Abstract
Weight reduction continues to be first-line therapy in the treatment of hypertension (HTN). However, the long-term effect of bariatric malabsorptive surgical techniques such as Roux-en-Y Gastric Bypass (RYGB) surgery in the management of hypertension (HTN) is less clear. African Americans (AA) are disproportionately affected by obesity and hypertension and have inconsistent outcomes after bariatric surgery (BS). Despite a plethora of bariatric literature, data about characteristics of a predominantly AA bariatric hypertensive cohort including hypertension in obese (HIO) are scarce and underreported. The aims of this study were, (1) to describe the preoperative clinical characteristics of HIO with respect to HTN status and age, and (2) to identify predictors of HTN resolution one year after RYGB surgery in an AA bariatric cohort enrolled at the Howard University Center for Wellness and Weight Loss Surgery (HUCWWS). In the review of 169 AA bariatric patients, the average BMI was 48.50 kg/m2 and the average age was 43.86 years. Obese hypertensive patients were older (46 years vs. 37.89 years; p < .0001); had higher prevalence of diabetes mellitus (DM, 43.09% vs. 10.87%; p < .0001) and dyslipidemia (38.2% vs. 13.04%; p 0.002). Hypertensive AA who were taking ≥ 2 antihypertensive medications prior to RYGB were 18 times less likely to experience HTN resolution compared to hypertensive AA taking 0–1 medications, who showed full or partial response. Also, HIO was less likely to resolve after RYGB surgery in patients who needed ≥ 2 antihypertensive medications prior to surgical intervention.
Similar content being viewed by others
Introduction
Obesity, which afflicts one third of the United States population, is defined as body mass index (BMI) of ˃30 kg/m21. In 2017–2018, the prevalence of adult obesity in USA was 42.4%, an increase of 30.5% from 1999–20002. The age-adjusted prevalence of severe obesity at 9.2% was higher in women than in men; whereas the overall prevalence of obesity was highest in non-Hispanic black women (56.9%) compared to Hispanic women (43.7%), non-Hispanic white women (39.8%), and non-Hispanic Asian women (17.2%)2. In fact, non-Hispanic black women had the highest percentage of obesity among all races and age groups since 20112. This is also further complicated by the current COVID-19 pandemic in which BMI and hypertension (HTN) linked to obesity may be central to understanding the disproportionate number of African American COVID‐19 mortality3,4. The overall total health-care costs attributable to epidemic obesity and overweight are significant and are projected to double every decade5,6.
Obesity is a complex disease, and its pathophysiology is multifaceted. Growing evidence in basic science and clinical literature suggests that obesity is a disorder of the energy homeostasis system7. Beyond diet, the interplay between genetic and environmental factors along with socioeconomic status and unhealthy lifestyle can confer obesity pathogenesis8,9. How these disparate inputs interact with genetic, epigenetic and developmental factors that predispose to obesity is a critical question for future studies. Currently, it is known that genetic susceptibility, decreasing estrogen levels, medication use and physical inactivity contribute to midlife obesity in menopausal women10,11,12,13. In some cases, underlying causes may be gene mutations in leptin–melanocortin pathway, endocrine and psychiatric disorders14,15. The obesity pathophysiology further extends to renal hemodynamics that is indicative of renal fatty acid uptake and alterations in metabolic effects16,17,18,19,20. Also, a substantial segment of obese patients presents with obstructive sleep apnea (OSA)21. Both renal hemodynamics and OSA can also result in significant improvement following surgical weight reduction21,22,23.
Obesity is an independent risk factor for diabetes mellitus (DM), cardiovascular disease (CVD), chronic kidney disease (CKD) and hypertension (HTN), the latter being the most common obesity-related comorbidity22,24,25,26,27,28,29. Increased CVD is attributed to increased adrenergic (or sympathetic) activity in essential (aka primary) HTN, which leads to a drastic elevation in heart failure30,31,32.
The special case of hypertension in obese (HIO), which is difficult to clinically dissociate from HTN due to obesity, is multifactorial and not simple to distinguish from primary HTN, which has unknown secondary cause. This reflects the lack of a standard definition for hypertension in obesity. The predominantly known pathways linking obesity to HTN include increased mechanical load; sympathetic nervous system stimulation; salt and water retention; insulin resistance (IR) and even alterations in the gut hormone profile and neural activity15,33,34,35,36. Obese individuals usually present with HTN at a younger age compared to individuals with primary HTN. But even in early presentation, HIO is less likely to be adequately controlled and medical intervention for weight loss has failed to show consistent benefit in terms of its resolution37,38.
