Abstract
Sleep problems are common in Taiwan. Poor sleep may be associated with many illnesses, including substance use disorders. Ketamine use disorder has significantly increased in Taiwan in recent years and may lead to physical and cognitive problems. Craving for ketamine is a risk factor for ketamine use and relapse, and poor sleep quality may increase craving. This study aimed to explore the mediating effects of craving on the relationship between poor sleep quality and ketamine use. Demographic data, sleep quality, severity of dependence and craving were recorded for current ketamine users and abstinent ketamine users. Mediation analysis was used to examine the mediating effect of craving on the relationship between poor sleep and ketamine use. This study enrolled 414 current ketamine users with ketamine use disorder, 238 current ketamine users without ketamine use disorder, and 102 abstinent ketamine users with ketamine use disorder. Compared with healthy controls, all ketamine users had poor sleep quality. Poor sleep quality was associated with the initiation of and dependence on ketamine use. Craving can mediate the relationship between poor sleep quality and ketamine use. Poor sleep quality remains a problem for those abstaining from ketamine use. Poor sleep quality in ketamine users is an important issue because it is directly and indirectly through craving associated with ketamine use.
Similar content being viewed by others
Introduction
Sleep is an essential physiological process for many vital functions, including restoration of the body, maintenance of energy and modulation of psychological states1. Sleep problems are a prevalent public health issue with between 6 and 10% of the population meeting the diagnostic criteria for insomnia2,3. Furthermore, approximately one-third of the population experiences sleep problems at some point in their lives3,4. Regarding sleep problems, two cross-sectional surveys conducted in 2003 and 2005 showed that the most common sleep problem in Taiwan was insomnia5,6. The survey from 2003 revealed that the age-adjusted prevalence of insomnia, defined as difficulty initiating sleep, difficulty maintaining sleep and early morning waking, was 10.3%, which was higher than that in Japan and Korea5. Another survey of 36,743 participants aged 18 years and over in 2005 showed that more than 25% had insomnia6. A more recent study in Taiwan that used the Pittsburgh Sleep Quality Index (PSQI) to assess sleep quality indicated that up to 46.6% of the participants had poor sleep quality7. The authors also argued that the prevalence of poor sleep quality is progressively increasing. All of the above evidence indicates that poor sleep quality is an important health issue in Taiwan.
Ketamine was first introduced and remains widely used as an anesthetic for medical and veterinary use8. Reports of recreational use of ketamine can be traced back to 19789, followed by a report of ketamine as a club drug in the 1990s10. Consumption of ketamine can result in a variety of health problems, such as cognitive impairment, cystitis, and accidental death10,11. Previous studies have documented that ketamine use disorder develops among recreational ketamine users12,13. Information regarding the prevalence of this disorder has shown that the population of those using ketamine began to increase worldwide, particularly in Asia, after 200014,15. Compared with drugs such as heroin or amphetamine, ketamine is relatively inexpensive and easy to obtain in Taiwan. Therefore, the culture of drug use in Taiwan underwent a change. A study of drug-related seizures and arrests showed that ketamine has become an increasingly popular illicit substance in Taiwan16. A National Household Survey on Health and Substance Abuse conducted in a population aged 12–64 years in Taiwan in 2005 showed that ketamine was the third most commonly abused drug17. Knowledge of the underlying factors associated with ketamine use may provide insight into managing individuals suffering from ketamine use disorder because treatment for ketamine use disorder is not yet available18.
Craving may result in substance use and relapse of substance abuse in people with substance use disorders19. Poor sleep quality may increase craving in people with substance use disorders20,21. Poor sleep quality has previously been identified as a risk factor for cocaine, alcohol and opiate use22,23,24. Poor sleep quality is an important health issue in substance users, as complaints regarding sleep are common25; however, there has been little study of how poor sleep quality is related to ketamine use disorder and how craving mediates sleep quality and ketamine use. Sleep is a private experience, and the components and importance of sleep quality vary across individuals. Therefore, self-reported evaluations are essential to measure sleep quality. This study aimed to explore the relationships between self-reported sleep quality and ketamine use. We hypothesized that (1) poor sleep quality may be associated with the initiation of and dependence on ketamine use and (2) craving mediates the relationship between sleep quality and ketamine use.
