Abstract
The Developmental Origins of Health and Disease (DOHaD) framework suggests that early-life experiences affect long-term health outcomes. We tested this hypothesis by estimating the long-run effects of exposure to World War II-related food deprivation during childhood and adolescence on the risk of suffering from hypertension and type 2 diabetes at adulthood for 90,226 women from the French prospective cohort study E3N. We found that the experience of food deprivation during early-life was associated with a higher risk of developing type 2 diabetes (+0.7%, 95% CI: 0.073–1.37%) and hypertension (+2.6%, 95% CI: 0.81–4.45%). Effects were stronger for individuals exposed at younger ages. Exposed individuals also achieved lower levels of education, slept less, and were more frequently smokers than unexposed individuals. These results are compatible with both the latency and the pathway models proposed in the DOHaD framework which theorise the association between early life exposure and adult health through both a direct link and an indirect link where changes in health determinants mediate health outcomes.
Similar content being viewed by others
Introduction
Based on the relationship between experience and the biology and psychology of development, the Life Course Health Development (LCHD) and the Developmental Origins of Health and Disease (DOHaD) framework suggest that risk factors, protective factors, and early-life experiences affect individuals’ long-term health and disease outcomes. Although exposure to particular environments and experiences appear to influence health development at all stages, it has been suggested that exposure to environmental insults during childhood and adolescence has particularly powerful and long-lasting consequences on health due to the persistence of bio-behavioural attributes that are acquired early in life1,2,3,4.
Many studies examined the relationship between early living conditions and health in later life using cohorts exposed to historical events as a natural experiment. Concerning developed countries, several papers have investigated the impact on health of WWII events, particularly the 1944-45 Dutch famine5,6,7,8,9,10, and the 1941-44 Leningrad siege11,12, and reported a higher incidence of breast cancer, type 2 diabetes, cardiovascular disease, stroke, and hypertension among cohorts exposed to famine during childhood or adolescence.
However, in most studies the health outcomes were self-reported, thus subject to errors and reporting bias compared with other sources of information, such as medical records or laboratory measurements13,14,15. In addition, many authors were unable to distinguish the direct effects of early life conditions from potential indirect effects mediated through changes in health behaviours and other health determinants, since such information is rarely available. Accounting for such mediating effects appears to be important; indeed, for example, hardship during childhood can have immediate adverse effects on schooling decisions and outcomes16, and thus affect health outcomes through reduced achieved education or adult socioeconomic status17. The experience of hardship may also influence an individual’s substance consumption or dietary pattern, which could in turn impact health outcomes18,19. Finally, many studies did not investigate heterogeneity of effects with respect to age at exposure and are therefore not able to inform policy makers which early life periods are particularly critical for health development.
In this paper, we used data from the French prospective cohort study E3N including ca. 100,000 women born between 1925 and 1950 to investigate the effects of exposure to World War II (WWII)-related under-nutrition during childhood and adolescence on the probability of suffering from hypertension, type 2 diabetes, and obesity later in life while considering potential confounders. In contrast to most existing studies, we used objectively measured health outcomes and also studied the relationship between food-deprivation and subsequent health-affecting behaviours (later-life sleep duration, tobacco consumption, and diet in terms of carbohydrate, lipid, protein and calorie intake) to explore potential indirect effects on health. Finally, we investigated whether the effects are heterogeneous with respect to age at exposure.
After the defeat in the Battle of France (10 May–25 June 1940), the French population experienced almost a decade of severe food supply problems. Access to food was directly affected by the military actions, the fragmentation of the national economy due to the German occupation, the German requisitions, and the contraction of imports and agricultural output20. A food rationing system was implemented in September 1940 but did not provide a sufficient diet. The initial rations for adults provided less than 1,700 calories per day and went as low as 1,000 calories in 1944. The most significant losses were in protein and fats. Only consumers with sufficient wealth or with connections to food-producing relatives or friends in the countryside could meet their nutritional needs through purchases on the black market or reception of care packages. Economic recovery required years and the last wartime controls were not lifted until 194921.
The global costs of type 2 diabetes, hypertension, and obesity, and most notably the costs associated with cardiovascular disease as a consequence of these conditions are large and will substantially increase in the coming decades22,23,24. Knowing more about the impact of early childhood conditions on adult health behaviour and health outcomes may allow policy makers to shift away from an emphasis on treatment in the later stages of disease to earlier, more effective preventive strategies and interventions to maximise health development.
