Abstract
To our knowledge, little attention has been paid to the sexual function of health workers. The aim of the present study was to assess the frequency of sexual dysfunction among Chinese doctors. In addition, the risk factors for sexual dysfunction were analyzed. This was a questionnaire-based multicenter cross-sectional survey performed in five large academic medical centers in China. A total of 539 male doctors, 547 female doctors were evaluated. We analyzed doctors' demographic characteristics, quality of life, sexual function and attitudes towards sexual problems. Chinese doctors are at high risk of sexual dysfunction and poor health. The prevalence of sexual dysfunction appears to increase with age, and is associated with various social and demographic factors including monthly income, physical exercise, working hours, night shift and health-related quality. The quality of life and sexual health of doctors deserves special attention as a significant public health concern. Alleviating work pressure, increasing income, improving quality of life and therapeutic sexual problems should be considered comprehensively.
Similar content being viewed by others
Introduction
Sexual functioning is an important part of human lives that relates to mental and physical wellbeing and social relations1,2,3. Sexual problems and dysfunctions are commonly encountered experiences that impact on the quality of life in the general population4,5.
According to numerous studies, sexual dysfunctions are highly prevalent in both sexes, ranging from 10 to 52% of men and 25% to 63% of women6. The large discrepancy in prevalence across studies could be attributed to the differences in the populations, the sampling methods, diagnostic criteria and assessment tools7,8,9. Among men, the most prevalent problems were erectile dysfunction, premature ejaculation, and orgasm problems. Whereas among women, the most frequent were low desire, reduced arousal, difficult to achieve an orgasm, and dyspareunia10,11. The reasons for sexual dysfunction are multiple and complex. In recent years, epidemiological researches have found associations between sexual dysfunction and many personal characteristics, such as age, education level, marital status, household income, mental and physical health problems12. Currently, sexual dysfunction have been studied extensively in different populations, but the sexual function of health workers has received very little attention13,14. In fact, these scanty studies only focused on the risk factors of sexual dysfunction, such as age and related diseases. That is, in these studies, the health worker groups was considered only as readily accessible samples, their sexual function has not been specially analyzed.
In general, doctors are considered to have a higher degree, higher incomes, and better health care than most of their peers. It is noteworthy that these characteristics have also been widely described in association with sexual dysfunction. On the other hand, numerous studies have demonstrated a clear relation between sexual function and quality of life15,16. As a particular occupational population, doctors undertake the mission of curing patients and exposure to disease, death, emergency which is believed to lead to a high level of occupational stress. Additionally, stress from night shift work, overtime, and other occupational characteristics, such as chemical exposure, radiation sources, musculoskeletal strain and disorders can also affect the mental and physical health of doctors17,18,19.
Thus, it is necessary to examine the patterns, demographic and clinical correlates of sexual dysfunction in doctors. Knowledge about doctors’ sexual functioning as well as early detection of sexual problems and dysfunctions is essential to promote a healthy sexual lifestyle which has unintelligible influence on their mental and physical health. And, furthermore, it may has implications for stability in doctors’ workforce and the quality of health cares it provides.
China is a country with a long history of conservative and traditional beliefs, thus the Chinese, even the Chinese doctors, are reluctant to discuss sexual matters openly20. The cultural factors make investigations of sexual function difficult. Actually, there have been no published studies in journals that evaluate the sexual function of Chinese doctors as far as we know. However, with the rapid advancement of internet technique and service, online surveys may provide a helpful solution for this case. China has the most internet users in the world, at 802 million in 2018. The internet service has become an essential open conduit for business, learning and daily communication in this country. Several studies have demonstrated that performance and effectiveness obtained using Internet surveys on sexual problems concur with those obtained using other methods, such as mailing questionnaires or telephone surveys21,22,23. What's more, online surveys may even provide a more relaxed and private environment, while allowing convenient data collection and analysis.
