Abstract
Favipiravir is considered a potential treatment for COVID-19 due its efficacy against different viral infections. We aimed to explore the safety and efficacy of favipiravir in treatment of COVID-19 mild and moderate cases. It was randomized-controlled open-label interventional phase 3 clinical trial [NCT04349241]. 100 patients were recruited from 18th April till 18th May. 50 patients received favipiravir 3200 mg at day 1 followed by 600 mg twice (day 2–day 10). 50 patients received hydroxychloroquine 800 mg at day 1 followed by 200 mg twice (day 2–10) and oral oseltamivir 75 mg/12 h/day for 10 days. Patients were enrolled from Ain Shams University Hospital and Assiut University Hospital. Both arms were comparable as regards demographic characteristics and comorbidities. The average onset of SARS-CoV-2 PCR negativity was 8.1 and 8.3 days in HCQ-arm and favipiravir-arm respectively. 55.1% of those on HCQ-arm turned PCR negative at/or before 7th day from diagnosis compared to 48% in favipiravir-arm (p = 0.7). 4 patients in FVP arm developed transient transaminitis on the other hand heartburn and nausea were reported in about 20 patients in HCQ-arm. Only one patient in HCQ-arm died after developing acute myocarditis resulted in acute heart failure. Favipiravir is a safe effective alternative for hydroxychloroquine in mild or moderate COVID-19 infected patients.
Similar content being viewed by others
Introduction
At the end of 2019, the entire world saw the first appearance of the coronavirus disease 2019 (COVID-19)1. By March 2020, it was declared a pandemic by the World Health Organization (WHO). Globally, more than 83 million cases of COVID-19 and more than 1.5 million deaths have been reported so far2, 3. The first case registered in Egypt was in February 2020, and, since then, the number has been increasing. By early July 2020, nearly 1.5 hundred thousand confirmed cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and about 8000 deaths were reported by the Ministry of Health (MoH)4. In Egypt, the curve of new cases prompted an investigation into the different treatment options to find the most effective and safe choice for COVID-19 patients. Favipiravir (FPV) is one of the potential options according to a Chinese study, considering its past history of efficacy against viral influenza5.
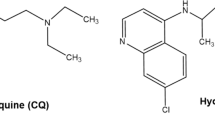
Being a novel RNA-dependent RNA polymerase (RdRp) inhibitor, FPV has also shown efficacy against the Ebola virus6, 7. FVP, known as Avigan, is a pyrazine derivative and guanine analogue that acts as a chain termination tool and prevents RNA elongation. Favipiravir demonstrated anti-viral activities against a broad array of RNA viruses, including arenaviruses, bunyaviruses, and filoviruses8. In Japan, favipiravir has been approved for influenza A resistant to neuraminidase inhibitors9.
Also, an expert consensus group in China suggested that chloroquine improved lung imaging and shortened the disease course10. However, a number of additional reports have since shown no positive impact with the addition of hydroxychloroquine (HCQ)11. The aim of the current study was to explore the safety and efficacy of favipiravir in the treatment of mild and moderate COVID-19 cases compared to hydroxychloroquine plus oseltamivir as the standard of care approved by the national protocol there.
Patients and methods
Study objectives
The primary objective of the current study was to evaluate the SARS-CoV-2 viral clearance on Days 3, 7 and 14. While the secondary objectives were the evaluation of the clinical outcomes on Days 3, 7, and 14, and the safety assessment of favipiravir versus the standard of care (SOC) HCQ-based therapy in the treatment of patients with mild or moderate COVID-19.
End points
The primary endpoints were the achievement of two successive negative SARS-CoV-2 PCR analysis tests 48 h apart by nasopharyngeal swab, normalization of body temperature for 48 h, improvement of radiological abnormalities at Day 14 and the hospital discharge rate. The secondary endpoints were the normalization of C-reactive protein (CRP) and serum ferritin levels.
