. Suppl. Off. J. Int. Soc. Hypertens. 9, S3–S8 (1991).
Levelt, E. et al. Relationship between left ventricular structural and metabolic remodeling in type 2 diabetes. Diabetes 65, 44–52 (2016).
Chizindu, A. A. & Emem-Chioma, P. The prevalence and correlations of electrocardiographic-left ventricular hypertrophy in a rural community in Africa. Niger. J. Med. 27, 7–13 (2018).
Jaggy, C. et al. Performance of classic electrocardiographic criteria for left ventricular hypertrophy in an African population. Hypertension 36, 54–61 (2000).
Tangjatuporn, W. et al. Associated factors of blood pressure control and complications of hypertension in hypertensive rural Thai populations of Baan Nayao, Chachoengsao Province. J. Med. Assoc. Thail. 95(Suppl 5), S48-57 (2012).
Brown, D. W., Giles, W. H. & Croft, J. B. Left ventricular hypertrophy as a predictor of coronary heart disease mortality and the effect of hypertension. Am. Heart J. 140, 848–856 (2000).
Nkum, B. C., Micah, F. B., Ankrah, T. C. & Nyan, O. Left ventricular hypertrophy and insulin resistance in adults from an urban community in The Gambia: Cross-sectional study. PLoS ONE 9, e93606 (2014).
Okin, P. M., Jern, S., Devereux, R. B., Kjeldsen, S. E. & Dahlöf, B. Effect of obesity on electrocardiographic left ventricular hypertrophy in hypertensive patients: The losartan intervention for endpoint (LIFE) reduction in hypertension study. Hypertension (Dallas) 35, 13–18 (2000).
Vakili, B. A., Okin, P. M. & Devereux, R. B. Prognostic implications of left ventricular hypertrophy. Am. Heart J. 141, 334–341 (2001).
Devereux, R. B. et al. Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA 292, 2350–2356 (2004).
Sriratanasathavorn, C. et al. The prevalence of left ventricular hypertrophy and associated factors in a Thai population. J. Med. Assoc. Thailand 83, S218–S222 (2000).
Rautaharju, P. M. et al. Electrocardiographic estimate of left ventricular mass versus radiographic cardiac size and the risk of cardiovascular disease mortality in the epidemiologic follow-up study of the First National Health and Nutrition Examination Survey. Am. J. Cardiol. 62, 59–66 (1988).
Centers for Disease Control and Prevention. Adult Tobacco Use Information (2020). https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm. Accessed 24 May 2020
Inoue, S. et al. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment (Health Communications Australiat, 2000).
Oh, S., Ahn, J., Nam, K.-U., Paeng, J.-Y. & Hong, J. Frankfort horizontal plane is an appropriate three-dimensional reference in the evaluation of clinical and skeletal cant. J. Korean Assoc. Oral Maxillofac. Surg. 39, 71–76 (2013).
WHO. Measuring Obesity: Classification and Description of Anthropometric Data: Report on a WHO Consultation on the Epidemiology of Obesity 2–7 (WHO, 1987).
Meelab, S. et al. Prevalence and associated factors of uncontrolled blood pressure among hypertensive patients in the rural communities in the central areas in Thailand: A cross-sectional study. PLoS ONE 14, e0212572 (2019).
Thai Hypertension Society. 2019 Thai Guidelines on the Treatment of Hypertension (Thai Hypertension Society, 2019).
Jevon, P. Procedure for recording a standard 12-lead electrocardiogram. Br. J. Nurs. 19, 649–651 (2010).
Sokolow, M. & Lyon, T. P. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am. Heart J. 37, 161–186 (1949).
Okin, P. M., Roman, M. J., Devereux, R. B. & Kligfield, P. Electrocardiographic identification of increased left ventricular mass by simple voltage-duration products. J. Am. Coll. Cardiol. 25, 417–423 (1995).
Devereux, R. B., Casale, P. N., Eisenberg, R. R., Miller, D. H. & Kligfield, P. Electrocardiographic detection of left ventricular hypertrophy using echocardiographic determination of left ventricular mass as the reference standard. Comparison of standard criteria, computer diagnosis and physician interpretation. J. Am. Coll. Cardiol. 3, 82–87 (1984).
Eguchi, K. et al. Association between diabetes mellitus and left ventricular hypertrophy in a multiethnic population. Am. J. Cardiol. 101, 1787–1791 (2008).
Jobe, M. et al. Electrocardiographic left ventricular hypertrophy among gambian diabetes mellitus patients. Ghana Med. J. 49, 19–24 (2015).