Method
Participants
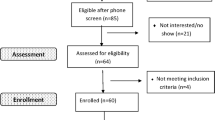
Ketamine users were recruited from the community and from a control environment, namely, from a number of drug rehabilitation centers. The inclusion criteria for participants from the community were as follows: (1) current ketamine use, (2) no other substance use disorders except tobacco use, and (3) no psychiatric diagnoses of schizophrenia, major depressive disorder or bipolar disorder. The inclusion criteria for participants in the control environment were as follows: (1) ketamine use disorder, (2) no other substance use disorders except tobacco use, and (3) no psychiatric diagnoses of schizophrenia, major depressive disorder or bipolar disorder. The healthy controls were those without any substance use disorder or mental illness and were age-, gender- and education-matched to the ketamine users. Initially, all participants, including current/abstinent ketamine users and healthy people, were interviewed by psychiatrists to assess whether or not participants had ketamine use disorder and fulfilled other inclusion criteria. If participants met the inclusion criteria, they underwent interviews and provided baseline data, including age, sex, severity of dependence, craving, sleep quality and mean money spent daily on ketamine use in the preceding week. Informed consent was obtained from all of the participants. The institutional review board of Kaohsiung Medical University approved the study protocol. All experiments were performed in accordance with relevant guidelines and regulations.
Assessments
Visual Analog Craving Scale (VACS)
We used the VACS, modified from previous studies26,27, to assess the level of craving in ketamine users from the community and control environment. The VACS consists of the following single question: how much did you crave/desire/want to use ketamine in the preceding week? The level of craving was rated from 0 (not at all) to 100 (very much).
Chinese-Mandarin version of the Severity of Dependence Scale (SDSch)
The SDSch, which consists of 5 questions, was used to measure the level of dependence on ketamine in the preceding week28. The score on the SDSch can range from 0 to 15 29.
Pittsburgh Sleep Quality Index (PSQI)
We used the PSQI to evaluate sleep quality over the preceding 1-month period. The PSQI is a self-reported questionnaire that is easy to administer30. It consists of 19 individual items to generate seven component scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The sum of the seven component scores yields one global score that indicates subjective sleep quality (range 0–21). A higher global score represents poorer subjective sleep quality. The Taiwanese version of the PSQI (PSQI-T) has good validity and reliability31. We used a cutoff point of five to indicate poor sleep quality7. We calculated rates of poor sleep quality based on PSQI-T > 5.
Data analysis
Comparison of sleep quality between the healthy controls, current ketamine users without ketamine use disorder, current ketamine users with ketamine use disorder, and abstinent ketamine users with ketamine use disorder was performed using analysis of variance (ANOVA). Tamhane’s T2 was used in the post hoc test to address unequal variances. The Chi-square (χ2) test was used to examine differences in categorical variables among groups. Analysis of covariance (ANCOVA) was used to compare sleep quality, craving and level of dependence among groups with the effects of age, gender, education and tobacco use adjusted for. We used a multinomial logistic regression model to explore the associations of poor sleep quality with different types of ketamine use behavior: never used ketamine, nonaddictive use and addictive use. Binary logistic regression was used to examine associations with poor sleep quality in those with addictive use, employing nonaddictive use as a reference. A mediation model was used to explore whether craving was a mediator of the relationship between poor sleep and the amount of money spent on ketamine32. The sequential Bonferroni procedure was used to adjust for multiple comparisons33.
Results
There were 844 people enrolled in this study, including 90 healthy controls and 754 ketamine users. Of the ketamine users, 102 (13.52%) had remained abstinent from ketamine for more than three months because they stayed in the control environment, while the others were current ketamine users from the community in South Taiwan. Furthermore, 414 (63.69%) of the current ketamine users from the community fulfilled the criteria for ketamine use disorder as set out in the DSM 5, while the others did not. Among all four groups (healthy controls, abstinent ketamine users with ketamine use disorder, current ketamine users with ketamine use disorder, and current ketamine users without ketamine use disorder), age, gender, education and tobacco use did not differ (Table 1).
There were significant differences in craving for ketamine and the severity of dependence among the current ketamine users without ketamine use disorder, current ketamine users with ketamine use disorder, and abstinent ketamine users with ketamine use disorder after adjusting for the effects of age, gender, education and tobacco use. In particular, the current and abstinent ketamine users with ketamine use disorder had higher levels of craving and a greater severity of dependence than the ketamine users without ketamine use disorder (craving: pcurrent ketamine users with ketamine use disorder < 0.001 and pabstinent ketamine users < 0.001; severity of dependence: pcurrent ketamine users with ketamine use disorder < 0.001 and pabstinent ketamine users < 0.001). The current ketamine users with ketamine use disorder did not differ in terms of the level of craving or the severity of dependence from the abstinent ketamine users with ketamine use disorder. The mean amount (SD) of money spent on ketamine was greater in the current ketamine users with ketamine use disorder than in those without ketamine use disorder (t = 506.54, p < 0.001).