Surgical intervention such as bariatric surgery (BS) as shown in the Gateway Randomized Trial39, is currently the most effective treatment modality for morbid obesity and HIO28,29. Bariatric surgery also serves as a practical approach for blood pressure control, sustained weight loss, and prevention of CVDs in obese patients with HTN39,40. However, the long-term management of BS in isolated HTN and its association with race remain unclear. The data show that in various bariatric cohorts, the rate of HTN resolution at 1-year post BS ranges from 38.8 to 59.6%28,29,41. Prevalence of HTN is highest and its resolution lowest among African Americans (AA) undergoing BS compared to other racial and ethnic groups42,43,44. Income brackets and bariatric surgery access45 as well as outcomes including weight-loss and comorbidity resolution46,47 in states such as Michigan and Texas, for example, differ between blacks and whites where blacks have higher rate of 30-day complications and lower weight loss at 1 year following Roux-en-Y gastric bypass (RYGB) surgery. Among comorbidities, the Gateway Randomized Trial noted that recent research efforts on BS heavily focused on metabolic and DM resolution, but not on hypertension39. Several recent meta-analyses48 and similar studies related to post-RYGB surgeries have also suggested that race is an important determinant of weight loss and comorbidity remission49,50,51,52,53,54,55,56,57,58,59. In most studies60, AAs were relatively underrepresented and did not account for several other comorbidities related to metabolic syndrome in AA obese women61,62,63,64,65,66.
In our study, the participants underwent RYGB and were predominantly AA obese women. There is a relative paucity of data about the features of HIO in AA seeking BS and the predictors of its resolution after RYGB surgery. We conducted this retrospective study (1) to describe the preoperative clinical characteristics HIO with respect to HTN status and age; and (2) to identify predictors of HIO resolution 1 year after RYGB surgery in an AA bariatric cohort enrolled at the Howard University Center for Wellness and Weight Loss Surgery (HUCWWS). Data were collected by review of medical records maintained at the HUCWWS.
Materials and methods
All experimental protocols, methods and ethical requirements were carried out in accordance with relevant guidelines and regulations of the Howard University Office of Regulatory Research Compliance (ORRC) and the Institutional Review Board Committee (HU-IRB), which approved the waiver (exemption) for informed patient consent and granted the approval for the medical chart review (IRB-16-CMED-30 and IRB-12-CMED-29) (HU-IRB) for this study. In this cohort study, the de-identified patient medical records that were maintained at HUCWWLS between 2007 and 2013 were reviewed. Patients with a body mass index (BMI) ≥ 40 kg/m2 or a BMI ≥ 35 kg/m2 with associated comorbidities; enrolled in the bariatric surgery program to undergo non-revision sleeve gastrectomy (SG) or Roux-en-Y Gastric Bypass (RYGB); and self-identified as African American were included in the study. Data about preoperative clinical characteristics, within 1 month prior to BS such as age, gender, BMI, blood pressure, heart rate, creatinine and comorbidities were collected. The diagnosis of HTN (≥ 140/90 mmHg), DM (≥ 126 mg/dl (7 mmol/L), hypercholesterolemia (> 200 mg/dl) and obstructive sleep apnea (OSA) was extracted from each patient’s active list of medical problems as entered by the treating physician.
Preoperative clinical characteristics (within 1 month prior to bariatric surgery) of obese AA with HTN were compared to obese AA without HTN (normotensives) in overall cohort; and then among two age groups of < 40 years and ≥ 40 years. Next, a subset of patients who underwent RYGB surgery and had one-year follow-up data available were analyzed. Within this subset, we identified patients who had no continued need for anti-hypertensive medications (responders) and patients who continued to need anti-hypertensive medications (non-responders) at 1 year after RYGB. Therefore, reduction in the number of medications was used as a criterion for a partial response to BS. Positive responders were then compared to non-responders in terms of their pre-operative baseline comorbidities, pre-operative medications and pre-operative pulse pressure to identify independent predictors of HTN resolution after RYGB surgery in African American bariatric patients.