Methods
Study population
The Etude Epidémiologique auprès de femmes de la Mutuelle Générale de l’Education Nationale or E3N is a French prospective cohort study which was initiated in 1990 to investigate risk factors of cancer and other major non-communicable diseases in women. E3N participants were insured through a national health system that primarily covered teachers and their families, and were enrolled in the study from 1990 onward after they had returned a baseline self-administered questionnaire. The cohort included nearly 100,000 women born between 1925 and 1950. Follow-up questionnaires were sent approximately every 2–3 years and addressed general and lifestyle characteristics together with medical events; the latter especially included cancers, cardiovascular diseases, type 2 diabetes, depression, fractures, and asthma. Our study includes data from the follow-up questionnaires until 2014. The follow-up questionnaire response rate remained stable over the whole study period at approximately 80%25. Due to active and passive follow-up (through the transfer of information on addresses, hospitalisations, vital status, reimbursed drugs from the files of the insurer MGEN who insures teachers and their families), the overall loss to follow-up was less than 3%. We used the entire E3N study population for which we have non-missing data on at least one of the health outcomes (diabetes, hypertension, obesity defined as BMI > 30 or overweight defined as BMI > 25) which resulted in a population of 90,226 women. All E3N study participants signed a written informed consent letter and the study protocol was reviewed and approved by the French National Commission for Data Protection and Privacy (ClinicalTrials.gov Identifier: NCT03285230).
Hypertension and type 2 diabetes assessment
Before 2004, all potential cases of type 2 diabetes were identified through follow-up questionnaires that included questions on the diagnosis of diabetes, diabetes-specific diet, diabetes drugs, and hospitalisations for diabetes. All potential cases were then contacted and asked to answer a diabetes-specific questionnaire that included questions on the circumstances of diagnosis (year of diagnosis, symptoms, biological exams, and fasting or random glucose concentration at diagnosis), diabetes therapy (prescription of anti-diabetic diet or physical activity, list of all used glucose-lowering drugs along time), and the most recent concentrations of fasting glucose and HbA1c. In order to be considered as validated, a potential case must have reported at least one of the following: (1) fasting plasma glucose ≥ 7.0 mmol/l or random glucose ≥ 11.1 mmol/l at diagnosis; (2) use of a glucose-lowering medication; (3) most recent values of fasting glucose or HbA1c concentrations ≥ 7.0 mmol/l or ≥ 7%, in the diabetes-specific questionnaire. After 2004, cases were identified through the drug reimbursement insurance database. The validation algorithm used in the E3N cohort to assess type 2 diabetes cases has been largely accepted and used in several previous publications (e.g. Mancini et al.26). All women who were reimbursed at least twice for any glucose-lowering medications during one year were considered to be validated cases of diabetes27.
Participants were asked to report whether they had hypertension at baseline and in each follow-up questionnaire sent every 2–3 year, the date of diagnosis, and the use of anti-hypertensive treatments. The month and year of diagnosis were provided for most cases (69%). For individuals who were missing the month of diagnosis (14% of cases), it was imputed to June of the year of diagnosis. The median time between the date of diagnosis and the date of response to the first questionnaire after diagnosis was 12 months. Thus, for the cases (n = 17%) with no year of diagnosis, we assigned it to be 12 months before they reported hypertension in a questionnaire. In 2004, a drug reimbursement database became available for 97.6% of participants. We used the self-reported date of diagnosis or the first date of drug reimbursement for anti-hypertensive medications (Anatomical Therapeutic Chemical Classification System codes C02, C03, C07, C08, and C09) whatever happened first, as the date of diagnosis for cases identified after 2004. In addition, using the information of the MGEN health insurance plan drug claim database, we assessed the validity of self-reported hypertension within the E3N cohort. We compared hypertension self-report to anti-hypertensive drug reimbursement (any of the above specified codes). A positive predictive value of 82% was observed among women alive in January 2004 and followed up to their response to the last considered questionnaire in 200828.
To gain statistical power for some of the regression analyses, we grouped the health outcome indicator variables into a new dichotomous variable equal to one if the individual was affected by any of the health conditions and zero otherwise.
Cofactors assessment
The E3N data provide information on a wide range of individual characteristics. Besides the date and place of birth, educational achievement, weight and height, a measure for the level of stress at work, and marital status, the data included information on early childhood conditions such as preterm birth, birth weight and height, age of the mother and father at birth, indicator variables for the individual’s and her father’s socioprofessional category, whether the individual lived on a farm, number of siblings, and information on the presence of type 2 diabetes and hypertension in the family. The data also included information on health behaviours, such as tobacco smoking, average hours of sleep per night, and dietary intake (used here as carbohydrate, protein, fat, and total calorie intakes).
Exposure to WWII-related food deprivation during childhood and adolescence
In the first questionnaire, the participants were asked how much they suffered from food deprivation related to WWII. The wording of the question was as follows: “How did you suffer from the food deprivations of the last World War?”. The possible answers were “not born at the time”, “not at all or little suffering”, “moderate suffering”, “a lot (continuous hunger)”, “enormously (deportation)”. Albeit subjective, this variable can be considered as a proxy measure of the intensity of the individual’s experience of hardship during WWII. From this variable, we constructed a dichotomous variable equal to one if the individual claimed to have suffered from hunger at least moderately and zero otherwise.