Mean PSQI scores differed significantly among the healthy controls, current ketamine users with/without ketamine use disorder, and abstinent ketamine users after controlling for the effect of age and gender. Post hoc analysis showed that the healthy controls had the lowest mean PSQI score (pcurrent ketamine users without ketamine use disorder = 0.001; pcurrent ketamine users with ketamine use disorder < 0.001 and pabstinent ketamine users < 0.001), while the current ketamine users with ketamine use disorder had the highest (pcurrent ketamine users without ketamine use disorder < 0.001 and pabstinent ketamine users = 0.007). The current ketamine users without ketamine use disorder and the abstinent ketamine users did not significantly differ in terms of mean PSQI scores (p = 0.551). The rates of poor sleep in healthy controls, current ketamine users with/without ketamine use disorder and abstinent ketamine users significantly differed. The rate of poor sleep was significantly higher in the current ketamine users with ketamine use disorder than in the current ketamine users without ketamine use disorder (χ2 = 11.84, p = 0.001) and the abstinent ketamine users (χ2 = 7.30, p = 0.007). The rate of poor sleep in the current ketamine users without ketamine use disorder did not differ from that in the abstinent ketamine users (χ2 = 0.001, p = 0.973).
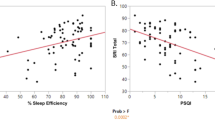
Multinomial logistic regression analysis showed that sleep quality was significantly associated with the status of ketamine use (Table 2). Poor sleep quality was significantly associated with current ketamine use with and without ketamine use disorder compared with the healthy controls. Furthermore, binary logistic regression in the current ketamine users indicated that poor sleep quality was a risk factor for ketamine use disorder. In addition, both sleep quality and craving for ketamine were associated with the amount of money spent on ketamine in current ketamine users with ketamine use disorder. Mediation analysis showed that poor sleep had an indirect effect via craving on the amount of money spent on ketamine (Table 3).
Discussion
This study found that (1) current ketamine users with and without ketamine use disorder and abstinent ketamine users had higher mean PSQI scores and higher rates of poor sleep quality than healthy controls; (2) poor sleep quality was associated with current nonaddictive or addictive ketamine use; and (3) craving may have mediated the relationship between sleep quality and money spent on ketamine. Poor sleep quality is a mental health issue not only for current ketamine users without ketamine use disorder but also for current ketamine users with ketamine use disorder compared to healthy people. Furthermore, the participants who had abstained from ketamine for more than three months also had sleep problems, which indicated that sleep problems were more prevalent in ketamine users regardless of the status of ketamine use than in healthy people. Therefore, mental health professionals should evaluate sleep quality when helping current and abstinent ketamine users.
Strong evidence has demonstrated the role of poor sleep quality in substance users in relation to an increased risk of relapse34,35. Therefore, poor sleep quality can be an indicator of a higher probability of relapse in abstinent ketamine users. In addition, the abstinent ketamine users with ketamine use disorder had a lower mean PSQI score and a lower rate of poor sleep quality than the current ketamine users with ketamine use disorder. This result was in line with previous studies involving cocaine and alcohol users, which showed that abstinence from these substances cannot completely reverse sleep problems23,36. However, studies on sleep quality in abstinent ketamine users are scarce. Due to the nature of the observational study, these results provided only preliminary evidence that ketamine users with ketamine use disorder do not experience complete remission in sleep quality after stopping ketamine use. Many factors may contribute to the presence of sleep problems in abstinent ketamine users. For example, sleep problems may have preceded the development of substance use25, and chronic substance use makes sleep problems worse37. Therefore, abstinence from substance use only partially reverses sleep problems. It would be worthwhile to explore the exact factors that contribute to poor sleep in abstinent ketamine users.