We used descriptive statistics to assess patient baseline clinical and demographic factors associated with HTN. For categorical variables, we obtained the counts (proportions) and evaluated significant differences using chi-square or Fisher’s exact test. We performed Analysis of variance (ANOVA) for continuous variables to assess significance for any differences in means among subjects with/without HTN; Wilcoxon’s rank-sum test was applied for comparisons of non-normal continuously distributed data. We conducted a univariate analysis to assess potential confounders. We performed a multivariate logistic regression analyses to determine significant independent predictors of having HTN and HTN resolution. Variables that were significantly associated with HTN and HTN resolution were included in a multivariate logistic regression analysis. In the logistic regression, variables are presented as odds ratios and confidence intervals. P-values less than 0.05 were considered statistically significant and confidence intervals (CI) are calculated at the 95% level. Data analysis was conducted using the Statistical Analysis System software 9.3 (SAS Institute, Cary, NC) and Statistical Analysis and Graphics (NCSS 9.0.7, Kaysville, UT). Fisher Exact Test was implemented to calculate p-values for fatty liver contribution to HTN at pre-op and post-op events because some of the cells had values below 5.
Results
Clinical characteristics of HIO in the African American bariatric cohort
In this retrospective chart review of 169 African American bariatric patients, 86% were female, 67% were ≥ 40 years of age and 73% had HTN within 1 month of the planned bariatric intervention. The average BMI of the overall cohort was 48.50 kg/m2 and the average age was 43.86 years. Obese hypertensive patients were older (46 years vs. 37.89 years; p < 0.0001); had higher prevalence of DM (43.09% vs. 10.87%; p < 0.0001) and dyslipidemia (38.2% vs. 13.04%; p 0.002). BMI and prevalence of obstructive sleep apnea were not significantly different between the two groups. Table 1 compares the baseline characteristics of obese normotensive and obese hypertensive AAs enrolled to undergo non-revisional sleeve gastrectomy (n = 31) or RYGB (n = 138) surgery at HUCWWLS. Obese hypertensives were older (46 years vs. 37.89 years; p < 0.0001); had higher prevalence of DM (43.09% vs. 10.87%; p < 0.0001) and dyslipidemia (38.2% vs. 13.04%; p 0.002). BMI and prevalence of obstructive sleep apnea were not significantly different between the two groups. Multivariate analysis adjusting for baseline factors associated with HTN showed that obese hypertensive patients were more likely to be older and were 5 times more likely to have DM compared to obese normotensive patients (see Table 2).
This cohort was further divided into two age groups (< 40 years and ≥ 40 years) and the baseline clinical characteristics were compared between obese normotensive and obese hypertensive AA patients (Table 3). This subgroup analysis showed that in patients younger than 40 years, there was no significant relationship between DM and HTN; univariate analysis showed that obese hypertensive patients were about 5 years older (34.47 years versus 29.04 years with p-value 0.0004) and had approximately 10 mm Hg higher pulse pressure (53.38 mm Hg versus 43.79 mm Hg p-value 0.037) driven by significantly elevated systolic blood pressure, compared to the obese normotensive AA patients. These differences were not significant after multivariate analysis.
Table 4 shows the number of participants with pre-operative hypertensive medications by age group (i.e. between < 40- and > 40-year-old groups). It is clear from the table that pre-operatively multiple medications are used more often and at a higher percentage by the > 40-year-old hypertensive patients than the younger age groups.
In patients 40 years of age or older, obese hypertensive AA patients were 8 times more likely to have DM compared to obese normotensive AA patients irrespective of their BMI and this relationship-maintained significance even after multivariate analysis was performed (Table 5). Pre-operative pulse pressure was elevated in both obese normotensives and obese hypertensives with no significant between group difference (51.27 versus 53.32; p-value 0.392).
