Abstract
The early and definitive diagnosis of malignant bile duct stenoses is essential for a timely and adequate therapy. However, tissue sampling with transpapillary brush cytology (BC) or forceps biopsy (FB) remains challenging. With this study, we aimed to compare the effectiveness and safety of different tissue sampling modalities (BC, FB without/after previous balloon dilatation). Standardized database research identified all patients, who underwent endoscopic retrograde cholangiography with BC and/or FB for indeterminate bile duct stenosis between January 2010 and April 2018 and with a definitive diagnosis. 218 patients were enrolled (149 cases with malignant and 69 with benign disease). FB had a significant higher sensitivity than BC (43% vs. 16%, p < 0.01). Prior balloon dilatation of the stenosis improved the sensitivity of FB from 41 to 71% (p = 0.03), the NPV from 36 to 81% (p < 0.01) and the accuracy from 55 to 87% (p < 0.01). The complication rates did not differ significantly between the modalities. In our center FB turned out to be the diagnostically more effective procedure. Balloon dilatation of the stenosis before FB had a significant diagnostic benefit and was not associated with a higher complication rate.
Similar content being viewed by others
Introduction
Biliary strictures are frequently caused by malignant tumors of the intra- or extrahepatic biliary tree, the gallbladder, the liver, the pancreas or the surrounding lymph nodes or by metastasis in these organs. However, benign conditions like autoimmune or infectious diseases or posttraumatic ischemias can also induce inflammation and scarring fibrosis, that mimic a malignant stricture. Unless the underlying history and the typical localization and configuration of the stricture unambiguously indicate a benign etiology, we speak of an indeterminate biliary stricture (IBiS), which is highly suspicious for malignancy but lacks a confirmative tissue diagnosis1. This is often the case in patients with primary sclerosing cholangitis (PSC), who develop fibrotic bile duct strictures but have a risk of 1.4% per year2 and a life-time risk of up to 14%3 to develop hepatobiliary malignancies, and in patients with chronic pancreatitis, who frequently develop strictures due to inflammation of the pancreatic head but also have an increased risk of pancreatic cancer (PCA)4.
The early and definitive exclusion or securing of malignancy of bile duct strictures is essential in order to avoid overtreatment (e.g. non-indicated surgical interventions or non-indicated chemotherapies) on the one hand, but on the other hand to allow for a curative resection or at least an immediate start of a palliative chemotherapy.
Current guidelines5,6 emphasize the importance of additional imaging like endoscopic ultrasound (EUS), computed tomography (CT) or magnetic resonance imaging (MRI) for the characterization and, if necessary and possible, targeted biopsy of a stricture-related mass. Furthermore, a potential benefit of additional endoscopic tools like cholangioscopy, intraductal ultrasound or laser endomicroscopy is discussed. Despite these methods, however, it is still the primary goal to obtain enough tissue for histological or cytological diagnosis. Since endoscopic retrograde cholangiography (ERC) is indicated under most circumstances, transductal brush cytology (BC) and transpapillary forceps biopsy (FB) are the methods of choice for tissue sampling but both with limited overall sensitivity. In the present study we aimed to identify the best diagnostic strategy considering relevant co-variates (type of forceps, localization of stricture, previous intervention) and complications.
Methods
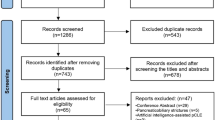
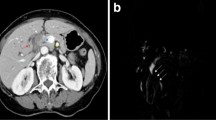
Through a structured database query of our endoscopy documentation system (Viewpoint 5, GE Healthcare) we identified all patients, who were first diagnosed with a biliary stricture suspicious for malignancy between January 2010 and April 2018 and underwent ERC with BC and/or FB at the University Hospital Bonn (Fig. 1). Strictures were considered suspicious for malignancy based on patient’s history and symptoms (e.g. painless jaundice, history of PSC, no previous surgery/trauma) and/or cholangiographic features including an irregular margin, asymmetric or abrupt narrowing and the double-duct sign (see Fig. 2A).