The present study found that poor sleep quality was associated with current ketamine use. Poor sleep was also associated with ketamine use disorder in current ketamine users. Information regarding how poor sleep is related to the status of ketamine use is limited. Roehr et al. reviewed previous studies on substances other than ketamine and argued that poor sleep may result in the initiation and maintenance of drug use25. Evidence has also indicated that sleep problems increased the risk of developing substance use disorders24,38. Our results provide evidence that poor sleep is also an indicator associated with the initiation of and dependence on ketamine use.
The analysis without mediation indicated that poor sleep was related to the amount of money spent on ketamine, which is an indicator of the amount of ketamine being used. The mediation analysis showed that the relationship between poor sleep and the amount of money spent on ketamine involves at least two pathways. One is a direct pathway, while the other is that poor sleep is related to money spent on ketamine by craving. Previous studies with substances other than ketamine demonstrated that poor sleep was positively associated with craving in substance users39,40. Our findings also demonstrated that poor sleep was positively associated with craving for ketamine, indicating a potential role of craving in mediating the relationship between sleep problems and ketamine use.
In conclusion, our findings raised some important implications for those with ketamine use disorder. First, sleep problems can persist in abstinent ketamine users. Second, sleep quality is important to ketamine use because poor sleep quality may be associated with increased risks of initiation and dependence. Third, the association between sleep problems and the amount of ketamine used may be indirect with craving as a mediator. Despite the current study having examined the associations between sleep quality, craving, and ketamine-related outcomes, there were limitations inherent in this investigation. First, we relied on self-reported data to measure sleep quality and ketamine-related outcomes. It is possible that these measurements contained errors and therefore may have biased our results. Objective sleep quality assessments by sleep monitoring devices can be used to reduce bias. Further study on the association between objective sleep qualities and ketamine use is warranted. Second, the use of cross-sectional data limited our ability to draw causal inferences regarding the determinants of poor sleep quality and ketamine use/outcomes. Third, the participants were voluntarily recruited. We enrolled participants meeting rigorous criteria and included variables in the analysis to reduce selection bias41,42. Fourth, fewer female participants may also limit the generalizability to the female population. Fifth, craving is a dynamic phenomenon. This may have contributed to levels of craving that were not high, because we asked about the average level of craving for the past week not the peak level of craving. Using the VACS to assess the mean level during the past week is feasible in studies of substance use disorder43. Sixth, fewer healthy controls were enrolled because we matched the controls to ketamine users by gender, age and education. Fewer healthy controls may have reduced the power of the analysis44. Enrolling more healthy controls while matching the low education level of the ketamine users is not easy in Taiwan because most healthy controls have higher education levels. Therefore, future studies with matched groups in a 1:1 ratio is warranted. This study was among few that have explored the relationship between sleep quality, craving and ketamine-related outcomes. By obtaining a better understanding of the role of sleep quality in ketamine users in relation to ketamine-related outcomes, we can make advances in devising more effective, personalized ketamine cessation interventions and relapse prevention strategies. Future research on the efficacy of clinical interventions designed to improve sleep quality in ketamine users is warranted to address cravings and promote cessation.
References
Zielinski, M. R., McKenna, J. T. & McCarley, R. W. Functions and mechanisms of sleep. AIMS Neurosci. 3, 67–104. https://doi.org/10.3934/Neuroscience.2016.1.67 (2016).
Ford, D. E. & Kamerow, D. B. Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention?. JAMA 262, 1479–1484 (1989).
Morin, C. M., LeBlanc, M., Daley, M., Gregoire, J. P. & Merette, C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 7, 123–130. https://doi.org/10.1016/j.sleep.2005.08.008 (2006).
Ohayon, M. M. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med. Rev. 6, 97–111 (2002).
Nomura, K., Yamaoka, K., Nakao, M. & Yano, E. Impact of insomnia on individual health dissatisfaction in Japan, South Korea, and Taiwan. Sleep 28, 1328–1332 (2005).
Kao, C. C., Huang, C. J., Wang, M. Y. & Tsai, P. S. Insomnia: prevalence and its impact on excessive daytime sleepiness and psychological well-being in the adult Taiwanese population. Qual. Life Res. 17, 1073–1080. https://doi.org/10.1007/s11136-008-9383-9 (2008).
Tai, S. Y., Wang, W. F. & Yang, Y. H. Current status of sleep quality in Taiwan: a nationwide walk-in survey. Ann. Gen. Psychiatry 14, 36. https://doi.org/10.1186/s12991-015-0078-7 (2015).