Based on such considerations, this survey was designed to provide the frequency of sexual dysfunction in Chinese doctors and to determine sociodemographic factors associated with clinically problems.
Methods
Participants
This multicenter cross-sectional survey was performed in five large academic medical centers in China from May to July 2019.
By using cluster sampling method, a population consisted initially of 1,396 doctors registered and working in five medical centers. These five centers located in the east, west, south, north, and centre of China respectively, can be considered as representative samples of this country's major public hospital. In considering the feasibility and convenience, a nonprobability sampling method was used in this survey. The final participants came from different department including internal medicine, surgery, pediatrics, obstetrics and gynecology, stomatology.
Informed consent was furnished according to the Declaration of Helsinki and obtained from all subjects after they were provided a detailed description of the experimental procedures and informed that they could withdraw from the survey at any time. All experimental protocol in this study involving human participants was approved by the Ethic Committee of Anhui Medical University and the relevant hospitals. (Approval number: PJ20190707; Clinical trial registration no. ChiCTR1800020321). We organized a multidisciplinary team of health professionals, including health and counselling psychologists, network engineers, venereologists, gynecologists, and reproductive biologists. We are confirming that all experiments were performed in accordance with relevant guidelines and regulations that promote respect for all human subjects and protect their health and rights. All study participants approved an electronic copy of informed consent to indicate their agreement for the clinical data to be used in scientific research and publication. Before the questionnaire was distributed, five graduate students and three professors participated in a pilot study to verify and modify the contents of the questionnaire.
A web page link to our questionnaire was sent to the doctors during breaks (https://www.wjx.cn/jq/83291804.aspx). The questionnaire system avoids duplicate entries by preventing users with the same IP address access to the survey twice. Respondents can able to choose an appropriate time to fill out the questionnaire (not busy or in a private environment). This survey was anonymous and participants' information was strictly confidential. The current questionnaires were self-administered and each subject was paid about $5 for participating in this survey.
A total of 1,396 participants (681 men, 715 women) were invited in this survey and 1,278 doctors (615 men, 663 women) submitted the questionnaire, overall participation rates of 90.3% for men and 92.7% for women. The sample size was based on a pilot survey of 160 doctors done in Hefei, Anhui, China in November, 2018. Based on the assumptions (two-tailed α of 0.05, power of 90.0%), a minimum of 897 participants was needed. In order to enhance the credibility of the answers to the questions on sexual function, subjects who had been sexually active, meaning having sex at least once in the last 6 months were included. Among the 1,278 participants, 192 were excluded for the following reasons: pregnant (n = 36); hormone replace-ment therapy (n = 8); diabetes, heart disease and malignant tumors (n = 75); not meet the sexually active criterion (n = 73). Ultimately, 1,086 valid questionnaires were used in the data analysis.
The survey started with an initial interface explained the purpose of the research, obtained informed consent and reviewed the patients’ answers regarding exclusion criteria. In order to enhance the quality of this research, a missing answer reminder component was appended in the system to avoid data missing and ensure data integrality. In addition, an experienced medical expert was available to help respondents with any survey difficulties on the internet or by telephone.
Each parts of the questionnaire
Section 1: focused on the socioeconomic and demographic status of respondents, such as age, gender, height, weight, marital status, education levels, history of diseases, monthly income, physical exercise status, whether menopause, reproductive history, work hours and night shift work situations, etc. These specific categories under each variable are shown in Table 1.
Section 2: assessed sexual function. Sexual function was evaluated with the Arizona Sexual Experience Scale (ASEX) in this survey. It is an effective, short, easy to use, reliable, non-invasive and unisex instruments to assess sexual functioning24,25,26. The translated version of the ASEX contains 5 items, providing a total score ranging from 5 and 30, items on the ASEX query sexual drive, ease of sexual arousal, penile erection or vaginal lubrication, ability to reach orgasm and satisfaction with orgasm in the past week27. Sexual dysfunction was defined as a total score 19 or more, any item 5 or more, or any three items 4 or more. This scale achieved good internal consistency, excellent test–retest reliability (two weeks, r = 0.80 and 0.89), and good construct validity. The Chinese version of the ASEX has been subsequently validated with different clinical samples, and was concluded that this version has high validity and reliability28,29.