Biliary strictures and different modalities for tissue sampling. (A) Dominant stricture of the left intrahepatic duct in a patient with advanced primary sclerosing cholangitis. (B) Acquisition of a brush cytology of a hilar stricture. (C) Small diameter forceps biopsy of a hilar stricture. (D–F) Cholangiography revealed a highly suspicious stricture of the proximal common bile duct in a patient undergoing endoscopic retrograde cholangiography due to obstructive jaundice. After a guide-wire had been passed over the stricture (D), balloon dilatation of the stricture was performed (E). Subsequently, multiple specimens were obtained using a large diameter forceps (F). Histopathologic examination exposed the stricture to be caused by a cholangiocarcinoma.
Choice and order of the diagnostic tools (BC and/or FB) depended on the assessment and preference of the respective endoscopist. For BC we used a 6 Fr cytology brush (Cook Medical Fusion Cytology Brush, length 25 mm, Fig. 2B). For FB, two different forceps types were used: Larger forcepses (Endo-Flex Biopsy Forceps, outer diameter 2.3 mm, oval cups and spike) were preferably used for strictures of the common bile duct (CBD) or the hilar region and were positioned free-handed under fluoroscopic control (Fig. 2F). For strictures of the intrahepatic ducts, usually smaller forcepses (MTW Biopsy Forceps, outer diameter 1.8 mm, oval spoon-shaped mouth without spike) were advanced through a 10 Fr pushing catheter (Endo-Flex Pusher, Fig. 2C) as described previously7. Strictures were frequently dilated with a balloon (Cook Medical Fusion Titan Biliary Dilation Balloon, 4–10 mm) before or after taking 1–3 biopsies (Fig. 2D–F). In most cases, biliary stents (Boston Scientific Flexima endoprostheses, 7–11.5 Fr; Endo-Flex double-pigtail stents, 7 or 10 Fr) were placed to secure bile flow.
We retrospectively recorded patient characteristics (i.e. age, gender, pre-existing diseases, prior surgery involving the hepatobiliary tract, previously diagnosed malignoma), ERC procedure details (i.e. modalities for tissue sampling including chronological order, previous dilatation, sphincterotomy or stenting, duration of ERC), stricture characteristics (localization, length, extent), ERC-induced complications (pancreatitis, cholangitis, hemorrhage with requirement of blood transfusions, perforation) and pre-interventional CA 19-9 levels.
Final diagnosis of malignancy was based on (a) cytologic and/or histologic evidence obtained by tissue sampling during ERC, endoscopic or percutaneous fine needle biopsy (FNB), surgery or autopsy; or (b) clinical course during a follow-up of at least six months. Definitely malignant and severely suspicious cyto-/histopathological findings were classified as positive. Nearly all tissue samples acquired via BC or FB were examined by two of our local pathologists with appropriate expertise. In cases when BC and FB were conducted during the same ERC, tissue samples from both modalities were examined by the same pathologists. A stricture was considered benign when there was no evidence for malignancy during a follow-up of at least 6 months (i.e. absence of radiomorphologic tumor progression including infiltration and/or metastatic dissemination). Unless otherwise specified, the following analyses are based on each patient’s first ERC in domo that fulfills the above mentioned inclusion criteria. The study was performed in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of the Medical Faculty of the University of Bonn (approval number 233/17). Written informed consent for ERC including tissue sampling and stricture dilatation was obtained from all patients.
Statistical analysis
Categorical variables are expressed as numbers with percentages in parenthesis. Continuous data are presented as mean ± standard deviation. Statistical comparison of proportions was performed using Chi2 test (with Yates correction) and two-tailed Fisher’s exact test, respectively. Unpaired t test with Welch’s correction was used to compare means of continuous variables. A p-value less than 0.05 was considered statistically significant. Statistical analyses were performed with IBM SPSS 25.