Clinical characteristics associated with non-resolution of hypertension 1-year after RYGB surgery in the African American bariatric cohort
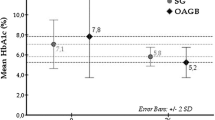
A subset of 133 patients who underwent RYGB was then evaluated. This group comprised predominantly of women (83%), with a mean age of 47 years and mean BMI of 49 kg/m2. Data about HTN status at 1-year after RYGB were available for only 57 patients. HTN remission rate at 1-year after RYGB surgery in this cohort was 49%. There were no significant differences in baseline clinical characteristics (Table 6) between positive responders and non-responders. However, multivariate logistic regression analysis showed that taking 0–1 antihypertensive medications and lower BMI pre-operatively were significantly associated with resolution of HTN after RYGB surgery in this African American bariatric cohort (Table 7). Hypertensive patients who were taking ≥ 2 antihypertensive medications pre-operatively were 18 times more likely to experience HTN non-resolution after RYGB surgery compared to hypertensive patients taking 0–1 medications. Thus, reduction in the number of medications can serve as a criterion for albeit partial response to RYGB-related surgical weight reduction.
Discussion
In our study, the participants had a high average income ($86,000) and had access to good nutrition that were either absent or scarce to many AA obese women studied in the past. Also, the very rare obesity studies that were conducted among the AA population were not associated with HTN and type 2 DM that disproportionally affect life expectancy in AA women. In a retrospective study by Shah et al., that looked at 3795 RYGB-operated obese patients, prevalence of pre-operative HTN was 40%67 and in the study by Flores et al.68, the prevalence of pre-operative HTN was 50%. Our study examined an AA bariatric cohort and showed a much higher prevalence of pre-operative HTN of 73%; 57% in patients aged < 40 years and 80% in patients aged ≥ 40 years. This finding is in concert with the latest NHANES data (https://www.cdc.gov/nchs/data/factsheets/factsheet_nhanes.pdf) that showed higher prevalence of obesity and HTN in non-Hispanic Blacks in both young and middle-age groups69. But, this may also reflect that African American patients seek bariatric intervention at a higher comorbidity burden, perhaps due to different health behaviors.
Our study highlights the differences in the clinical characteristics of obese hypertensives versus obese normotensives overall and in relation to age in AA, who have been previously under-represented in bariatric studies. Both age and DM were significantly associated with HTN in our study, consistent with the Lilliam Flores et al. study68. Our analysis shows that in obese AA aged ≥ 40 years, the prevalence of DM is eight times more in patients with HTN versus without HTN regardless of the body mass index, which is likely related to the metabolic syndrome. But association between HTN and DM was not significant in younger patients aged < 40 years.
The co-occurrence of HTN, DM and obesity is referred to as metabolic syndrome (MetS) diagnosed when any of the following three out of five clinical risk factors are present70: impaired fasting serum glucose; low levels of serum high-density lipoprotein (HDL) cholesterol; elevated serum triglycerides (i.e. Hypertriglyceridemia); central obesity and HTN. The prevalence of metabolic syndrome increases with age and disproportionately affects AA71,72,73. This was seen in our bariatric cohort as well. Interestingly, despite comparable BMI, there was no increased prevalence of DM noted in the obese hypertensives compared to obese normotensives at age < 40 years. But, the prevalence of HTN increased from 57 to 80% and prevalence of DM increased from 28 to 48% after age 40 years, without notable change in BMI over time. This likely reflects the importance of duration of exposure to obesity and the related milieu in increasing the burden of cardiovascular comorbidities. Adipose tissue is not just a fat storage, but it is an endocrine organ. It secretes a variety of biologically active derivatives, such as angiotensinogen, adipokines, proinflammatory and inflammatory molecules (interleukin-1β, interleukin-6, tumor necrosis factor-α, C-reactive protein), reactive oxygen species, homeostasis modulating compounds and acute phase reaction proteins. This leads to a proinflammatory and prothrombotic state associated with vascular dysfunction leading to hypertension. In obese individuals, there is increase in circulating blood volume, increased heart rate, increased cardiac output, endothelial dysfunction and loss of arterial compliance (arterial stiffening), all contributing to HIO34,35.
Though our study is a small retrospective cohort study, it shows the interaction of age, HTN and DM in an obese African American bariatric cohort. Due to cross sectional nature, this study cannot establish temporal relationship between DM and HTN. Small sample size resulted in wide confidence intervals; nevertheless, there was a significant association between DM, age and HTN in African American bariatric patients. Waist circumference measurements were not available.