Study design
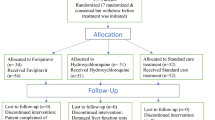
It was a computer-based randomized, controlled, and interventional clinical Phase 3 trial to assess the safety and efficacy of favipiravir versus a HCQ-based therapy (SOC) in the treatment of 100 patients with mild or moderate COVID-19, confirmed by reverse transcription polymerase chain reaction (RT-PCR) of nasopharyngeal swabs. A block-randomization scheme was generated by computer software; patients were randomized between favipiravir and the HCQ-based therapy in a 1:1 ratio. All patients were enrolled from day zero of presentation to the isolation hospital. Group I included 50 patients, who received oseltamivir 75 mg 12 hourly for 10 days and hydroxychloroquine 400 mg 12 hourly on Day 1, followed by 200 mg 12 hourly daily on Day 2 to 10, conforming to the national standard of care therapy. Group 2 included 50 patients, who received the investigational drug favipiravir in a regimen of 3200 mg (1600 mg 12 hourly) loading dose on Day 1 followed by 1200 mg maintenance dose (600 mg 12 hourly daily) on Days 2 to 10.
The procedures applied in this study were approved by the Ethical Committee of Human Experimentation of Ain Shams University [FMASU P14/2020] and registered on clinicaltrials.gov [NCT04349241] on 16 April 2020 and was in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments in humans, 2013. Recruitment started on 18 April 2020.
Study setting
Patients with COVID-19 were randomized to either therapy protocols in two university isolation hospitals. Among 243 COVID-19 patients presented to the two participating isolation hospitals, 100 met the inclusion criteria and agreed to participate in the trial. In the first hospital, Obour Ain Shams University Specialized Hospital (situated in Cairo), 40 patients received favipiravir and 46 the HCQ-based therapy. The rest were admitted to the second hospital, Assiut University Hospital (situated in Upper Egypt).
Study population
The included patients were adults between 18 and 80 years with confirmed COVID-19 documented by diagnostic laboratory tests (e.g. nasopharyngeal swab) at the time of illness and having mild to moderate symptoms according to the national protocol classification. Patients in whom the disease was severe, as indicated by the presence of dyspnea, respiratory rate ≥ 30/min, blood oxygen saturation ≤ 93%, partial pressure of arterial oxygen to fraction of inspired oxygen ratio < 300, and/or lung infiltrates > 50% within 24–48 h or a life-threatening symptoms of the disease defined as respiratory failure, septic shock, and/or multiple organ dysfunction or failure, were excluded. Moreover, pregnant or lactating females or those who participated in any investigational clinical study, other than observational, within the previous 30 days were also excluded.
Study procedures
Screening phase
A written, signed, and dated informed consent form (ICF) was obtained from each patient (if the subject was unable to provide informed consent, the subject’s legally acceptable representative signed instead of them) before inclusion in the study. Patients’ clinical report forms included demographic data, full medical history, comorbidities and concurrent medications. In addition, in a physical examination, the body weight, height, body mass index, vital signs (blood pressure, heart rate and temperature) and blood oxygen saturation were assessed and recorded.
Baseline laboratory investigations included complete blood count (CBC), liver (alanine amino transferase (ALT), aspartate amino transferase (AST), total and direct bilirubin, kidney function tests (serum creatinine), CRP, serum ferritin, HIV antibody, HCV antibody, HBV surface antigen (HBsAg) and urine pregnancy test for females. Creatine kinase (CK) total and creatine kinase-MB (CK-MB), lactate dehydrogenase (LDH) and coagulation test (D-dimer, prothrombin time and INR) were assessed. COVID-19 was confirmed by SARS-CoV-2 RT-PCR test based on the nasopharyngeal swab. On admission, besides electrocardiogram (ECG), and chest X-ray or computed tomography (CT) scan of the chest was also performed.
Treatment phase
Once eligibility was confirmed, patients were randomized and medication started. The patients received information regarding the identification and notification of adverse events, and the recording of the concomitant medications. The patients were advised to record in diaries the daily doses of the study medications. If the patients were fatigued or uneducated, the clinical pharmacist or the treating physician was responsible for recording the data. Clinical assessment and vital signs were documented daily and adverse events were recorded. Follow-up laboratory results for liver function tests, SARS-CoV2 RT-PCR tests by nasopharyngeal swab, CRP, and serum ferritin levels were repeated on Days 3, 7, and 14 of the treatment. Follow-up chest X-ray and/or CT scan were performed on Day 14. All patients received anticoagulation in both arms in the form of enoxaparin 40 mg SC for 14 days or 1 mg/kg every 12 h in case of D-dimers > 1000 ng/ml for 1 month.