Results
Patients’ characteristics and final diagnosis
Endoscopic database research yielded a total of 247 patients with IBiS, who underwent ERC from January 2010 to April 2018 and received further sampling with BC and/or FB (Fig. 1). No definitive diagnosis could be obtained in 29 cases due to an insufficient follow-up, i.e. less than 6 months (for death or other reasons). Therefore, 218 patients (Table 1) remained for the final statistical analysis.
Malignant disease was finally diagnosed in 149 patients. Final malignant diagnosis based on (a) cytological and/or histological evidence obtained by surgery/autopsy (n = 81), percutaneous tissue sampling (n = 18), EUS-FNA (n = 2), tissue sampling via BC/FB (n = 38) and (b) the clinical course during a follow-up of 6 months (n = 10, mean follow-up for this cohort: 12.59 ± 7.10 months). Cases with confirmation of malignancy by multiple diagnostic modalities were subsumed under the first mentioned method. Benign condition was finally diagnosed in 69 patients by (a) surgery (n = 24) and (b) the clinical course during a follow-up of at least 6 months (n = 45, mean follow-up for this cohort: 27.15 ± 18.10 months).
The underlying diseases are summarized in Table 2. Malign stricture was caused by cholangiocarcinoma (CCA) in 89 cases (59.73%) and by PCA in 38 cases (25.50%). PSC was the most frequent cause of benign stricture with 50.72% (35/69 cases). 40/218 patients (18.35%) fulfilled inclusion criteria for the study due to PSC with dominant stricture (Fig. 2A). In 5 of these cases (12.50%), dominant stricture was caused by a cholangiocarcinoma. 70/218 patients (32.11%), 44 patients with benign and 26 patients with malignant stricture, underwent more than one ERC during the evaluation period (Fig. 3).
Follow-up ERCs. 70 patients received more than one endoscopic retrograde cholangiography (ERC). Patient drop out (as noted on the sides) was due to the clinical course of malignant disease, intercurrent confirmation of stricture dignity through other modalities or a loss of follow-up. There was only one patient with malignant disease among the 15 patients undergoing more than four ERCs. The denoted sensitivities, negative predictive values (NPV) and accuracies of the ERCs were calculated considering the results of both, brush cytologies and forceps biopsies. Since there were no false-positive diagnoses, specificity and positive predictive values reached 100%.
Overall diagnostic performance of BC and FB
Altogether 83 brush cytologies and 188 forceps biopsies were obtained during the first ERC with tissue sampling in 218 patients. Sufficient sample material for pathological examination was acquired in 85.54% (71/83 BC) and 97.87% (184/188 FB). Definitely malignant or highly suspicious pathological findings were acquired with BC in 7 of 44 (15.91%) and with FB in 56 of 129 (43.41%) patients with malignant disease (p < 0.01, Fig. 4). Corresponding negative predictive values (NPV) and accuracies were 42.19% and 47.89% for BC and 42.97% (p = 0.92) and 60.33% (p = 0.07) for FB. Specificity and positive predictive values reached 100% for both modalities (no false-positive diagnoses). BC and FB showed higher sensitivities for CCA compared to PCA (CCA: BC: 23.08%, FB: 51.90%, PCA: BC: 10%, FB: 32.35%, CCA vs. PCA: BC: p = 0.65, FB: p = 0.06). The localization of CCA had no significant influence on the sensitivity of FB (distal CCA: 60%, perihilar CCA: 46.15%, intrahepatic CCA: 71.43%, p > 0.05). Due to a low case count in the subgroups, analyses of the sensitivity of BC depending on localization of CCA were not reliable.
Diagnostic performance of BC and FB. The bar chart opposes the sensitivities (Sens), the negative predictive values (NPV) and the accuracies (Acc) of the respective modalities in percentages (rounded to the nearest whole number). Appendant specificities and positive predictive values were not depicted in this chart, as they were 100% consistently. FB forceps biopsy, BC brush cytology, *p < 0.05, **p < 0.01.