Section 3: assessed quality of life. Health-related quality of life was evaluated with the validated Chinese version of the Short-Form 12. This section has twelve items and is composed of eight domains: physical functioning (PF), role limitations due to physical functioning (RP), bodily pain (BP), general health perceptions (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (MH). In general, the physical component summary (PCS) includes PF, RP, BP, and GH, and mental component summary (MCS) includes VT, SF, RE, and MH. Dimension score is converted into a standard 100 scores, a higher score indicates a better quality of life30,31. In fact, as a short, generic measure of QOL, Short-Form 12 has been proved to have high applicability and reliability for the Chinese samples32,33,34,35.
Section 4: an examination of help-seeking behavior. In this section, two questions were asked: First, do you need professional guidance on sexual function? Second, have you received any medical advice or treatment for sexual problems?
At the end of this questionnaire, participants were invited to provide an e-mail address in order to know the final results of this study, as well as for the possible further observational follow-up study.
Statistical analysis
SPSS for Windows (SPSS 18.0, Chicago, IL, USA) were used for statistical analysis, with a significance level of 5% (double tailed). chi-square tests, Student’s t-test, regression analysis model were used to describe the relationships among the variables under suitable conditions. The database was established using EpiData V3.1 software. Bartlett’s test and Kaiser Meyer Olkin measure were used to evaluate the validity. The reliability were evaluated by Cronbach’s α coefficient. Forward stepwised logistic regression was used to identify risk factors related to with sexual dysfunction.
Results
Ultimately, a total of 539 male doctors, 547 female doctors aged 24 to 61 (37.12 ± 10.3) years old were evaluated.
Table 1 displays the basic demographic characteristics of the population. In this survey, about 19.3% of the participants were unmarried, and 80.7% were married. Only 11.3% of the respondents were 50 or older and more than half (83.6%) of them had a master degree or higher. In addition, nearly 95.7 percent of doctors worked more than 40 h a week, 42.5% of them had monthly incomes above 10,000 yuan (approximately $1,454 in 2019).
Sexual dysfunction in male and female doctors
Table 2 shows the mean scores of sexual drive, sexual arousal, lubrication/erection, orgasm and sexual satisfaction of the subjects. Built on the self-reported, the prevalence of sexual dysfunction was 35.1% in the whole sample, 20.2% in males and 49.73% in females. Female doctors report significantly higher rates of sexual dysfunction than male doctors (χ2 = 103.760, P = 0.001). Specifically, female doctors were more likely to have sexual drive, sexual arousal and orgasm problems than male.
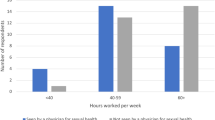
Differences in the incidence of sexual dysfunction between groups were presented in Fig. 1. Compared with doctors aged 21–34 years, the prevalence of sexual dysfunction among doctors aged 50 years or older was higher. In addition, more night shifts, longer working hours, lower monthly income, less physical exercise were strongly associated with increased risk for sexual dysfunction. The prevalence of postmenopausal female subjects was significantly greater than that of premenopausal female subjects. However, there was no significant association between the sexual dysfunction and marital status or education level in this research.
Health-related quality of subjects
Table 3 shows the features of the total and dimension scores of the health-related quality. The mean score of PCS and MCS was 43.2, 41.7 for male and 43.1, 40.3 for female, respectively. It is worth reminding that all these values were significantly lower than the midpoint of the total scales (50), suggesting that the health status of these doctors were poor.