Statistical analysis
We regressed the health outcomes (diabetes, hypertension, obesity, overweight) and the health determinants (education, sleep duration, tobacco smoking, and diet in terms of carbohydrate, protein, lipid, and total energy intakes) on exposure to famine and a range of individual and family characteristics using Logit regressions to estimate marginal effects at the mean. The coefficient of the marginal effect at the means gives the change in probability of a health condition occurring for a one unit change in the explanatory variable when the values of all covariates within the sample are set to their means. We tried out different model adjustments to see whether our results were robust to the inclusion of the different cofactors. We included year of birth and place of birth fixed effects in all models, and clustered standard errors at the level of the department. The results were also robust to clustering at the level of the postcode area.
For the regressions on the health outcomes, we also estimated models in which we interacted exposure to famine with dummy variables indicating whether the individual belongs to a certain age group to investigate whether food deprivation impacts health outcomes differently when individuals are exposed at different stages of development. We defined five age cohorts: those born before WWII from 1925–1929 (aged 10–15 years at the beginning of WWII), born 1930–1934 (aged 5–10 years), born 1935–1939 (aged 0–5 years); those born during the war, i.e. 1940–1945, and those born after 1945.
All methods were performed in accordance with the relevant guidelines and regulations.
Results
WWII and risk of hypertension and type 2 diabetes at adulthood
Table 1 shows general summary statistics. Table 2 presents the results from our first model in which we estimated differences in the health outcomes for individuals who declared having suffered at least moderately from hunger during WWII and those who declared not having suffered. Our findings suggest that the experience of WWII-related food deprivation during early life is linked to a higher probability of developing type 2 diabetes and hypertension later in life. We did not find evidence for effects on the probability of being obese or overweight. More precisely, individuals who declared having suffered at least moderately from WWII-related hunger during childhood or adolescence had a 0.7% (95% CI: 0.073–1.37%) higher risk of suffering from type 2 diabetes and a 2.6% (95% CI: 0.81–4.45%) higher risk of suffering from hypertension at adulthood compared to unaffected individuals.
In this model, we controlled for a large range of potential cofounders. We included birth-year and department fixed effects, indicator variables for whether the individual lives with a spouse, achieved higher education, has been born preterm, lived on a farm for more than three months during childhood and whether the individual or her father belongs to a high socioprofessional category, the age of the individual’s mother and father at her birth, the number of siblings, the level of physical and mental stress experienced at work, an index of deprivation for the individual’s current area of residence, history of diseases running in the family and the variables concerning the individual’s health behaviour which include smoking, sleep and diet in terms of carbohydrate, protein, fat and calorie intake. Results are robust to the inclusion and exclusion of these different cofactors (tables are made available by the authors upon request), despite a large variation in the number of observations dropped due to the inclusion of certain cofactors with a large number of missing values. Notably, the results remain robust to the inclusion of health-affecting behaviours (tobacco consumption, sleep duration, and diet in terms of protein, lipid, carbohydrate and calorie intake), suggesting a direct association between early-life exposure and later-life risk for disease independently of potential changes in the health-affecting behaviours we observe in the data.
Interactions with age
In our second set of models, we included age group interaction terms to see whether experiencing hunger at different ages had differential effects on later life health. For higher statistical power, we used the indicator variable equal to one if the individual suffered from any of the health conditions and zero otherwise. Column 1 in Table 3 shows a positive association between having suffered hunger during early life and the risk to suffer from any health condition (type 2 diabetes and/or hypertension) later in life, which increased by 2.83% (95% CI: 1.1%–4.6%).
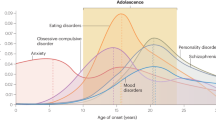
In column 2 of the same Table, we reported the estimates for the model with the age group interaction terms. The coefficients were of a higher magnitude for individuals who have been born from 1935 to 1939 (coefficient on “Hunger x born 1935-1939”) and were therefore aged 0 to 5 at the beginning of exposure (the onset of WWII). The association appeared to exist also for individuals born during the war (coefficient on “Hunger x born during WWII”) but the result is less statistically significant. Exposure to hunger does not yield statistically significant results for individuals who were older than 5 at the time of exposure. Figure 1 presents the point estimates and 95% confidence intervals graphically. Finding that the adverse effects of exposure to hunger were mainly present in individuals exposed before age 5 is suggestive evidence for the existence of a sensitive period of development during the first 5 years of life during which individuals appear to be particularly vulnerable to the exposure to adverse conditions.