Influence of stricture dilatation on the diagnostic performance of forceps biopsy
Balloon dilatation of the stricture was performed in 49/218 cases (22.48%). FB was performed after prior balloon dilatation in 31 cases and without prior dilatation in 158 cases (Fig. 4). Stricture dilatation to 6–10 mm (depending on the diameter of the bile duct) prior to FB provided a significant diagnostic advantage: Without prior dilatation, FB yielded a sensitivity of 40.52%, an NPV of 35.51% and an accuracy of 55.19% (Fig. 4). After stricture dilatation, sensitivity, NPV and accuracy significantly increased to 71.43% (p = 0.03), 80.95% (p < 0.01) and 87.10% (p < 0.01). In none of the analyzed procedures, balloon dilatation of the stricture was performed prior to BC. Performance of stricture dilatation had a significant influence on the duration of ERC (mean duration of ERC without dilatation: 57.17 ± 24.92 min, mean duration of ERC with dilatation: 69.18 ± 37.37 min, p = 0.04).
Other potential confounding factors
Stricture localization, extent and length
Stricture localization and the respective diagnostic approach are summarized in Table 3. 92.02% (173/188) of the strictures were high-grade with a narrowing > 90%, whereas 7.98% (15/188) of the strictures showed a minor narrowing < 90%. The mean stricture length was 22.45 ± 10.79 mm. Stricture length did not correlate with presence of malignancy (point-biserial correlation coefficient rpb = 0.03). Neither stricture localization nor extent nor length (strictures shorter vs. longer than mean length) significantly influenced the sensitivity of BC or FB.
Forceps types
Large diameter forceps and small diameter forceps were used in 79.86% (111/139) and 25.18% (35/139) of the cases (when FB was conducted and forceps type known), respectively (Table 3). Sufficient sample material for pathological examination was acquired in 99.10% (110/111) and 100% (35/35) of the cases using large and small diameter forceps, respectively. Their diagnostic performance did not differ significantly.
Effect of prior EST and prior biliary stenting
119 of 211 (56.40%) patients underwent ERC with endoscopic sphincterotomy (EST) prior to the evaluation period or prior to meeting the inclusion requirements for this study. Prior biliary stenting was done in 71 of 218 (32.57%) patients. Neither prior EST nor prior stenting altered sensitivity of BC or FB significantly.
Implications of pre-interventional CA 19-9 levels on the diagnostic performance of brush cytology and forceps biopsy
Pre-interventional CA 19-9 levels of patients with malignant disease (4218.72 ± 11,828.27 U/ml) were significantly higher than in patients with benign condition (92.95 ± 365.98 U/ml, p < 0.05; see Table 1). ROC analysis provided a suitable cut-off value of 80 U/ml with a remarkable capacity to predict benign and malignant condition (AUC: 0.85 ± 0.04, sensitivity: 73.91%, specificity: 85.71%, PPV: 93.15%, NPV 55.56%, accuracy 77.17%). When the cut-off value was exceeded, NPV and accuracy of BC and FB decreased significantly (BC: sensitivity: 0% vs. 14.29%, p > 0.05, NPV: 65% vs. 5.26%, p < 0.01, accuracy: 65% vs. 18.18%, p < 0.01; FB: sensitivity: 38.10% vs. 44.07%, p > 0.05, NPV: 64.86% vs. 13.16%, p < 0.01, accuracy: 71.11% vs. 48.44%, p < 0.05; each comparison for CA 19-9 lower vs. higher than 80 U/ml).
Adverse events
ERC-induced pancreatitis or cholangitis was observed after 14 of 242 (5.79%) and 3 of 244 (1.23%) ERCs, respectively (Table 4). ERC-induced perforation of the bile duct, severe post-interventional situations (hemorrhage requiring transfusions; requirement of intensive care or surgery) or death did not occur in any case. Stricture dignity, applied modality or stricture dilatation showed no correlation with the incidence of adverse events.