Follow-up phase
Patients were followed up for a period of up to 30 days following the end of treatment for any newly developed symptoms, signs or adverse events.
Theory
The aim of the current study was to explore the safety and efficacy of favipiravir in the treatment of mild and moderate cases of COVID-19 compared to hydroxychloroquine plus oseltamivir as the standard of care approved the national protocol.
Statistical methods
Descriptive statistics were displayed in term of mean and standard deviation in continuous variables and frequency distribution (number and percentage) in case of categorical variables. Student t test was used to compare the means of the two groups and Chi-square was used to test the association between categorical variables. Fisher Exact was used if the expected number in one cell of the 2 × 2 table was less than 5 or less than 5 observations were expected in more than 25% of the cells. A p value of ≤ 0.05 was considered statistically significant. SPSS (Statistical Package for Social Sciences or Statistical Product and Service Solutions) version 22.0 was used. Absolute risk (benefit) was calculated as the number of patients showing PCR conversion as a percentage of all PCR +ve cohort at a certain time point.
Results
One hundred confirmed COVID-19 patients, according to the standard case definition, were randomly divided between the FPV and HCQ-based therapy arms.
Table 1 illustrates the base line characteristics of the two study groups with COVID-19. Both FPV and HCQ-based therapy groups were comparable as regards demographic characteristics and comorbidities. Healthcare workers represented 70% in the FPV and 62% in the HCQ-based therapy arms. Direct contact with a confirmed case was reported by 74% and 72% of patients treated in the FPV arm and HCQ-based therapies respectively. Comorbidities in the form of hypertension, diabetes, and ischemic heart diseases were equally manifested in both groups. Patients treated in the HCQ-based arm reported 1 extra day of hospital stay on average, but the difference was not statistically significant (12.4 vs. 11.5 days in the HCQ based arm and FPV arm respectively).
As for the laboratory safety profile; three patients (6%) in the HCQ-based arm reported a D-dimer level above 1000 compared to seven patients in the FPV (14%), but the difference was not significant. The average platelet count was relatively lower in the HCQ-based group compared to the FPV arm and the difference was significant (p = 0.029). Radiologically, 24% of those who received the HCQ-based therapy showed bilateral basal peripheral ground glass opacities in chest CT compared to 20% of those who received FPV (p > 0.05). Serum ferritin, LDH, CK total and CKMB showed no significant difference between the two groups.
The main symptoms and signs reported in the two groups were fever and dry cough, as illustrated in Table 2. They were reported more frequently in the FPV arm (36% vs. 38% respectively) than the HCQ-based therapy (24% and 30% respectively), but the difference was not significant (p > 0.05). Expectoration, sore throat, diarrhoea, rhinorrhea, anosmia and loss of taste were rarely reported by patients from either group. Oxygen saturation was within an average of 97% on room air in both groups.
The average onset of SARS-CoV-2 PCR negativity was 8.1 days in the HCQ-based therapy and 8.3 days in the FPV arm. More than half of the patients on the HCQ-based therapy (55.1%) turned PCR negative at or before the 7th day from diagnosis compared to 48% in the FPV arm. However, the difference was not statistically significant (p = 0.7). Figure 1 shows the percentage of the onset of SARS-CoV2 PCR negativity starting from the 3rd till the 14th day.
The efficacy of the two treatment regimens were assessed with respect to improvement in the laboratory tests; D-dimer and serum ferritin as well as the radiological improvements are illustrated in Table 3. The two regimens were comparable in relation to the viral clearance before the 7th day in terms of the 3 parameters: D-dimer, serum ferritin, and radiological findings. COVID-19 patients with D-dimer ≤ 250 ng/ml, 68.2% (n = 15) cleared the virus before the 7th day in the HCQ-based therapy compared to only 45.5% (n = 5) in the FPV arm (p = 0.379).
Both regimens displayed a different safety profile. Four patients (8%) in the FPV arm experienced elevated liver transaminases 3–5 times the upper normal limit between Day 7 and Day 14, but did not necessitate the withholding of therapy and improvement was seen within 2 weeks after the end of treatment. There was one case of mortality among the COVID-19 patients in the HCQ-based arm due to an acute heart failure resulting from myocarditis on Day 8.
