Abstract
Appropriate drainage duration is vital for the postoperative rehabilitation of patients with breast cancer (BC) undergoing modified radical mastectomy (MRM). To provide better and individualized postoperative management for these patients, this study explored independent predictors of postoperative drainage duration in patients with BC. This was a single-center retrospective cohort study. Patients diagnosed with BC and treated with MRM from May 2016 to April 2020 were randomly divided into training (n = 729) and validation (n = 243) cohorts. Univariate and multivariate Cox analyses revealed that the body mass index, serum albumin level, hypertension, number of total dissected axillary lymph nodes, and ratio of positive axillary lymph nodes were independent predictors of postoperative drainage duration in the training cohort. Based on independent predictors, a nomogram was constructed to predict the median postoperative drainage duration and the probability of retaining the suction drain during this period. This nomogram had good concordance and discrimination both in the training and validation cohorts and could effectively predict the probability of retaining the suction drain during drainage, thus assisting clinicians in predicting postoperative drainage duration and providing individualized postoperative management for patients with BC.
Similar content being viewed by others
Introduction
Breast cancer (BC) is a critical public health threat to women worldwide1. At present, the treatment of BC mainly includes surgical operation, radiotherapy, chemotherapy, endocrine therapy, and targeted therapy2. Modified radical mastectomy (MRM) is a widely used surgical method for invasive BC; it is also the gold standard for the staging of axillary lymph nodes in patients with axillary lymph node metastasis3. Patients undergoing MRM usually have varied postoperative drainage durations due to the large surgical wound and the injury to blood vessels and lymphatic vessels during the surgery4. No consensus exists on the timing of suction drain removal. However, the premature removal of the suction drain may lead to seroma formation, thus increasing the risk of infection, arm lymphedema, and flap necrosis. In addition, later extubation limits postoperative shoulder exercise and prolongs the hospital stay of patients5.
Hypertension and obesity were recognized as factors that prolong drainage duration in patients undergoing mastectomy and axillary dissection6,7,8,9,10. A few other predictors have also been reported, but no model was available for predicting postoperative drainage duration. Therefore, exploring more predictors and constructing a predictive model of drainage duration was necessary so as to provide better and individualized postoperative management for patients. Nomogram is a convenient and intuitive modeling tool that can quantify demographic and clinical variables to generate a visible model that can predict a specific event11.
The purpose of this study was to explore factors related to drainage duration in patients undergoing MRM. Based on this, an efficient model was explored, and a nomogram was constructed that could be used for an individualized assessment of drainage duration in patients with BC.
Materials and methods
Patients selection and data acquisition
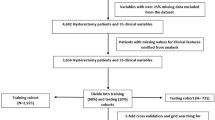
This study involved female patients with unilateral BC who underwent MRM at Northern Jiangsu People’s Hospital between May 2016 and April 2020. During the surgery, an ultrasonic scalpel was used to dissect axillary lymph nodes, and larger lymphatic vessels were ligated using absorbable sutures. After mastectomy and axillary dissection, two suction drains were placed to provide negative pressure suction: one at the axilla and the other at the chest wall. Besides, elastic bandage and external compression dressing were used to obliterate the dead space of the chest wall and axilla after the surgery. The exclusion criteria were as follows: (1) the number of total dissected axillary lymph nodes less than 10, (2) received neoadjuvant therapy before the surgery, (3) distant metastases occurred when patients were diagnosed, (4) drainage duration of axillary suction drain more than 3 weeks, (5) patients with seroma formation after removing axillary suction drain, (6) patients with an incomplete record of drainage duration, (7) patients with a disease that may change hematological data, and (8) patients with other complications. Finally, 972 patients were included in the study.
The following data were collected for each patient: patient ID, age, laterality of tumor, body mass index (BMI), peripheral blood lymphocyte count (PBLC), serum albumin level, hypertension, diabetes, type of intraoperative fluid, use of painkillers after surgery, number of positive axillary lymph nodes (PLNs), number of total dissected axillary lymph nodes (TLNs), drainage duration of chest wall suction drain (DDCSD), and drainage duration of axillary suction drain (DDASD). The drainage fluid was emptied and measured every 24 h. The criterion of chest wall and axillary suction drain removal was total drain output of 20 mL or less daily for 2 days starting from postoperative day 3. The chest wall suction drain was removed before the axillary suction drain.