We also evaluated a small subset of patients who had one year follow up data available to identify clinical factors associated with resolution of HTN 1-year after bariatric surgery. As most of patients with available follow-up data had undergone RYGB, only this surgical cohort was analyzed. One year follow up rate was low at 43% and HTN resolution data was available only in 57 patients. This analysis showed that hypertensive patients who were taking ≥ 2 antihypertensive medications pre-operatively had a very high likelihood of non-resolution of hypertension one year after RYGB surgery. Poor follow up rate significantly limits conclusions from this analysis. However, the reduction observed in the number of medications post-RYGB surgery in our study can be used as a criterion for a recognizable response since it represents a less severe disease or even a well-controlled disease as exemplified in the Gateway Randomized Trials designed to assess the impact of BS in patients with obesity and hypertension39.
Also, information about other variables previously described to be associated with hypertension resolution such as duration of hypertension, percentage excess weight loss and pre-operative vitamin D levels was not available in the health records.
These findings contribute to our understanding of the bariatric African American cohort whose aging is associated with higher cardiovascular comorbidity burden. Also, obese African-American bariatric patients with pre-operative HTN who require none or at most 1 antihypertensive medication to control their blood pressure are much more likely to experience hypertension resolution at 1-year following bariatric surgery.
The limitations of this study include (1) retrospective nature, (2) small sample size, (3) lack of availability of anthropometric data other than BMI, (4) poor 1-year follow up rate, especially dietary habits, (5) lack of availability of excess body weight loss and (6) lack of generalizability.
For generalizability and addressing the limitations stated above, future longitudinal studies may be required to examine large multiethnic cohorts; further validation of the contribution of age and DM to HTN in obese individuals; evaluation of ethnic variations; refinement of the definition of “obesity related hypertension”; and the wholesome enhancement of treatment strategies aimed at HTN resolution in bariatric patients.
Abbreviations
- AA:
-
African American
- BMI:
-
Body Mass Index
- BS:
-
Bariatric surgery
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- HIO:
-
Hypertension in obese
- RYGB:
-
Roux-en-Y gastric bypass
- HUCWWS:
-
Howard University Center for Wellness and Weight Loss Surgery
- IR:
-
Insulin resistance
- MetS:
-
Metabolic syndrome
- NHB:
-
Non-Hispanic Black
- SG:
-
Sleeve gastrectomy
References
Ogden, C. L., Carroll, M. D., Fryar, C. D. & Flegal, K. M. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief 219, 1–8 (2015).
Hales, C. M., Carroll, M. D., Fryar, C. D. & Ogden, C. L. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief 360, 1–8 (2020).
Alkhatib, A. L. et al. BMI is associated with Coronavirus Disease 2019 intensive care unit admission in African Americans. Obesity (Silver Spring) 28, 1798–1801 (2020).
Katzmarzyk, P. T., Salbaum, J. M. & Heymsfield, S. B. Obesity, noncommunicable diseases, and COVID-19: A perfect storm. Am. J. Hum. Biol. 32, e23484 (2020).
Withrow, D. & Alter, D. A. The economic burden of obesity worldwide: A systematic review of the direct costs of obesity. Obes. Rev. 12, 131–141 (2011).
Wang, Y., Beydoun, M. A., Liang, L., Caballero, B. & Kumanyika, S. K. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 16, 2323–2330 (2008).
Schwartz, M. W. et al. Obesity pathogenesis: An endocrine society scientific statement. Endocr. Rev. 38, 267–296 (2017).
Locke, A. E. et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 518, 197–206 (2015).
Speakman, J. R. A nonadaptive scenario explaining the genetic predisposition to obesity: The “predation release” hypothesis. Cell. Metab. 6, 5–12 (2007).
Poggiogalle, E. et al. Does endogenous GLP-1 affect resting energy expenditure and fuel selection in overweight and obese adults?. J. Endocrinol. Invest. 41, 439–445 (2018).
Stokes, A. et al. Association of obesity with prescription opioids for painful conditions in patients seeking primary care in the US. JAMA Netw. Open 3, e202012 (2020).
Osland, E., Powlesland, H., Guthrie, T., Lewis, C. A. & Memon, M. A. Micronutrient management following bariatric surgery: The role of the dietitian in the postoperative period. Ann. Transl. Med. 8, S9 (2020).