Discussion
In suspected malignant biliary strictures tissue acquisition is usually required, since in most cases imaging alone with CT, MRI or EUS does not lead to a definitive diagnosis, which is albeit essential for initiating an appropriate therapy8,9. Furthermore, obtaining a histology in case of biliary malignancy is becoming increasingly important to assess the presence of predictive markers in order to offer a personalized chemotherapy, such as IDH1 with recently presented positive phase III data in the 2nd line therapy10,11.
Endoscopic or percutaneous fine needle biopsy is a viable option in case of a visible mass or bile duct wall thickening12,13,14; but most patients with IBiS suffer from cholestasis or even septic cholangitis and require biliary drainage preferably through ERC. In this situation according to current recommendations4,6 transpapillary BC or FB is the primary method to obtain tissue for a cytological or histological diagnosis. While the specificity of both methods is excellent, sensitivity and NPV are limited.
In the present study we analyzed retrospectively a cohort of 218 patients, who underwent ERC with BC and/or FB due to a suspected malignant biliary stricture between January 2010 and April 2018, in order to identify parameters that may impact the sensitivity and NPV of tissue sampling. In a metaanalysis from 2015 (including 9 studies and 730 patients) Navaneethan et al.15 reported comparable pooled sensitivities of BC and FB in diagnosing malignant biliary strictures of 45% and 48.1%. Our data confirm this observation in a large and representative real-life cohort with a higher sensitivity of FB (43.4%) compared to BC (15.9%) while the specificity was 100% for both methods. Not surprisingly, we also found higher sensitivities for CCA (BC: 23.08%, FB: 51.90%) than for PCA (BC: 10%, FB: 32.35%). This difference might be explained by the fact that for technical reasons the brush detaches the cell material rather superficially, while the forceps penetrates deeper into the targeted tissue. In many cases with submucosal tumor growth or marked desmoplastic fibrosis and especially in case of an extraluminal tumor like PCA, the cell material obtained by BC might be suboptimal. It should be noted, however, that the significant difference between BC and FB in our cohort was primarily due to the comparatively poor sensitivity of BC, while FB had a sensitivity that was comparable with previously reported ones15. This might be partly explained by the fact that we did not routinely use advanced cytologic techniques, such as digital image analysis and fluorescence in situ hybridization, which improve the sensitivity of BC for diagnosing malignancy in IBiS16,17,18. Moreover, we obtained adequate material for cytological examination in only 85.54% with brushing, which might be due to the relative high percentage of very fibrotic PSC related strictures. Other centers, however, reported excellent results of ERC with BC in screening for PSC related biliary malignancy19. Furthermore, we have used BC much less frequently, so that a certain selection bias cannot be excluded. It is therefore questionable whether our results should generally lead to the conclusion that FB is superior to BC. Rather, local cytopathological expertise as well as anatomical and technical conditions should also be considered. In order to optimize the cellular yield and thereby increase its sensitivity, some technical improvements of the brush have also been presented in the meantime20,21.
Given the limited sensitivity of BC and FB and in order to avoid false negative results, it is recommended either to use an alternative method like EUS-FNB for tissue sampling5,6 or to repeat the ERC with FB/BC (supplemented if necessary with advanced imaging techniques like cholangioscopy or intraductal ultrasound). Our findings support the latter recommendation: Taking into account an inevitable patient drop-out due to the clinical course of malignant disease, confirmation of stricture dignity through other modalities or a loss of follow-up, repetition of tissue sampling via ERC led to satisfying NPVs (with the 4th ERC yielding an NPV of 88.89%, see Fig. 3). As we could show, pre-interventional CA 19-9 levels proved to be a valuable tool in order to assess the reliability of negative cytological/histological findings of BC or FB. The NPV of BC and FB decreased significantly when a cut-off value of 80 U/ml was exceeded. Negative cytological/histological findings of BC or FB despite exceedance of the CA 19-9 cut-off value of 80 U/ml should encourage to repeat tissue sampling.