Risk factors of sexual dysfunction
Table 4 shows the demographic and clinical correlates of sexual dysfunction. A forward stepwise multiple regression analysis was used to analyze the impact of variables. After adjusting for confounding variables, we found that age (2.14, P = 0.009), monthly income (OR = 0.45, P = 0.023), physical exercise (OR = 0.57, P = 0.005), working hours (OR = 1.65, P = 0.017), PCS (OR = 0.63, P = 0.001), and MCS (OR = 0.66, P = 0.038) were identified as risk factors of sexual dysfunction in male doctors. In all female, age (OR = 1.079, P = 0.009), night shift (OR = 1.38, P = 0.040), working hours (OR = 2.15, P = 0.026), menopause (OR = 5.05, P = 0.010), PCS (OR = 0.70, P = 0.047), and MCS (OR = 0.43, P = 0.019) were significant predictors of sexual dysfunction.
Reliability and validity analysis
The overall Cronbach’s α coefficient of the profile was 0.810, indicating that the questionnaire had good internal reliability. Exploratory factor analysis showed that KMO measure was 0.836 and Bartlett’s sphericity P value was 0.001, indicating that the data collected from the instrumental were valid for factor analysis.
Help-seeking behavior examination
The help-seeking behavior examination indicated that most of the participants (82.2%) expressed need on the guidance of sexual life. Our data on help-seeking also suggested that only 3.15% of these participants sought medical consultation for their sexual problems.
Discussion
This was a questionnaire-based multicenter cross-sectional survey performed in five large academic medical centers in Nanjing, Hefei, Changchun, Urumqi and Zhanjiang from May to July 2019. Participants were enrolled from these five medical centers through a nonrandom cluster sampling procedure.
Our results show that the prevalence of sexual dysfunction was 49.73% in females doctors. In all ASEX items, female doctors endorsed more frequent sexual dysfunction than male doctors, which is consistent with recent studies36,37. In previous surveys, about 40% of female reports some form of sexual problems38,39, and the prevalence may be even lower in China. For instance, Ma et al. interviewed 586 married women aged 22 to 60 who visited a health clinic and reported a prevalence rate of 37.6% in China40. In another study, a survey showed that 37.9 percent of the young and middle-aged women in Hong Kong had sexual dysfunction41. Similarly, Luo et al. suggested that the incidence of sexual dysfunction in Chinese women was 26.5 percent, less than one-third42. Factors contributing to the diverse rates include various sociocultural backgrounds, sample selection, assessment methods, assessment procedures and different cutoff values. Recently, in a study that used a similar assessment method to ours, 18.4% of Spanish women and 28.7% of Portuguese women were classified as having sexual dysfunction10. In fact, this prevalence appeared to be much lower than that of Chinese female doctors in our study. Despite these demographic and methodological differences, we concluded that Chinese doctors, especially women, are at high risk of sexual dysfunction.
In the current study, the percentage of participants with sexual dysfunction generally increased with age, as showed in Fig. 1. However, the overall prevalence of sexual dysfunction among people aged 35–50 has declined slightly. Among the youngest participants, the high prevalence of sexual dysfunction may reflect the fact that a considerable proportion of young doctors are currently facing serious sexual problems. Several contributing factors may account for this phenomenon. The high incidence of sexual dysfunction among young doctors may be associated with a higher proportion of singles, less sexual experience and a higher rate of sexual partner turnover. On the other hand, tremendous work pressure, economic problems and poor physical and mental health may also play an important role in the high incidence of sexual dysfunction among young doctors in China. The correlation between these factors and sexual dysfunction has been widely reported12,43. Sexual problems are also common among older doctors. As some literatures have reported, they are more likely to suffer from poor lubrication or erectile dysfunction, as well as to lack an interest in sex44,45.