Discussion
Despite the emergence of the COVID 19 vaccines, the need for reliable, safe, and efficient treatment options is still the most important point of clinical research. At the start of the pandemic, hydroxychloroquine was suggested as a potential antiviral medication based on the medication’s cellular interaction with the virus and in vitro data12, 13. The clinical debate is confronting any newly published articles regarding any promising Drugs. Different studies argued about the efficacy of favipiravir and hydroxychloroquine. Initial anecdotal evidence suggested that HCQ helps with pneumonia with regard to the shortening of the disease course and an improvement of lung imaging14. This led the Centers for Disease Control and Prevention (CDC) to suggest the use of HCQ and the Food and Drug Administration (FDA) allowing its emergency use without rigorous clinical trials followed by the revocation of its emergency use in mid-June 202015, 16. These results directed researchers all over the world to test different treatment options to decrease the median duration of viremia to get better outcomes.
Favipiravir inhibits SARS-CoV-2 in vitro17. According to the limited published data regarding its use in COVID-19 management, there was a great need for different studies evaluating its efficacy and safety in such a situation. A randomized study, Favipiravir versus Arbidol, showed a better outcome with favipiravir in patients with moderate severity18. Another multicentre prospective Chinese trial, randomized open-label, studying 236 patients, compared favipiravir and Arbidol, demonstrated a higher clinical recovery rate at Day 7 in moderately ill patients receiving favipiravir (71.4% vs. 55.9%, p = 0.0199). Clinical recovery was defined as 3 or more days of improvement in the respiratory rate, oxygenation, cough, and fever. There was no placebo group for comparison and this study has not been peer reviewed18. Favipiravir, when compared to other anti-viral drugs like lopinavir/ritonavir, demonstrated reduced median viral clearance and radiographic chest imaging improvement with an average of 4 days, which is shorter than that of the current study (8.3 days) in the FVP arm5. This may be due to a larger number of their recruited patients. The clinical improvement such as mainly fever resolution was achieved chiefly at Day 3, and dry cough at Day 7 in the FPV group in the current study, besides the improvement of the other symptoms. Our data compared age, sex-matched groups, randomized to SOC (HCQ and Oseltamivir) and FPV showed similar efficacy regarding time to viral clearance by nasopharyngeal swab PCR testing (p = 0.7), mean hospital stay (p = 0.4) and safety.
The current study is considered as one of the first randomized controlled trials, assessing HCQ and Oseltamivir (the national standard protocol) versus FPV for treatment of mild to moderate COVID-19 disease. Nearly 90% of both groups of patients achieved viral clearance by Day 14 and there was one case of mortality in the HCQ-based group. Tang and colleagues found that the probability of negative SARS-CoV-2 testing by Day 28 was 85.4% in the HCQ group and 81.3% in the SOC group (difference 4.1%, 95% CI 10.3–18.5%) and adverse effects were more common in the HCQ group (30% vs. 9%), which was superior to that reported in the current study HCQ-arm based therapy of about 40% gastrointestinal tracts symptoms10.
Despite that, favipiravir resulted in a moderate elevation of hepatic transaminases (8%), which is higher than what has been reported by Cai and his colleagues, in only one patient (2.86%). It dropped back to normal levels within 2 weeks and there was no discontinuation of treatment. Achieving a high safety profile in a large number of patients apart from gastrointestinal upsets and a transient elevation of transaminases made out the FVP to be a safe and promising agent19. Being the backbone of a treatment protocol is minimizing the risk of adverse events and drug-drug interactions, the HCQ-receiving group of patients reported in 20 patients various gastrointestinal symptoms including epigastric pain, nausea, and diarrhoea, requiring symptomatic treatment in half of them.