When we retrospectively analyzed a potential impact of other confounding co-variates, we found no significant impact of prior EST or prior biliary stenting on the sensitivity of BC or FB. In contrast to others22,23,24 we could also not confirm a significant impact of stricture length, stricture localization or stricture extent on the sensitivity of transpapillary tissue sampling. Also, sensitivity of FB did not differ between a large or small diameter forceps and the sample yield was excellent with both types. Nevertheless, according to previous publications modification of forceps type25,26 might even improve sensitivity or make it easier to insert the forceps into the bile duct and to reach the stricture. The most relevant finding in our study is probably the significantly better sensitivity and NPV of FB following prior balloon dilation (which was primarily indicated in order to secure bile flow and to allow the implantation of a biliary stent). In our study, we performed FB after balloon dilatation in 31 cases and without prior dilatation in 158 cases (Fig. 4). This somewhat more aggressive approach increased the duration of ERC (57.17 ± 24.92 min vs. 69.18 ± 37.37 min, p = 0.04) but was not associated with an increased complication rate such as perforation, bleeding or pancreatitis (Table 4). However, the sensitivity [71.43% vs. 40.52% (p = 0.03)], the NPV [80.95% vs. 35.51% (p < 0.01)] and the accuracy [87.10% vs. 55.19% (p < 0.01)] were significantly higher for FB with prior balloon dilatation compared to FB without prior dilatation (Fig. 4). A potential selection bias cannot be excluded since balloon dilatation of the stricture was performed in only 49/218 cases (22.48%) and more likely in narrow strictures with relevant impairment of the bile flow. However as noted above, stricture extent did not have a significant influence on the diagnostic performance of FB in our study. Cholangiocarcinoma, the most common cause of IBiS in our study, often shows a periductal-infiltrating growth pattern with a dense desmoplastic fibrous stroma27. We speculate that balloon dilation tears the superficial desmoplastic and fibrous tissue so that the forceps can reach better and more effectively the submucosal tumor parts. Two previous studies analyzed the impact of stricture dilatation on the diagnostic yield: The first study28 on 46 patients reported that a combination of stricture dilation, endoscopic needle aspiration, and biliary brushing significantly improved the diagnostic yield for IBiS; the second study29 (139 patients) could not confirm a better sensitivity of BC after dilatation. In the present study we did not perform a balloon dilatation prior BC, because we expected that it is more difficult for the bristles of the brush to scrape cellular material from a stenosis that is then no longer narrowed. Therefore, in contrast to both previous studies, our study is the first which analyzes the effect of prior balloon dilatation on the sensitivity of forceps biopsy.
In conclusion, FB turned out to be the more effective method for transpapillary tissue sampling in our center. Balloon dilatation of the stenosis before FB provided a significant diagnostic benefit and was not associated with more complications. When both, tissue sampling and stricture dilatation, are indicated, we therefore recommend to dilate first and to take the FB afterwards. In order to validate our findings, we would advocate a prospective case control study. For this study design, the recruitment of patients will certainly take several years and could be accelerated by a contribution of multiple centers to the study.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Novikov, A., Kowalski, T. E. & Loren, D. E. Practical management of indeterminate biliary strictures. Gastrointest. Endosc. Clin. N. Am. 29, 205–214. https://doi.org/10.1016/j.giec.2018.12.003 (2019).
Weismüller, T. J. et al. Patient age, sex, and inflammatory bowel disease phenotype associate with course of primary sclerosing cholangitis. Gastroenterology 152, 1975-1984.e8. https://doi.org/10.1053/j.gastro.2017.02.038 (2017).
Tischendorf, J. J. W., Hecker, H., Krüger, M., Manns, M. P. & Meier, P. N. Characterization, outcome, and prognosis in 273 patients with primary sclerosing cholangitis: a single center study. Am. J. Gastroenterol. 102, 107–114. https://doi.org/10.1111/j.1572-0241.2006.00872.x (2007).