Table 3 shows that the physical and mental health of Chinese doctors in this study are very poor. In recent years, China's huge population base and growing demand for patient health have led to overworking of doctors. The proportion of doctors in the total population in China is 1:735, which is much lower than that in Western countries46. Numerous studies, including our research (Table 1), have reported that Chinese doctors face enormous occupational stress due to their low income, long working hours and poor working environment47,48. It is noteworthy that sexual dysfunction is widely suggested being associated with stress and poor quality of life2. Data from a large British study (NHSLS data) show that emotional and stress-related problems increase the risk of sexual difficulties. It is also suggested that physiological and psychological state are independent factors affecting sexual function49. What's more, another study from Denmark found that poor health is linked to the increasing incidence of sexual dysfunction in both sexes. Physical health problems mainly affect men's sexual life, and mental health problems are closely related to female sexual dysfunction50. Therefore, we believe that a series of effective measures, such as reducing workload and increasing income, may be helpful to reduce work pressure and improve health. We suggest that step up the quality of life of doctors should be considered in the current medical reform, which may be meaningful for improving sexual function among doctors in China.
A number of previous studies consistently reported that only a small proportion of patients with sexual dysfunction may actually seek help, ranging from 6 to 32%. In fact51,52,53, our study showed that the majority (82.2%) of doctors with sexual dysfunction reported that they need professional guidance. Surprisingly, only 12 doctors (3.15%) received any medical advice or treatment at all. That is, despite the relatively high prevalence of sexual dysfunction among sexually active doctors, we observed that few participants seek help for their problems. This may be linked to traditional Chinese beliefs that discussion of sexual issues is intensely private. With the continuous development and progress of society, Chinese are more open to discussing sexual problems. However, they are still reluctant to discuss doctors. These doctors might be unwilling to raise sexual issue with specialist not only because of shyness but also due to many doctors may feel embarrassed when reporting their diseases, especially facing colleagues54. We should note that doctors are always regarded as models of health knowledge and behavior by the whole society. It is of great importance to doctors and other health professionals to be aware of common sexual difficulties in themselves and patients, and manage them.
The current study was based on an online survey that is generally considered less reliable. But notice that despite the increasing openness and diversity of society, Chinese are still reluctant to discuss sexual issues openly. We believe that an anonymous online questionnaire evaluation system may be a more suitable tool which can provides a comfortable and free environment for people to report and discuss their sexual issues.
However, the causal relationship between quality of life and sexual dysfunction has yet to be investigated. As our data were cross-sectional, we can't infer causality in the relationships we show. In other words, among various factors associated with sexual dysfunction, two-way causality is an obvious possibility. Despite these confusions and concerns, many studies have shown that sexual life satisfaction, mood and quality of life were strongly correlated2,43. In addition, recent advances in therapy for sexual dysfunction may have beneficial effects on quality of life. Regardless of these complex situations, to solve these problems, decision-makers should strive to improve the income and working environment of doctors. On the other hand, researchers should focus on identifying the relevant factors and mechanisms of sexual problems as well as developing appropriate therapies.
Participants in this study were restricted to public hospitals in cities, so there may be better working conditions than private or rural clinics. In China, urban doctors were the most likely to have higher education, higher income and better health care than rural doctors. However, most hospitals are public institutions with fewer private clinics in China. Therefore, we initially focus on municipal hospitals, and expect to consider rural clinics in large multi-center research in the future.
In this survey, only sexually active participants (at least once in the last 6 months) were incorporated into the final analysis, so excluded individuals who may not have had sex recently. This manner may limit our conclusions as excluded respondents may have avoided sex due to sexual difficulties. Excluded doctors were more likely to be single and have lower monthly incomes. In addition, we don't have information about the sexual partners or who used drugs that could suppress libido.
We did not consider variability by ethnicity in this analysis. The Han is the majority ethnic group in China. Before formal study, we have found that the proportion of respondents from minority ethnic groups was too low for reliable analysis (1.9%) in our pre-investigation. We currently undertaking a focus study among ethnic minorities to address this question.
That is, prevalence estimates for the studied sexual dysfunctions may not be applicable to the entire physician groups, but they are most likely to be effective for the sexually active majority of Chinese doctors. Despite these limitations, this is the first report on sexual function of doctors in China.