The need for informed consent was waived by approving ethics committee because of the retrospective nature of the study, and the study design was approved by the Medical Ethics Committee of Northern Jiangsu People's Hospital.
Independent predictors of DDASD
The eligible patients were randomly divided into training cohort and validation cohort. The training cohort was used to explore independent predictors of DDASD and construct a predictive nomogram model. First, univariate Cox models were employed to identify the relationships between clinicopathological characteristics and DDASD of patients. Variables significantly correlated with the DDASD were screened out by the P value < 0.05 in the univariate Cox model. Second, these significant variables were further fitted into a multivariate Cox model. The variance inflation factor (VIF) value of each variable was checked to confirm the collinearity among variables. Finally, variables with the P value < 0.05 in the multivariate Cox model were considered as independent predictors and used to construct the nomogram model.
Construction and validation of the nomogram
A predictive nomogram model was constructed based on the results of the multivariate Cox model. This nomogram was validated using the validation cohort and internally processed. The concordance index (C-index) with a 95% confidence interval (95% CI) was calculated in the training and validation cohorts to evaluate the discrimination of the nomogram. Calibration plots (500 bootstrap resamples) were established to check the concordance between the nomogram‐predicted and the actual probability of retaining the suction drain at the median DDASD. Furthermore, receiver operating characteristic (ROC) curves were generated to assess the sensitivity and specificity of the nomogram-predicted probability of retaining the suction drain. The area under the curve (AUC) value with a 95% CI was also calculated.
Statistical analyses
All statistical analyses were conducted using R software version 4.0.012. Two-sided P values < 0.05 were considered statistically significant.
Ethical approval
This article is a retrospective review of patient data, and the study design was approved by the Medical Ethics Committee of Northern Jiangsu People's Hospital. This article does not contain any studies with animals or human participants performed by any of the authors. All methods were carried out in accordance with relevant guidelines and regulations.
Informed consent
For this type of study formal consent is not required, and the need for informed consent was waived by approving ethics committee.
Results
Clinicopathological characteristics of patients
As shown in Table 1, 729 patients were included in the training cohort and 243 in the validation cohort. The median DDCSD and median DDASD of all patients were 5 days (ranging 4–8 days) and 11 days (ranging 5–21 days), respectively. No statistically significant difference was found between the training and validation cohorts.
Screening for independent predictors of DDASD and developing the nomogram
The results of univariate and multivariate Cox analyses in the training cohort are shown in Table 2. The univariate analysis showed that BMI, hypertension, TLNs, ratio of PLNs, PLNs, albumin level, and age correlated with the DDASD (P < 0.05). These variables were fitted into a multivariate Cox model. The VIF values of all variables were less than 2, indicating no collinearity among variables. BMI, albumin, hypertension, TLNs, and ratio of PLNs were independent predictors of DDASD. Furthermore, hypertension led to a longer DDASD (hazard ratio < 1). The increases in BMI, TLNs, and ratio of PLNs were associated with a longer DDASD (hazard ratio < 1). The increase in the albumin level was associated with a shorter DDASD (hazard ratio > 1). A nomogram was constructed based on the results of the multivariate Cox model to predict the probability of DDASD equal to or more than 11 days and median DDASD (Fig. 1).
Calibration and validation of the nomogram
The calibration plots of the nomogram in the training and validation cohorts are presented in Fig. 2. A prediction probability of DDASD ≥ 11 days of more than 40% for the groups was considered slightly underestimated, while a probability of less than 40% was pretty accurate. On the whole, a good concordance existed between the predicted and actual probabilities.
The C-index of the nomogram in the training and validation cohorts was 0.727 (95% CI 0.704–0.749) and 0.73 (95% CI 0.694–0.766), indicating good discrimination of this model. The ROC of the nomogram-predicted probability of DDASD ≥ 11 days is shown in Fig. 3. The AUC value of the ROC in the training cohort and validation cohort was 0.846 (95% CI 0.817–0.875) and 0.849 (95% CI 0.801–0.897), respectively, implying that the nomogram had good sensitivity and specificity in diagnosing patients with the DDASD equal to or more than 11 days.
Receiver-operating characteristic curves (ROCs) for evaluating the performance of the nomogram-predicted probability of drainage duration of axillary suction drain ≥ 11 days in the training cohort and validation cohort. (A) The ROC curve in the training cohort indicates an area under the curve (AUC) of 0.846 (95% CI 0.817–0.875). (B) In the validation cohort, the ROC indicates an AUC of 0.849 (95% CI 0.801–0.897).