Kempeneers, M. A. et al. International consensus guidelines for surgery and the timing of intervention in chronic pancreatitis. Pancreatology 20, 149–157. https://doi.org/10.1016/j.pan.2019.12.005 (2020).
Nakai, Y. et al. International consensus statements for endoscopic management of distal biliary stricture. J. Gastroenterol. Hepatol. 35, 967–979. https://doi.org/10.1111/jgh.14955 (2020).
Sun, B. et al. Review article: Asia-pacific consensus recommendations on endoscopic tissue acquisition for biliary strictures. Aliment Pharmacol. Ther. 48, 138–151. https://doi.org/10.1111/apt.14811 (2018).
Kulaksiz, H. et al. A novel method of forceps biopsy improves the diagnosis of proximal biliary malignancies. Dig. Dis. Sci. 56, 596–601. https://doi.org/10.1007/s10620-010-1535-4 (2011).
Heinzow, H. S. et al. Comparative analysis of ERCP, IDUS, EUS and CT in predicting malignant bile duct strictures. World J. Gastroenterol. 20, 10495–10503. https://doi.org/10.3748/wjg.v20.i30.10495 (2014).
Rösch, T. et al. A prospective comparison of the diagnostic accuracy of ERCP, MRCP, CT, and EUS in biliary strictures. Gastrointest. Endosc. 55, 870–876. https://doi.org/10.1067/mge.2002.124206 (2002).
Lowery, M. A. et al. Safety and activity of ivosidenib in patients with IDH1-mutant advanced cholangiocarcinoma: a phase 1 study. Lancet Gastroenterol. Hepatol. 4, 711–720. https://doi.org/10.1016/S2468-1253(19)30189-X (2019).
Abou-Alfa, G. K. et al. ClarIDHy: a global, phase III, randomized, double-blind study of ivosidenib (IVO) vs placebo in patients with advanced cholangiocarcinoma (CC) with an isocitrate dehydrogenase 1 (IDH1) mutation. Ann. Oncol. 30, v872–v873. https://doi.org/10.1093/annonc/mdz394.027 (2019).
Garrow, D. et al. Endoscopic ultrasound: a meta-analysis of test performance in suspected biliary obstruction. Clin. Gastroenterol. Hepatol. 5, 616–623. https://doi.org/10.1016/j.cgh.2007.02.027 (2007).
Lee, J. H., Salem, R., Aslanian, H., Chacho, M. & Topazian, M. Endoscopic ultrasound and fine-needle aspiration of unexplained bile duct strictures. Am. J. Gastroenterol. 99, 1069–1073. https://doi.org/10.1111/j.1572-0241.2004.30223.x (2004).
Mohamadnejad, M. et al. Role of EUS for preoperative evaluation of cholangiocarcinoma: a large single-center experience. Gastrointest. Endosc. 73, 71–78. https://doi.org/10.1016/j.gie.2010.08.050 (2011).
Navaneethan, U. et al. Comparative effectiveness of biliary brush cytology and intraductal biopsy for detection of malignant biliary strictures: a systematic review and meta-analysis. Gastrointest. Endosc. 81, 168–176. https://doi.org/10.1016/j.gie.2014.09.017 (2015).
Barr Fritcher, E. G. et al. An optimized set of fluorescence in situ hybridization probes for detection of pancreatobiliary tract cancer in cytology brush samples. Gastroenterology 149, 1813-1824.e1. https://doi.org/10.1053/j.gastro.2015.08.046 (2015).
Levy, M. J. et al. Prospective evaluation of advanced molecular markers and imaging techniques in patients with indeterminate bile duct strictures. Am. J. Gastroenterol. 103, 1263–1273. https://doi.org/10.1111/j.1572-0241.2007.01776.x (2008).
Smoczynski, M. et al. Routine brush cytology and fluorescence in situ hybridization for assessment of pancreatobiliary strictures. Gastrointest. Endosc. 75, 65–73. https://doi.org/10.1016/j.gie.2011.08.040 (2012).