In general, our findings noted that most Chinese doctors reported having sexual dysfunction and a poor quality of life. The prevalence of sexual dysfunction appears to increase with age, and it is associated with various social and demographic factors including monthly income, physical exercise, working hours, night shift and health-related quality.
Considering the professional characteristics and exemplary role of doctors, their risk management of life and sexual health problems deserves special attention from health policy makers as a significant public health concern.
Data availability
The authors declare that all data supporting the findings of this study are available within the article or from the corresponding author upon reasonable request.
References
McCabe, M. P. et al. Incidence and prevalence of sexual dysfunction in women and men: A consensus statement from the fourth international consultation on sexual medicine 2015. J. Sex Med. 13, 144–152 (2016).
Laumann, E. O., Paik, A. & Rosen, R. C. Sexual dysfunction in the United States: Prevalence and predictors. JAMA 281, 537–544 (1999).
Lee, D. M., Nazroo, J., O’Connor, D. B., Blake, M. & Pendleton, N. Sexual health and well-being among older men and women in England: Findings from the English longitudinal study of ageing. Arch. Sex. Behav. 45, 133–144 (2016).
Chang, S. R., Yang, C. F. & Chen, K. H. Relationships between body image, sexual dysfunction, and health-related quality of life among middle-aged women: A cross-sectional study. Maturitas 126, 45–50 (2019).
Flynn, K. E. et al. Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of U.S. Adults. J. Sex Med. 13, 1642–1650 (2016).
Heiman, J. R. Sexual dysfunction: Overview of prevalence, etiological factors, and treatments. J. Sex Res. 39, 73–78 (2002).
Nappi, R. E. et al. Female sexual dysfunction (FSD): Prevalence and impact on quality of life (QoL). Maturitas 94, 87–91 (2016).
McCool, M. E. et al. Prevalence of female sexual dysfunction among premenopausal women: A systematic review and meta-analysis of observational studies. Sex. Med. Rev. 4, 197–212 (2016).
Mercer, C. H. et al. Changes in sexual attitudes and lifestyles in Britain through the life course and over time: findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet 382, 1781–1794 (2013).
Peixoto, M. M. & Nobre, P. Prevalence and sociodemographic predictors of sexual problems in Portugal: A population-based study with women aged 18 to 79 years. J. Sex Marital Ther. 41, 169–180 (2015).
Beutel, M. E., Weidner, W. & Brahler, E. Epidemiology of sexual dysfunction in the male population. Andrologia 38, 115–121 (2006).
Christensen, B. S. et al. Sexual dysfunctions and difficulties in denmark: Prevalence and associated sociodemographic factors. Arch. Sex. Behav. 40, 121–132 (2011).
Bacon, C. G. et al. Sexual function in men older than 50 years of age: Results from the health professionals follow-up study. Ann. Intern. Med. 139, 161–168 (2003).
Welch, G., Weinger, K. & Barry, M. J. Quality-of-life impact of lower urinary tract symptom severity: Results from the Health Professionals Follow-up Study. Urology 59, 245–250 (2002).
Naeinian, M. R., Shaeiri, M. R. & Hosseini, F. S. General health and quality of life in patients with sexual dysfunctions. Urol. J. 8, 127–131 (2011).
McCabe, M. P. Intimacy and quality of life among sexually dysfunctional men and women. J. Sex Marital Ther. 23, 276–290 (1997).
Vijendren, A., Yung, M. & Sanchez, J. Occupational health issues amongst UK doctors: A literature review. Occup. Med. (Lond.) 65, 519–528 (2015).
Yao, Y., Wang, W., Wang, F. & Yao, W. General self-efficacy and the effect of hospital workplace violence on doctors’ stress and job satisfaction in China. Int. J. Occup. Med. Environ. Health 27, 389–399 (2014).
Li, L. et al. Work stress, work motivation and their effects on job satisfaction in community health workers: A cross-sectional survey in China. BMJ Open 4, e004897 (2014).