Abel, W. M., Spikes, T. & Greer, D. B. A qualitative study: Hypertension Stigma among Black Women (J. Cardiovasc, Nurs, 2020).
Cooiman, M. I. et al. Genetic obesity and bariatric surgery outcome in 1014 patients with morbid obesity. Obes. Surg. 30, 470–477 (2020).
Zhang, Y. et al. Obesity: Pathophysiology and intervention. Nutrients 6, 5153–5183 (2014).
Rebelos, E. et al. Renal hemodynamics and fatty acid uptake: effects of obesity and weight loss. Am. J. Physiol. Endocrinol. Metab. 317, E871–E878 (2019).
Alkharaiji, M., Anyanwagu, U., Donnelly, R. & Idris, I. Effect of bariatric surgery on cardiovascular events and metabolic outcomes in obese patients with insulin-treated type 2 diabetes: A retrospective cohort study. Obes. Surg. 29, 3154–3164 (2019).
Pareek, M., Bhatt, D. L., Schiavon, C. A. & Schauer, P. R. Metabolic surgery for hypertension in patients with obesity. Circ. Res. 124, 1009–1024 (2019).
Lopez-Martinez, J. E. et al. The short-term effects of Roux-en-Y gastric bypass on renal excretion of sodium and its association with blood pressure. Obes. Surg. 30, 102–110 (2020).
Lascaris, B. et al. Cardiac structure and function before and after bariatric surgery: A clinical overview. Clin. Obes. 8, 434–443 (2018).
Priyadarshini, P. et al. Impact of bariatric surgery on obstructive sleep apnoea–hypopnea syndrome in morbidly obese patients. J. Minim Access Surg. 13, 291–295 (2017).
Li, K. et al. Effects of bariatric surgery on renal function in obese patients: A systematic review and meta analysis. PLoS ONE 11, e0163907 (2016).
Sillo, T. O. et al. The impact of bariatric surgery on the resolution of obstructive sleep apnoea. BMC Res. Notes 11, 385-018-3484–5 (2018).
Zhang, C., Rexrode, K. M., van Dam, R. M., Li, T. Y. & Hu, F. B. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation 117, 1658–1667 (2008).
Noppa, H., Bengtsson, C., Wedel, H. & Wilhelmsen, L. Obesity in relation to morbidity and mortality from cardiovascular disease. Am. J. Epidemiol. 111, 682–692 (1980).
Mokdad, A. H. et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 289, 76–79 (2003).
Kopelman, P. Health risks associated with overweight and obesity. Obes. Rev. 8(Suppl 1), 13–17 (2007).
Zhang, N. et al. Reduction in obesity-related comorbidities: Is gastric bypass better than sleeve gastrectomy?. Surg. Endosc. 27, 1273–1280 (2013).
Hallersund, P. et al. Gastric bypass surgery is followed by lowered blood pressure and increased diuresis—long term results from the Swedish Obese Subjects (SOS) study. PLoS ONE 7, e49696 (2012).
Poirier, P. et al. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 113, 898–918 (2006).
Floras, J. S. & Ponikowski, P. The sympathetic/parasympathetic imbalance in heart failure with reduced ejection fraction. Eur. Heart J. 36, 1974–1982 (2015).
Lymperopoulos, A., Rengo, G. & Koch, W. J. Adrenergic nervous system in heart failure: Pathophysiology and therapy. Circ. Res. 113, 739–753 (2013).
Hall, J. E., Crook, E. D., Jones, D. W., Wofford, M. R. & Dubbert, P. M. Mechanisms of obesity-associated cardiovascular and renal disease. Am. J. Med. Sci. 324, 127–137 (2002).
Youn, J. C. et al. Adiponectin and progression of arterial stiffness in hypertensive patients. Int. J. Cardiol. 163, 316–319 (2013).
Kotsis, V., Stabouli, S., Papakatsika, S., Rizos, Z. & Parati, G. Mechanisms of obesity-induced hypertension. Hypertens. Res. 33, 386–393 (2010).
Ding, C., Gao, D., Wilding, J., Trayhurn, P. & Bing, C. Vitamin D signalling in adipose tissue. Br. J. Nutr. 108, 1915–1923 (2012).
Singer, G. M. & Setaro, J. F. Secondary hypertension: obesity and the metabolic syndrome. J. Clin. Hypertens. (Greenwich) 10, 567–574 (2008).