Despite the comparable efficacy of both arms of treatment in the current study, we should consider the international debate regarding the HCQ safety. This has led to much controversy, given the potential for cardiac complications, prompting medical experts to advocate caution20. There is currently a race for finding an effective treatment for COVID-19 and there are a lot of uncertainties concerning the benefit of treatment with HCQ21. Two small non-peer reviewed randomized studies have shown seemingly contradictory results. In one study, HCQ did not exhibit any difference in fever improvement or viral clearance with negative SARS-CoV-2 PCR22. In another study, HCQ showed a significant improvement in symptoms and radiological CT scan findings23. One recent non-randomized study failed to demonstrate any benefit among patients hospitalized with an oxygen requirement24, while an open-labelled randomized controlled trail (RCT) involving 150 patients demonstrated a modest alleviation of symptoms25.
A retrospective analysis of data from patients hospitalized with confirmed SARS-CoV-2 infection in all U.S. Veterans Health Administration medical centres until April 11, 2020, concluded that there was no clear evidence that the use of HCQ, either with or without azithromycin, reduced the risk of mechanical ventilation in patients hospitalized with COVID-1926. An association of increased overall mortality was identified in patients treated with HCQ alone27.
Geleris and colleagues retrospectively found that there was no significant association between HCQ use and the need for invasive ventilation or death. These findings were reached after a review of 1376 COVID-19 patients hospitalized in New York City. More than 800 patients among them received HCQ (dosed at 600 mg on Day 1, followed by 400 mg daily for 5 days)28. The low mortality rate in our study could be explained by the early initiation of the antiviral treatment as found in other studies. Also, the target group of patients were mainly mild to moderate cases only, with the exclusion of severely and critically ill patients29. The use of oseltamivir was part of the national protocol of treatment of such cases at the beginning of the pandemic. It was removed lately from the current protocols. Both drugs are being studied in new clinical trials even in combination30.
In conclusion it can be said that favipiravir is a safe and effective alternative to hydroxychloroquine in patients with mild or moderate COVID-19. Favipiravir can be used safely during home isolation for mild to moderate cases. But the safety of hydroxychloroquine for home treatment in isolation is still questionable. Further studies on the role of favipiravir in severe COVID 19 patient management are recommended.
Limitations of the study
The low number of included patients due to the limited availability of favipiravir.
Change history
18 September 2021
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1038/s41598-021-98683-5
References
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497e506 (2020).
World Health Organization. .https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed on 3/1/2021.
Chan, J. F. et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395, 514e23 (2020).
Egyptian Ministry of Health. https://www.care.gov.eg/EgyptCare/Index.aspx. Accessed 3/1/2021.
Cai, Q. et al. Experimental treatment with favipiravir for COVID-19: An open-label control study. Engineering 6, 1192–1198 (2020).
Madelain, V. et al. Ebola virus dynamics in mice treated with favipiravir. Antiviral Res. 123, 70–77 (2015).
Furuta, Y., Komeno, T. & Nakamura, T. Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 93(7), 449–463 (2017).
Hayden, F. G. & Shindo, N. Influenza virus polymerase inhibitors in clinical development. Curr. Opin. Infect. Dis. 32(2), 176–186 (2019).
Zhonghua, J., He, H., Hu, X. & Za, Z. Expert consensus on chloroquine phosphate for the treatment of novel coronavirus pneumonia. 43, E019 (2020).
Tang, W. et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: Open label, randomised controlled trial. BMJ 14(369), m1849 (2020).
Zhou, D., Dai, S. M. & Tong, Q. COVID-19: A recommendation to examine the effect of hydroxychloroquine in preventing infection and progression. J. Antimicrob. Chemother., dkaa114.
Liu, J. et al. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 6, Article 16 (2020).
Gao, J., Tian, Z. & Yang, X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci. Trends 14(1), 72–73 (2020).
Information for Clinicians on Investigational Therapeutics for Patients with COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/therapeutic-options.html.
Food and Drug Administration. www.fda.gov/media/138945/download.
American College of Cardiology. Ventricular arrhythmia risk due to hydroxychloroquine-azithromycin treatment for COVID-19. https://www.acc.org/latest-in-cardiology/articles/2020/03/27/14/00/.
Wang, M. et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 30(3), 269–271 (2020).
Chen, C., Zhang, Y., Huang, J. & Yin, P. Favipiravir versus arbidol for COVID-19: A randomized clinical trial. medRxiv https://doi.org/10.1101/2020.03.17.20037432v4 (2020).