Pal, H., Berry, N., Kumar, R. & Ray, R. Ketamine dependence. Anaesthesia Intensive Care 30, 382–384 (2002).
Siegel, R. K. Phencyclidine and ketamine intoxication: a study of four populations of recreational users. NIDA Res. Monogr. 21, 119–147 (1978).
Morgan, C. J., Curran, H. V. & Independent Scientific Committee on Drugs. Ketamine use: a review. Addiction 107, 27–38. https://doi.org/10.1111/j.1360-0443.2011.03576.x (2012).
Freese, T. E., Miotto, K. & Reback, C. J. The effects and consequences of selected club drugs. J. Subst. Abuse Treat. 23, 151–156. https://doi.org/10.1016/S0740-5472(02)00267-2 (2002).
Critchlow, D. G. A case of ketamine dependence with discontinuation symptoms. Addiction 101, 1212–1213 (2006).
Goyal, S., Ambekar, A. & Ray, R. Ketamine dependence in an anesthesiologist: an occupational hazard?. Indian J. Psychol. Med. 36, 335–337. https://doi.org/10.4103/0253-7176.135395 (2014).
Drugs, U. N. O. & Crime. World drug report 2010. (United Nations Publications, 2010).
Li, J. H. et al. To use or not to use: an update on licit and illicit ketamine use. Subst. Abuse Rehabil. 2, 11–20. https://doi.org/10.2147/SAR.S15458 (2011).
Feng, L. Y. et al. Comparison of illegal drug use pattern in Taiwan and Korea from 2006 to 2014. Subst. Abuse Treat. Prev. Policy 11, 34. https://doi.org/10.1186/s13011-016-0078-x (2016).
Li, L.-H., Liang, K.-Y. & Wu, S.-I. National Bureau of Health Promotion National Bureau of Controlled Drugs, National Health Research Institutes, Department of Health, Taipei (2006).
Huang, M.-C., Chen, L.-Y., Chen, C.-K. & Lin, S.-K. Potential benefit of lamotrigine in managing ketamine use disorder. Med. Hypotheses 87, 97–100 (2016).
Tiffany, S. T. & Wray, J. M. The clinical significance of drug craving. Ann. N. Y. Acad. Sci. 1248, 1–17. https://doi.org/10.1111/j.1749-6632.2011.06298.x (2012).
Chen, B. et al. Sleep regulates incubation of cocaine craving. J. Neurosci. 35, 13300–13310. https://doi.org/10.1523/JNEUROSCI.1065-15.2015 (2015).
Freeman, L. K. & Gottfredson, N. C. Using ecological momentary assessment to assess the temporal relationship between sleep quality and cravings in individuals recovering from substance use disorders. Addict. Behav. 83, 95–101. https://doi.org/10.1016/j.addbeh.2017.11.001 (2018).
Roane, B. M. & Taylor, D. J. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep 31, 1351–1356 (2008).
Angarita, G. A. et al. Abstinence-related changes in sleep during treatment for cocaine dependence. Drug Alcohol Depend. 134, 343–347. https://doi.org/10.1016/j.drugalcdep.2013.11.007 (2014).
Angarita, G. A., Emadi, N., Hodges, S. & Morgan, P. T. Sleep abnormalities associated with alcohol, cannabis, cocaine, and opiate use: a comprehensive review. Addict. Sci. Clin. Pract. 11, 9. https://doi.org/10.1186/s13722-016-0056-7 (2016).
Roehrs, T. A. & Roth, T. Sleep disturbance in substance use disorders. Psychiatr. Clin. N. Am. 38, 793–803. https://doi.org/10.1016/j.psc.2015.07.008 (2015).
Culbertson, C. et al. Methamphetamine craving induced in an online virtual reality environment. Pharmacol. Biochem. Behav. 96, 454–460. https://doi.org/10.1016/j.pbb.2010.07.005 (2010).
Sinha, R. & O’Malley, S. S. Craving for alcohol: findings from the clinic and the laboratory. Alcohol Alcohol. (Oxford, Oxfordshire) 34, 223–230 (1999).
Tung, C. K., Yeung, S. W., Chiang, T. P., Xu, K. & Lam, M. Reliability and validity of the Severity of Dependence Scale in a Chinese sample of treatment-seeking ketamine users. East Asian Arch. Psychiatry 24, 156–164 (2014).