Colonnello, E. & Jannini, E. A. Impact of Chinese Traditional Culture and Related Social Norms on Current Chinese Sexuality and on the Future of Chinese Sexual Medicine. In Cultural Differences and the Practice of Sexual Medicine: A Guide for Sexual Health Practitioners (eds Rowland, D. L. & Jannini, E. A.) 95–113 (Springer, Cham, 2020).
Song, S. H., Jeon, H., Kim, S. W., Paick, J. S. & Son, H. The prevalence and risk factors of female sexual dysfunction in young korean women: An internet-based survey. J. Sex. Med. 5, 1694–1701 (2008).
Shaeer, O., Shaeer, K. & Shaeer, E. The Global Online Sexuality Survey (GOSS): Female sexual dysfunction among Internet users in the reproductive age group in the Middle East. J. Sex. Med. 9, 411–424 (2012).
Pachankis, J. E. et al. Hidden from health: Structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM Internet Survey. AIDS 29, 1239–1246 (2015).
Vaillancourt-Morel, M. P. et al. Profiles of cyberpornography use and sexual well-being in adults. J. Sex. Med. 14, 78–85 (2017).
Esposito, K. et al. Determinants of female sexual dysfunction in type 2 diabetes. Int. J. Impot. Res. 22, 179–184 (2010).
Basson, R. et al. Dehydroepiandrosterone and cortisol as markers of HPA axis dysregulation in women with low sexual desire. Psychoneuroendocrinology 104, 259–268 (2019).
McGahuey, C. A. et al. The Arizona Sexual Experience Scale (ASEX): Reliability and validity. J. Sex Marital Ther. 26, 25–40 (2000).
Zhu, X. et al. Sexual experiences of chinese patients living with an ostomy. J. Wound Ostomy Continence Nurs. 44, 469–474 (2017).
Hou, C. L. et al. Sexual dysfunction and its impact on quality of life in Chinese patients with schizophrenia treated in primary care. Compr. Psychiatry 65, 116–121 (2016).
Gandek, B. et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. International Quality of Life Assessment. J. Clin. Epidemiol. 51, 1171–1178 (1998).
Johnson, J. A. & Coons, S. J. Comparison of the EQ-5D and SF-12 in an adult US sample. Qual. Life Res. 7, 155–166 (1998).
Lam, C. L., Tse, E. Y. & Gandek, B. Is the standard SF-12 health survey valid and equivalent for a Chinese population?. Qual. Life Res. 14, 539–547 (2005).
Lu, P. & Liang, Y. Health-related quality of life of young chinese civil servants working in local government: Comparison of SF-12 and EQ5D. Appl. Res. Qual. Life 11, 1445–1464 (2016).
Liang, Y. & Cao, R. Is the health status of female victims poorer than males in the post-disaster reconstruction in China: A comparative study of data on male victims in the first survey and double tracking survey data. BMC Womens Health 14, 18 (2014).
Shou, J. et al. Reliability and validity of 12-item Short-Form health survey (SF-12) for the health status of Chinese community elderly population in Xujiahui district of Shanghai. Aging Clin. Exp. Res. 28, 339–346 (2016).
Byerly, M. J., Nakonezny, P. A., Fisher, R., Magouirk, B. & Rush, A. J. An empirical evaluation of the Arizona sexual experience scale and a simple one-item screening test for assessing antipsychotic-related sexual dysfunction in outpatients with schizophrenia and schizoaffective disorder. Schizophr. Res. 81, 311–316 (2006).
Harley, E. W., Boardman, J. & Craig, T. Sexual problems in schizophrenia: prevalence and characteristics. A cross sectional survey. Soc. Psychiatry Psychiatr. Epidemiol. 45, 759–766 (2010).
Moreira, E. D. et al. Sexual problems and help-seeking behaviour in adults in the United Kingdom and continental Europe. BJU Int. 101, 1005–1011 (2008).