Pilkington, V., Pepperrell, T. & Hill, A. A review of the safety of favipiravir—A potential treatment in the COVID-19 pandemic?. J. Virus Erad. 6, 45–51 (2020).
de Barros, C. M. et al. COVID-19 pandemic—A narrative review of the potential roles of chloroquine and hydroxychloroquine. Pain Physician 23(4S), S351–S366 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study [published correction appears in Lancet. 2020 Mar 28;395(10229):1038]. Lancet 395(10229), 1054–1062 (2020).
Jun, C. et al. A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease-19 (COVID-19). J. Zhejiang Univ. 49, 215–219 (2020).
Chen, Z. et al. Efficacy of hydroxychloroquine in patients with COVID-19: Results of a randomized clinical trial. medRxiv https://doi.org/10.1101/2020.03.22.20040758v3 (2020).
Mahevas, M. et al. No evidence of clinical efficacy of hydroxychloroquine in patients hospitalized for COVID-19 infection with oxygen requirement: Results of a study using routinely collected data to emulate a target trial. BMJ 369, m1844 (2020).
Tang, W. et al. Hydroxychloroquine in patients mainly with mild to moderate COVID-19: An open-label, randomized, controlled trial. medRxiv https://doi.org/10.1101/2020.04.10.20060558v2 (2020).
Magagnoli, J. et al. Outcomes of hydroxychloroquine usage in United States veterans hospitalized with COVID-19. medRxiv https://doi.org/10.1101/2020.04.16.20065920v1.full.pdf (2020).
Borba, M. et al. Chloroquine diphosphate in two different dosages as adjunctive therapy of hospitalized patients with severe respiratory syndrome in the context of coronavirus (SARS-CoV-2) infection: Preliminary safety results of a randomized, double-blinded, phase IIb clinical trial (CloroCovid-19 Study). JAMA Netw. Open 3(4), e208857. https://doi.org/10.1001/jamanetworkopen.2020.8857 (2020).
Geleris, J., Sun, Y., Platt, J. & Zucker, J. Observational study of hydroxychloroquine in hospitalized patients with COVID-19. N. Engl. J. Med. 382, 2411–2418 (2020).
Saber-Ayad, M., Saleh, M. A. & Abu-Gharbieh, E. The rationale for potential pharmacotherapy of COVID-19. Pharmaceuticals 13(5), 96 (2020).
Bosaeed, M. et al. A trial of favipiravir and hydroxychloroquine combination in adults hospitalized with moderate and severe Covid-19: A structured summary of a study protocol for a randomised controlled trial. Trials 21(1), 904. https://doi.org/10.1186/s13063-020-04825-x.PMID:33129363;PMCID:PMC7602769 (2020).
Funding
This study was funded by Rameda Pharmaceutical Company.
Author information
Authors and Affiliations
Contributions
H.D. shared in the protocol of the study, data collection and writing the manuscript. A.F.S. data collection and writing the manuscript. All other authors contributed equally in Management and follow up of patients beside data collection. By M.E. statistical analysis was done. Study design and revision of the manuscript by M.E.-S. and F.E. were done.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1038/s41598-021-98683-5
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dabbous, H.M., El-Sayed, M.H., El Assal, G. et al. RETRACTED ARTICLE: Safety and efficacy of favipiravir versus hydroxychloroquine in management of COVID-19: A randomised controlled trial. Sci Rep 11, 7282 (2021). https://doi.org/10.1038/s41598-021-85227-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-85227-0
This article is cited by
-
Biased, wrong and counterfeited evidences published during the COVID-19 pandemic, a systematic review of retracted COVID-19 papers
Quality & Quantity (2023)
-
Addendum: The efficacy and safety of Favipiravir in treatment of COVID-19: a systematic review and meta-analysis of clinical trials
Scientific Reports (2022)
-
Small molecules in the treatment of COVID-19
Signal Transduction and Targeted Therapy (2022)
-
Efficacy of antiviral therapies for COVID-19: a systematic review of randomized controlled trials
BMC Infectious Diseases (2022)
-
Effectiveness of favipiravir in COVID-19: a live systematic review
European Journal of Clinical Microbiology & Infectious Diseases (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.