Fernández-Calderón, F., Vidal-Giné, C., López-Guerrero, J. & Lozano-Rojas, Ó. M. Reliability, convergent and structural validity and cut-off score of the Severity of Dependence Scale for recreational ketamine users. Addict. Behav. 60, 1–7. https://doi.org/10.1016/j.addbeh.2016.03.016 (2016).
Buysse, D. J. et al. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep 14, 331–338 (1991).
Tzeng, J. I., Fu, Y. W. & Lin, C. C. Validity and reliability of the Taiwanese version of the Pittsburgh Sleep Quality Index in cancer patients. Int. J. Nurs. Stud. 49, 102–108. https://doi.org/10.1016/j.ijnurstu.2011.08.004 (2012).
MacKinnon, D. P., Fairchild, A. J. & Fritz, M. S. Mediation analysis. Annu. Rev. Psychol. 58, 593. https://doi.org/10.1146/annurev.psych.58.110405.085542 (2007).
Holm, S. A simple sequentially rejective multiple test procedure. Scand. J. Stat. 6, 65–70 (1979).
Brower, K. J. & Perron, B. E. Sleep disturbance as a universal risk factor for relapse in addictions to psychoactive substances. Med. Hypotheses 74, 928–933. https://doi.org/10.1016/j.mehy.2009.10.020 (2010).
Nettleton, S., Meadows, R. & Neale, J. Disturbing sleep and sleepfulness during recovery from substance dependence in residential rehabilitation settings. Sociol. Health Illn. 39, 784–798. https://doi.org/10.1111/1467-9566.12528 (2017).
Brower, K. J., Krentzman, A. & Robinson, E. A. Persistent insomnia, abstinence, and moderate drinking in alcohol-dependent individuals. Am. J. Addict. 20, 435–440. https://doi.org/10.1111/j.1521-0391.2011.00152.x (2011).
Conroy, D. A. & Arnedt, J. T. Sleep and substance use disorders: an update. Curr. Psychiatry Rep. 16, 487. https://doi.org/10.1007/s11920-014-0487-3 (2014).
Haario, P., Rahkonen, O., Laaksonen, M., Lahelma, E. & Lallukka, T. Bidirectional associations between insomnia symptoms and unhealthy behaviours. J. Sleep Res. 22, 89–95. https://doi.org/10.1111/j.1365-2869.2012.01043.x (2013).
Serre, F., Fatseas, M., Swendsen, J. & Auriacombe, M. Are sleep disturbances associated with craving intensity? What is the influence of psychiatric comorbidity and type of substance on this relationship? A computerized ambulatory monitoring study in patients beginning treatment for addiction. Drug Alcohol Depend. 100, e94 (2015).
Valentino, R. J. & Volkow, N. D. Drugs, sleep, and the addicted brain. Neuropsychopharmacology 45, 3–5. https://doi.org/10.1038/s41386-019-0465-x (2020).
Pannucci, C. J. & Wilkins, E. G. Identifying and avoiding bias in research. Plast. Reconstr. Surg. 126, 619–625. https://doi.org/10.1097/PRS.0b013e3181de24bc (2010).
Keeble, C., Law, G. R., Barber, S. & Baxter, P. D. Choosing a method to reduce selection bias: a tool for researchers. Open J. Epidemiol. 05, 155–162. https://doi.org/10.4236/ojepi.2015.53020 (2015).
Lee, J. W., Brown, E. S., Perantie, D. C. & Bobadilla, L. A comparison of single-item visual analog scales with a multiitem Likert-type scale for assessment of cocaine craving in persons with bipolar disorder. Addict. Disord. Treat. 1, 140–142 (2002).
Hennessy, S., Bilker, W. B., Berlin, J. A. & Strom, B. L. Factors influencing the optimal control-to-case ratio in matched case-control studies. Am. J. Epidemiol. 149, 195–197 (1999).
Funding
This study was supported by Grants KMUH104-4T05, KMUH107-7R68, and KMUH108-8R63.
Author information
Authors and Affiliations
Contributions
P.-W. wrote the text, H.-C.L. and H.-C.W. collected data, C.-Y.H. designed the study, C.-H.K. analyzed the data, and C.-F.Y. designed the study and collected data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yen, CF., Lin, HC., Ko, CH. et al. Sleep quality among individuals with ketamine use and the mediating role of craving. Sci Rep 10, 20535 (2020). https://doi.org/10.1038/s41598-020-77631-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-77631-9
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.