Moreira, E. D. Jr. et al. Help-seeking behaviour for sexual problems: the global study of sexual attitudes and behaviors. Int. J. Clin. Pract. 59, 6–16 (2005).
Ma, J., Pan, L., Lei, Y., Zhang, A. & Kan, Y. Prevalence of female sexual dysfunction in urban chinese women based on cutoff scores of the Chinese version of the female sexual function index: A preliminary study. J. Sex. Med. 11, 909–919 (2014).
Zhang, H. & Yip, P. S. Female sexual dysfunction among young and middle-aged women in Hong Kong: Prevalence and risk factors. J. Sex. Med. 9, 2911–2918 (2012).
Luo, H. et al. Elevated free triiodothyronine may lead to female sexual dysfunction in Chinese urban women: A hospital-based survey. Sci. Rep. 7, 1216 (2017).
Rosen, R. C. et al. Quality of life, mood, and sexual function: A path analytic model of treatment effects in men with erectile dysfunction and depressive symptoms. Int. J. Impot. Res. 16, 334–340 (2004).
Gelfand, M. M. Sexuality among older women. J. Women’s Health Gend. Based Med. 9, 15–20 (2000).
Waite, L. J., Iveniuk, J., Laumann, E. O. & McClintock, M. K. Sexuality in older couples: Individual and dyadic characteristics. Arch. Sex. Behav. 46, 605–618 (2017).
Li, J., Yang, W. & Cho, S. I. Gender differences in job strain, effort-reward imbalance, and health functioning among Chinese physicians. Soc Sci Med 62, 1066–1077 (2006).
Wu, H., Zhao, Y., Wang, J. N. & Wang, L. Factors associated with occupational stress among Chinese doctors: A cross-sectional survey. Int. Arch. Occup. Environ. Health 83, 155–164 (2010).
Sun, T. et al. Workplace violence, psychological stress, sleep quality and subjective health in Chinese doctors: A large cross-sectional study. BMJ Open 7, e017182 (2017).
Mitchell, K. R. et al. Sexual function in Britain: Findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Lancet 382, 1817–1829 (2013).
Christensen, B. S. et al. Associations between physical and mental health problems and sexual dysfunctions in sexually active Danes. J Sex Med 8, 1890–1902 (2011).
Ansong, K. S., Lewis, C., Jenkins, P. & Bell, J. Help-seeking decisions among men with impotence. Urology 52, 834–837 (1998).
Nicolosi, A., Moreira, E. D. Jr., Shirai, M., Bin Mohd Tambi, M. I. & Glasser, D. B. Epidemiology of erectile dysfunction in four countries: cross-national study of the prevalence and correlates of erectile dysfunction. Urology 61, 201–206 (2003).
Metz, M. E. & Seifert, M. H. Men’s expectations of physicians in sexual health concerns. J. Sex Marital Ther. 16, 79–88 (1990).
Lin, C. M. & Li, C. Y. Prevalence of cardiovascular risk factors in Taiwanese healthcare workers. Ind. Health 47, 411–418 (2009).
Acknowledgements
We would like to thank all participants. We also thank the researchers from Jilin University, Xingjiang Medical University, Jiangsu Medical University and Guangdong Medical University for their efforts throughout the research project. Also contributing to the study were researchers from the Anhui Medical University, as well as engineers, nurses and doctors. Financial support: This work was supported by the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2019PT310002).
Author information
Authors and Affiliations
Contributions
All authors have contributed significantly in the content of the manuscript. W.L. and G.L. proposed the study and wrote the first draft. S.L., P.L., H.C., Y.Z. acquired data and drafted the figures. G.L. and Y.C. is the guarantor, provided senior oversight for design, analysis and interpretation. All authors contributed to the design and interpretation of the study and to further drafts.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, W., Li, S., Lu, P. et al. Sexual dysfunction and health condition in Chinese doctor: prevalence and risk factors. Sci Rep 10, 15180 (2020). https://doi.org/10.1038/s41598-020-72072-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-72072-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.