Discussion
Prevention of complications is an important part of the postoperative management of patients with BC. The use of a suction drain after MRM can significantly reduce the occurrence of seroma formation and infection13,14. However, prolonged drainage duration increases the risk of infection, as the drain itself may allow germs into the wound15. In addition, later removal of the suction drain also delays the opportunity for postoperative functional exercise, leading to a series of consequences, such as arm lymphedema, restriction of the shoulder movement, and self-care disorders16. Therefore, appropriate drainage duration is vital for the postoperative rehabilitation of patients with BC.
Some previous studies concluded that the suction drain should be removed when the drainage volume is 20–50 mL or less in 24 h17,18,19. In this study, the criterion for drain removal was total drain output of 20 mL or less daily for 2 days starting from postoperative day 3, which not only reduced the occurrence of postoperative subcutaneous effusion but also did not prolong the drainage duration too much. The median DDASD in this study was 11 days. Although it was longer than that reported in previous studies18, most patients accepted it. The DDASD exceeded 21 or even 30 days in a few patients. Hence, it was presumed that some larger lymphatic vessels might not be reached by an ultrasonic scalpel during the surgery, or the suture ligating the lymphatic vessels might loosen, resulting in lymphorrhagia20. To avoid the subsequent bias, patients whose DDASD exceeded 21 days were excluded.
Multivariate Cox analysis was performed in the training cohort, revealing several independent predictors. A high BMI significantly correlated with an increased risk of prolonged drainage duration. An interpretation for this might be as follows: obese patients usually had longer surgical time, larger surgical wounds, and richer subcutaneous adipose tissue than ordinary patients, leading to graver adipose tissue liquefaction by the thermal injury during the surgery21,22. Moreover, the poor blood supply of subcutaneous adipose tissue in obese patients also delayed wound healing, which also caused adipose tissue liquefaction, necrosis, and subcutaneous fluid after the operation, thus prolonging the duration of drainage23. The present study found that a longer drainage duration was significantly associated with the dissection of more lymph nodes, which was consistent with previous findings24,25. Some studies found that the drainage fluid produced during the early postoperative period of MRM was produced mainly by the leakage of blood vessels and lymphatic vessels destroyed during the surgery17. Gong et al. reported that the ligation of all lymphatic vessels connecting to the dissected lymph node specimens significantly reduced the postoperative drainage volume in patients who underwent MRM compared with the use of electrocautery or scalpel26. The ratio of PLNs was found to be an important predictor of drainage duration in this study. Petrek et al. shared a similar view on this27. A previous study showed that a large number of new lymphatic vessels were produced in the body due to the obstruction of lymphatic circulation after axillary lymph node metastasis28. Besides, excessive dissection of axillary lymph nodes and the destruction of more blood vessels and lymphatic vessels might also lead to an increase in postoperative drainage volume27. Hypertension has been shown as a significant predictor of drainage duration in many previous studies6,7,8,10. The fragility of capillaries and lymphatics were found to be increased in hypertensive patients, causing more postoperative bleeding and wound ooze. Meanwhile, a long-term history of hypertension was more likely to cause sodium-water retention, which might inhibit lymphatic circulation, thus increasing the risk of wound ooze and prolonging the drainage duration29. However, the relationship between the serum albumin level and postoperative drainage duration could not be explained. It was speculated that a low serum albumin level caused a decrease in plasma colloid osmotic pressure, thus increasing the volume of postoperative drainage fluid under the stimulation of vessel injury caused by surgery. Besides, a low serum albumin level might decrease the resistance to infection, thus prolonging the healing time of wounds and increasing the postoperative drainage volume.
The predictive model constructed in this study can help clinicians in clinical work. Using this model, clinicians can predict the estimated postoperative drainage duration and keep patients informed about the possible hospitalization days, eliminating their concerns to some extent. Clinicians can also identify patients with high probabilities of retaining the suction drain and take early intervention measures such as albumin infusion for patients with low serum albumin level. Moreover, patients with prolonged predicted drainage duration can be discharged home with the axillary suction drain when they recover well after surgery, which can decrease hospitalization days and costs of patients.