Boyd, S. et al. Screening primary sclerosing cholangitis and biliary dysplasia with endoscopic retrograde cholangiography and brush cytology: risk factors for biliary neoplasia. Endoscopy 48, 432–439. https://doi.org/10.1055/s-0041-110792 (2016).
Fogel, E. L. et al. Effectiveness of a new long cytology brush in the evaluation of malignant biliary obstruction: a prospective study. Gastrointest. Endosc. 63, 71–77. https://doi.org/10.1016/j.gie.2005.08.039 (2006).
Shieh, F. K. et al. Improved endoscopic retrograde cholangiopancreatography brush increases diagnostic yield of malignant biliary strictures. World J. Gastrointest. Endosc. 6, 312–317. https://doi.org/10.4253/wjge.v6.i7.312 (2014).
Naitoh, I. et al. Predictive factors for positive diagnosis of malignant biliary strictures by transpapillary brush cytology and forceps biopsy. J. Dig. Dis. 17, 44–51. https://doi.org/10.1111/1751-2980.12311 (2016).
Nishikawa, T. et al. Factors affecting the accuracy of endoscopic transpapillary sampling methods for bile duct cancer. Dig. Endosc. 26, 276–281. https://doi.org/10.1111/den.12140 (2014).
Park, J. G. et al. Percutaneous transluminal forceps biopsy in patients suspected of having malignant biliary obstruction: factors influencing the outcomes of 271 patients. Eur. Radiol. 27, 4291–4297. https://doi.org/10.1007/s00330-017-4796-x (2017).
Tamada, K. et al. Ropeway-type bile duct biopsy forceps with a side slit for a guidewire. Gastrointest. Endosc. 53, 89–92. https://doi.org/10.1067/mge.2001.112094 (2001).
Yamamoto, K. et al. Evaluation of novel slim biopsy forceps for diagnosis of biliary strictures: Single-institutional study of consecutive 360 cases (with video). World J. Gastroenterol. 23, 6429–6436. https://doi.org/10.3748/wjg.v23.i35.6429 (2017).
Rizvi, S. & Gores, G. J. Current diagnostic and management options in perihilar cholangiocarcinoma. Digestion 89, 216–224. https://doi.org/10.1159/000360791 (2014).
Farrell, R. J. et al. The combination of stricture dilation, endoscopic needle aspiration, and biliary brushings significantly improves diagnostic yield from malignant bile duct strictures. Gastrointest. Endosc. 54, 587–594. https://doi.org/10.1067/mge.2001.118715 (2001).
de Bellis, M. et al. Influence of stricture dilation and repeat brushing on the cancer detection rate of brush cytology in the evaluation of malignant biliary obstruction. Gastrointest. Endosc.. 58, 176–182. https://doi.org/10.1067/mge.2003.345 (2003).
Acknowledgements
Interim results of this study were presented at the 73rd annual conference of the German Society of Gastroenterology (DGVS) in 2018 and the 49th congress of the German Society of Endoscopy (DGE-BV) in 2019. The present study is part of the MD thesis of D. Pörner.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
D.P. and T.J.W. designed and initiated the study, enrolled patients, performed the statistical analysis, analyzed the results and wrote and edited the paper. D.J.K., D.H., A.H., R.M., R.H., J.N., C.P.S. and T.J.W. performed the endoscopic interventions. H.M., T.R.G. and S.M. performed the surgical interventions during the clinical follow-up. M.A.G. did the oncological follow-up and treatment. H.P.F. and M.T. performed the histopathological analyses. All authors approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pörner, D., Kaczmarek, D.J., Heling, D. et al. Transpapillary tissue sampling of biliary strictures: balloon dilatation prior to forceps biopsy improves sensitivity and accuracy. Sci Rep 10, 17423 (2020). https://doi.org/10.1038/s41598-020-74451-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-74451-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.