Liao, Y., Cooper, R. S., Mensah, G. A. & McGee, D. L. Left ventricular hypertrophy has a greater impact on survival in women than in men. Circulation 92, 805–810 (1995).
Gosse, P. Left ventricular hypertrophy as a predictor of cardiovascular risk. J. Hypertens. Suppl. Off. J. Int. Soc. Hypertens. 23, S27-33 (2005).
Okwuosa, T. M. et al. Left ventricular hypertrophy and cardiovascular disease risk prediction and reclassification in blacks and whites: The atherosclerosis risk in communities study. Am. Heart J. 169, 155–161 (2015).
Porthan, K. et al. ECG left ventricular hypertrophy as a risk predictor of sudden cardiac death. Int. J. Cardiol. 276, 125–129 (2019).
Dweck, M. R. et al. Left ventricular remodeling and hypertrophy in patients with aortic stenosis: Insights from cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 14, 50 (2012).
Glenn, D. J. et al. A murine model of isolated cardiac steatosis leads to cardiomyopathy. Hypertension 57, 216–222 (2011).
Mbaye, A. et al. Left ventricular hypertrophy in black African subjects with artery hypertension: Results of a cross-sectional survey conducted in semi-rural area in Senegal. Ann. Cardiol. Angeiol. (Paris) 66, 210–216 (2017).
Shenasa, M. & Shenasa, H. Hypertension, left ventricular hypertrophy, and sudden cardiac death. Int. J. Cardiol. 237, 60–63 (2017).
Mewton, N., Liu, C. Y., Croisille, P., Bluemke, D. & Lima, J. A. C. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 57, 891–903 (2011).
Palatini, P. & Julius, S. Elevated heart rate: A major risk factor for cardiovascular disease. Clin. Exp. Hypertens. 26, 637–644 (2004).
Inoue, T. & Ohya, Y. Elevated heart rate, a risk factor and risk marker of cardiovascular disease. Curr. Hypertens. Rev. 7, 29–40 (2011).
Saba, M. M., Ibrahim, M. M. & Rizk, H. H. Gender and the relationship between resting heart rate and left ventricular geometry. J. Hypertens. 19, 367–373 (2001).
Zakopoulos, N. A. et al. Twenty-four-hour heart rate and blood pressure are additive markers of left ventricular mass in hypertensive subjects. Am. J. Hypertens. 19, 170–177 (2006).
Inoue, T. et al. Development of electrocardiographic left ventricular hypertrophy and resting heart rate over time: Findings from the OGHMA study. Angiology 71, 70–76 (2019).
Acknowledgements
The authors express their grateful thanks to the director, healthcare workers and village health volunteers of Baan-Na-Yao Health Promoting Hospital, Chachoengsao Province. The authors thank all the staff of the Department of Military and Community Medicine, Phramongkutklao College of Medicine, for their support in completing this study.
Funding
The present study was supported by Phramongkutklao College of Medicine.
Author information
Authors and Affiliations
Contributions
The concept for study was developed by P.V., S.L., P.L., T.P., P.P., S.P., P.A., V.P., K.C., P.J., P.K., N.P., R.P., P.T., M.M., R.R. and B.S. P.V., S.L., P.L., T.P., P.P., S.P., P.A., V.P., K.C., P.J., P.K., N.P., R.P. and B.S. collected the data. P.V., S.L., P.L. and B.S. analyzed the data. P.V., S.L., P.L. and B.S. wrote the first draft. All authors contributed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Viwatrangkul, P., Lawanwisut, S., Leekhaphan, P. et al. Prevalence and associated factors of electrocardiographic left ventricular hypertrophy in a rural community, central Thailand. Sci Rep 11, 7083 (2021). https://doi.org/10.1038/s41598-021-86693-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-86693-2
This article is cited by
-
Factors associated with electrocardiographic left ventricular hypertrophy among patients with hypertension in Thailand
Clinical Hypertension (2024)
-
Association between raised blood pressure and elevated serum liver enzymes among active-duty Royal Thai Army personnel in Thailand
BMC Cardiovascular Disorders (2023)
-
Effect of the weight-loss program using daily self-weighing combined with personalized counseling led by village health volunteers in adults with obesity in a rural community, Thailand: a randomized controlled trial
BMC Primary Care (2023)
-
Prevalence, awareness, and control of hypertension and associated factors among Royal Thai Army personnel in Thailand from 2017 to 2021
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.