This study had some limitations. First, chemotherapy and the duration of elastic bandage use might influence postoperative drainage duration13,24; the present study had insufficient data on this, leading to a bias. Second, the participants in this study were from a single center in China, and therefore the predictive model might not be applicable to other centers. Furthermore, inevitable selection bias might have affected the conclusions due to the retrospective design of the study.
This study is novel in developing a nomogram for predicting drainage duration in patients with BC undergoing MRM. Undoubtedly, the nomogram can provide information for the postoperative drainage duration management of these patients. In addition, the sample size of this study was much larger than that of previous studies, increasing the statistical power and made the results more plausible.
Conclusions
The study found out that BMI, serum albumin level, hypertension, TLNs, and ratio of PLNs were independent predictors of drainage duration in patients undergoing MRM. Based on this, a nomogram was constructed to predict the median postoperative drainage duration. The nomogram could predict the probability of retaining the suction drain during drainage, thus assisting clinicians in providing better and individualized postoperative management for patients with BC.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424. https://doi.org/10.3322/caac.21492 (2018).
McDonald, E. S., Clark, A. S., Tchou, J., Zhang, P. & Freedman, G. M. Clinical diagnosis and management of breast cancer. J. Nucl. Med. 57(Suppl 1), 9s–16s. https://doi.org/10.2967/jnumed.115.157834 (2016).
National Comprehensive Cancer Network (2019) NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines). Breast Cancer Version 1.2019. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed 21 Feb 2020.
Osteen, R. T. & Karnell, L. H. The National Cancer Data Base report on breast cancer. Cancer 73, 1994–2000. https://doi.org/10.1002/1097-0142(19940401)73:7%3c1994::aid-cncr2820730735%3e3.0.co;2-o (1994).
Ouldamer, L. et al. Dead space closure with quilting suture versus conventional closure with drainage for the prevention of seroma after mastectomy for breast cancer (QUISERMAS): Protocol for a multicentre randomised controlled trial. BMJ Open 6, e009903. https://doi.org/10.1136/bmjopen-2015-009903 (2016).
Burak, W. E. Jr., Goodman, P. S., Young, D. C. & Farrar, W. B. Seroma formation following axillary dissection for breast cancer: Risk factors and lack of influence of bovine thrombin. J. Surg. Oncol. 64, 27–31. https://doi.org/10.1002/(sici)1096-9098(199701)64:1%3c27::aid-jso6%3e3.0.co;2-r (1997).
Loo, W. T. & Chow, L. W. Factors predicting seroma formation after mastectomy for Chinese breast cancer patients. Indian J. Cancer 44, 99–103. https://doi.org/10.4103/0019-509x.38940 (2007).
Akinci, M., Cetin, B., Aslan, S. & Kulacoglu, H. Factors affecting seroma formation after mastectomy with full axillary dissection. Acta Chir. Belg. 109, 481–483. https://doi.org/10.1080/00015458.2009.11680464 (2009).
Iida, S. et al. An analysis of factors that influence the duration of suction drainage in breast cancer surgery. J. Nippon Med. School 75, 332–336. https://doi.org/10.1272/jnms.75.332 (2008).
Kumar, S., Lal, B. & Misra, M. C. Post-mastectomy seroma: A new look into the aetiology of an old problem. J. R. Coll. Surg. Edinb. 40, 292–294 (1995).
Balachandran, V. P., Gonen, M., Smith, J. J. & DeMatteo, R. P. Nomograms in oncology: More than meets the eye. Lancet Oncol. 16, e173-180. https://doi.org/10.1016/s1470-2045(14)71116-7 (2015).
R Core Team. R: A language and environment for statistical computing. https://www.R-project.org/. (R Foundation for Statistical Computing, Vienna, 2020).
Agrawal, A., Ayantunde, A. A. & Cheung, K. L. Concepts of seroma formation and prevention in breast cancer surgery. ANZ J. Surg. 76, 1088–1095. https://doi.org/10.1111/j.1445-2197.2006.03949.x (2006).
Horgan, K., Benson, E. A., Miller, A. & Robertson, A. Early discharge with drain in situ following axillary lymphadenectomy for breast cancer. Breast 9, 90–92. https://doi.org/10.1054/brst.2000.0142 (2000).
Chen, C. F., Lin, S. F., Hung, C. F. & Chou, P. Risk of infection is associated more with drain duration than daily drainage volume in prosthesis-based breast reconstruction: A cohort study. Medicine 95, e5605. https://doi.org/10.1097/md.0000000000005605 (2016).