Calhoun, D. A. Hyperaldosteronism as a common cause of resistant hypertension. Annu. Rev. Med. 64, 233–247 (2013).
Schiavon, C. A. et al. Effects of bariatric surgery in obese patients with hypertension: The GATEWAY randomized trial (gastric bypass to treat obese patients with steady hypertension). Circulation 137, 1132–1142 (2018).
Kuno, T., Tanimoto, E., Morita, S. & Shimada, Y. J. Effects of bariatric surgery on cardiovascular disease: A concise update of recent advances. Front. Cardiovasc. Med. 6, 94 (2019).
Dogan, K. et al. Effectiveness and safety of sleeve gastrectomy, gastric bypass, and adjustable gastric banding in morbidly obese patients: A multicenter, retrospective, Matched Cohort Study. Obes. Surg. 25, 1110–1118 (2015).
Egan, B. M., Zhao, Y., Axon, R. N., Brzezinski, W. A. & Ferdinand, K. C. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation 124, 1046–1058 (2011).
Decoste, M., Vanobberghen, R., Borgermans, L. & Devroey, D. Uncontrolled hypertension among black Africans in the city of Brussels: a case-control study. Eur. Rev. Med. Pharmacol. Sci. 17, 886–894 (2013).
Sundquist, J., Winkleby, M. A. & Pudaric, S. Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: an analysis of NHANES III, 1988–1994. Third National Health and Nutrition Examination Survey. J. Am. Geriatr. Soc. 49, 109–116 (2001).
Clapp, B. et al. Disparities in access to bariatric surgery in Texas 2013–2017. JSLS https://doi.org/10.4293/JSLS.2020.00016 (2020).
Wood, M. H. et al. Association of race with bariatric surgery outcomes. JAMA Surg. 154, e190029 (2019).
Turner, M. et al. Weight loss and co-morbidity resolution between different races and ethnicities after gastric bypass. Surg. Obes. Relat. Dis. 15, 1943–1948 (2019).
Admiraal, W. M. et al. Ethnic differences in weight loss and diabetes remission after bariatric surgery: A meta-analysis. Diabetes Care 35, 1951–1958 (2012).
Istfan, N. et al. Racial differences in weight loss, hemoglobin A1C, and blood lipid profiles after Roux-en-Y gastric bypass surgery. Surg. Obes. Relat. Dis. 12, 1329–1336 (2016).
Ng, J. et al. Ethnic variation in weight loss, but not co-morbidity remission, after laparoscopic gastric banding and Roux-en-Y gastric bypass. Surg. Obes. Relat. Dis. 11, 94–100 (2015).
Gullick, A. A. et al. Association of race and socioeconomic status with outcomes following laparoscopic Roux-en-Y gastric bypass. Obes. Surg. 25, 705–711 (2015).
Puzziferri, N. et al. Long-term follow-up after bariatric surgery: A systematic review. JAMA 312, 934–942 (2014).
Lewis, K. H., Edwards-Hampton, S. A. & Ard, J. D. Disparities in treatment uptake and outcomes of patients with obesity in the USA. Curr. Obes. Rep. 5, 282–290 (2016).
Miller-Matero, L. R., Tobin, E. T., Clark, S., Eshelman, A. & Genaw, J. Pursuing bariatric surgery in an urban area: Gender and racial disparities and risk for psychiatric symptoms. Obes. Res. Clin. Pract. 10, 56–62 (2016).
Khorgami, Z., Arheart, K. L., Zhang, C., Messiah, S. E. & de la Cruz-Munoz, N. Effect of ethnicity on weight loss after bariatric surgery. Obes. Surg. 25, 769–776 (2015).
Coleman, K. J. & Brookey, J. Gender and racial/ethnic background predict weight loss after Roux-en-Y gastric bypass independent of health and lifestyle behaviors. Obes. Surg. 24, 1729–1736 (2014).
Limbach, K. E., Ashton, K., Merrell, J. & Heinberg, L. J. Relative contribution of modifiable versus non-modifiable factors as predictors of racial variance in roux-en-Y gastric bypass weight loss outcomes. Obes. Surg. 24, 1379–1385 (2014).