Gençay Can, A., Ekşioğlu, E. & Çakçı, F. A. Early detection and treatment of subclinical lymphedema in patients with breast cancer. Lymphatic Res. Biol. 17, 368–373. https://doi.org/10.1089/lrb.2018.0033 (2019).
Srivastava, V., Basu, S. & Shukla, V. K. Seroma formation after breast cancer surgery: What we have learned in the last two decades. J. Breast Cancer 15, 373–380. https://doi.org/10.4048/jbc.2012.15.4.373 (2012).
Okada, N. et al. Early removal of drains and the incidence of seroma after breast surgery. Breast Cancer 22, 79–83. https://doi.org/10.1007/s12282-013-0457-3 (2015).
Kottayasamy Seenivasagam, R., Gupta, V. & Singh, G. Prevention of seroma formation after axillary dissection—A comparative randomized clinical trial of three methods. Breast J. 19, 478–484. https://doi.org/10.1111/tbj.12164 (2013).
Iovino, F., Auriemma, P. P., Ferraraccio, F., Antoniol, G. & Barbarisi, A. Preventing seroma formation after axillary dissection for breast cancer: A randomized clinical trial. Am. J. Surg. 203, 708–714. https://doi.org/10.1016/j.amjsurg.2011.06.051 (2012).
Lumachi, F. et al. Seroma prevention following axillary dissection in patients with breast cancer by using ultrasound scissors: A prospective clinical study. Eur. J. Surg. Oncol. 30, 526–530. https://doi.org/10.1016/j.ejso.2004.03.003 (2004).
Theunissen, D., Cant, P. J. & Dent, D. M. Factors that influence volume and duration of wound drainage after mastectomy and level III axillary node clearance. Breast 10, 538–539. https://doi.org/10.1054/brst.2001.0286 (2001).
Maaskant-Braat, A. J. et al. Sentinel Node and Recurrent Breast Cancer (SNARB): Results of a nationwide registration study. Ann. Surg. Oncol. 20, 620–626. https://doi.org/10.1245/s10434-012-2625-7 (2013).
Zielinski, J., Jaworski, R., Irga, N., Kruszewski, J. W. & Jaskiewicz, J. Analysis of selected factors influencing seroma formation in breast cancer patients undergoing mastectomy. Arch. Med. Sci. 9, 86–92. https://doi.org/10.5114/aoms.2012.29219 (2013).
Isozaki, H., Yamamoto, Y., Murakami, S., Matsumoto, S. & Takama, T. Impact of the surgical modality for axillary lymph node dissection on postoperative drainage and seroma formation after total mastectomy. Patient Saf. Surg. 13, 20. https://doi.org/10.1186/s13037-019-0199-z (2019).
Gong, Y. et al. Prevention of seroma formation after mastectomy and axillary dissection by lymph vessel ligation and dead space closure: A randomized trial. Am. J. Surg. 200, 352–356. https://doi.org/10.1016/j.amjsurg.2009.10.013 (2010).
Petrek, J. A. et al. Axillary lymphadenectomy. A prospective, randomized trial of 13 factors influencing drainage, including early or delayed arm mobilization. Arch. Surg. 125, 378–382. https://doi.org/10.1001/archsurg.1990.01410150100018 (1990).
Mumprecht, V. & Detmar, M. Lymphangiogenesis and cancer metastasis. J. Cell Mol. Med. 13, 1405–1416. https://doi.org/10.1111/j.1582-4934.2009.00834.x (2009).
Twelves, D. et al. The feasibility of nipple aspiration and duct lavage to evaluate the breast duct epithelium of women with increased breast cancer risk. Eur. J. Cancer 49, 65–71. https://doi.org/10.1016/j.ejca.2012.07.012 (2013).
Acknowledgements
The authors would like to thank all the reviewers who participated in the review and MJEditor (http://www.mjeditor.com) for its linguistic assistance during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
S.W. analyzed the data and wrote the manuscript. Z.X. contributed significantly to the revision of the manuscript and helped to process the raw data. D.S., Z.O., H.B., S.Z. and X.W. collected the data. J.Z. designed the study and helped to analyze the data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, S., Xin, Z., Sui, D. et al. Development and validation of a nomogram to predict drainage duration in patients with breast cancer treated with modified radical mastectomy. Sci Rep 11, 2533 (2021). https://doi.org/10.1038/s41598-021-82073-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-82073-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.