Harvin, G., DeLegge, M. & Garrow, D. A. The impact of race on weight loss after Roux-en-Y gastric bypass surgery. Obes. Surg. 18, 39–42 (2008).
Elli, E. F. et al. Bariatric surgery outcomes in ethnic minorities. Surgery 160, 805–812 (2016).
Stanford, F. C. et al. Patient race and the likelihood of undergoing bariatric surgery among patients seeking surgery. Surg. Endosc. 29, 2794–2799 (2015).
Sugerman, H. J., Wolfe, L. G., Sica, D. A. & Clore, J. N. Diabetes and hypertension in severe obesity and effects of gastric bypass-induced weight loss. Ann. Surg. 237, 751–756 (2003).
Fitzgibbon, M. L. et al. Weight loss and African-American women: A systematic review of the behavioural weight loss intervention literature. Obes. Rev. 13, 193–213 (2012).
Gower, B. A. & Fowler, L. A. Obesity in African-Americans: The role of physiology. J. Intern. Med. 288, 295–304 (2020).
Kinsey, A. W. et al. Similar weight loss and maintenance in African American and White women in the Improving Weight Loss (ImWeL) trial. Ethn. Health, 1–13 (2018).
Buscemi, J. et al. Associations between fiber intake and Body Mass Index (BMI) among African-American women participating in a randomized weight loss and maintenance trial. Eat. Behav. 29, 48–53 (2018).
Tussing-Humphreys, L. M., Fitzgibbon, M. L., Kong, A. & Odoms-Young, A. Weight loss maintenance in African American women: A systematic review of the behavioral lifestyle intervention literature. J. Obes. 2013, 437369 (2013).
Shah, K. et al. Long-term effects of laparoscopic Roux-en-Y gastric bypass on metabolic syndrome in patients with morbid obesity. Surg. Obes. Relat. Dis. 12, 1449–1456 (2016).
Flores, L. et al. Hypertension remission 1 year after bariatric surgery: Predictive factors. Surg. Obes. Relat. Dis. 10, 661–665 (2014).
Lackland, D. T. Racial differences in hypertension: implications for high blood pressure management. Am. J. Med. Sci. 348, 135–138 (2014).
Rotman, Y. et al. The association of genetic variability in patatin-like phospholipase domain-containing protein 3 (PNPLA3) with histological severity of nonalcoholic fatty liver disease. Hepatology 52, 894–903 (2010).
Bonora, E. et al. Hyperinsulinemia and insulin resistance are independently associated with plasma lipids, uric acid and blood pressure in non-diabetic subjects. The GISIR database. Nutr. Metab. Cardiovasc. Dis. 18, 624–631 (2008).
Hildrum, B., Mykletun, A., Hole, T., Midthjell, K. & Dahl, A. A. Age-specific prevalence of the metabolic syndrome defined by the International Diabetes Federation and the National Cholesterol Education Program: The Norwegian HUNT 2 study. BMC Public Health 7, 220-2458-7–220 (2007).
Staiano, A. E. et al. Uncovering physiological mechanisms for health disparities in type 2 diabetes. Ethn. Dis. 25, 31–37 (2015).
Acknowledgements
Special thanks to Dr. Jason Umans for scientific critique. This project has been funded to C.G. in whole or in part with UL1TR000101 from the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through the Clinical and Translational Science Awards Program (CTSA), a trademark of DHHS, part of the Roadmap Initiative, “Re-Engineering the Clinical Research Enterprise." This work was also supported and funded by NIH/NCI subcontract U01CA185188 to Z.A.S.
Author information
Authors and Affiliations
Contributions
C.G. and Z.A.S. wrote the manuscript; C.G. and Z.A.S. conducted the study; C.G. reviewed patient medical record data supported by Z.A.S.; J.N. performed the statistical analysis; M.B. and A.M. assisted in reviewing the data; G.O. provided feedback; D.T., and T.F. were the surgeons that operated on the patients and also reviewed the original manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gandotra, C., Basam, M., Mahajan, A. et al. Characteristics and resolution of hypertension in obese African American bariatric cohort. Sci Rep 11, 1683 (2021). https://doi.org/10.1038/s41598-021-81360-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-81360-y
This article is cited by
-
Trends in blood pressure and hypertension among older adults and oldest-old individuals in China between 2008-2018
Hypertension Research (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.