Effect of exposure to hunger on the probability of suffering from any health condition (type 2 diabetes and/or hypertension) at adulthood. The arrows show the 95% confidence interval. Only the results for individuals born from 1935 to 1939 are statistically significantly different from 0. The estimate for individuals born from 1946 to 1950 is not precisely estimated as few individuals declared having suffered from WWII-related hunger.
The associations between exposure to hunger and later-life health remained when we adjusted for health-affecting behaviours (tobacco consumption, sleep duration, and diet in terms of protein, lipid, carbohydrate, and calorie intake). This can be seen from the coefficients presented in Columns 3 and 4 from models including health-affecting behaviours which are similar to the coefficients presented in Columns 1 and 2 from the models in which we do not adjust for health-affecting behaviours. This suggests a direct association between early-life exposure and later-life risk for disease independently of potential changes in the health-affecting behaviours we observe in the data.
WWII and changes in health determinants
To investigate the potential indirect pathways through which early-life exposure to hunger could affect adult health, we examined whether having suffered from hunger was associated with changes in health determinants such as educational achievement and health-affecting behaviours including sleep duration, tobacco smoking, and diet in terms of carbohydrate, protein, lipid, and calorie intake. Results are reported in Table 4. The experience of hunger during childhood was positively correlated with tobacco consumption and inversely associated with average sleep duration and achieved educational level. We did not find evidence for associations with diet. We adjusted for a range of cofactors including indicator variables for whether the individual lived with a spouse, had been born preterm, had lived on a farm for more than three months during childhood, whether the individual or her father belonged to a high socioprofessional category, the age of the individual’s mother and father at her birth, the number of siblings, the level of physical and mental stress experienced at work, and an index of deprivation for the individual’s current area of residence. All models included birth-year and birth-place fixed effects.
Discussion
We exploited data on 90,226 women from the French prospective cohort study E3N to estimate the long-run effects of exposure to World War II-related food deprivation during early life on the risk of developing type 2 diabetes, hypertension, and obesity at adulthood, while considering potential confounders. We also investigated whether the effects depended on the individual’s age at exposure. Finally, we examined the relationship between food-deprivation and subsequent health-affecting behaviours to explore potential indirect effects on health of severe food-deprivation.
We found that the experience of WWII-related food deprivation during early life was linked to a higher risk of developing type 2 diabetes (+0.7%, 95% CI: 0.073–1.37%) and hypertension (+2.6%, 95% CI: 0.81–4.45%) in adulthood. This still held true when we adjusted for a range of cofactors including health-affecting behaviours. The health of individuals who had been exposed up to age 5 appeared to be more affected than the health of individuals exposed at a later age. Exposure to hunger during early-life was also associated with different health determinants. We found a negative association between having suffered from hunger and educational achievement and mean sleep duration whereas the probability of ever smoking tobacco appeared to be higher among affected individuals.
Many studies investigated health outcomes in cohorts exposed to famine, and several found evidence that early malnutrition played a role in the origins of type 2 diabetes and high blood pressure. It was reported that women aged 6–8 at the peak of starvation during the 1941–44 Leningrad siege had higher systolic blood pressure compared to unexposed individuals born during the same period11. Women exposed to the 1944–1945 Dutch famine had an increased age-adjusted type 2 diabetes hazard ratio relative to unexposed women29. Severe under-nutrition at ages 11–14 among individuals exposed to the Dutch famine was reported to be associated with a higher probability of developing diabetes mellitus and/or peripheral arterial disease at ages 60–7610. Our findings are consistent with these results. Concerning the critical window of exposure, however, our findings differed from the aforementioned studies. We found that individuals exposed during early childhood (up to age 5) were more strongly affected whereas the previously cited studies identified mid- and late childhood as potential critical periods of exposure.
Relatively little information is available on the association between famine exposure and changes in health-affecting behaviours later in life. It was reported that early-life exposure to famine was associated with higher prevalence of smoking and physical activity later in life, but not with higher risk of unhealthy diet or of high alcohol consumption30. The negative association we identified between early-life hunger and sleep is in line with previous research indicating that disturbances of sleep are widespread in victims of adverse childhood experiences31,32. Our findings of a negative correlation between suffering from hunger and educational achievement are supported by Jyoti et al.16 who found that food insecurity negatively affects school children’s academic performance.
Within the Developmental Origins of Health and Disease (DOHaD) framework, the relationship between early life exposure and health trajectories across adulthood has been explained using both latency and pathway models. The latency model links early-life exposure to adult health outcomes in a direct manner independently of intervening life circumstances. It proposes that early-life exposures can program long-term or permanent changes in biological and behavioural systems1,2. This is based on the notion of biological imprinting which has been theorised by David Barker’s work33,34 who suggested that factors during early childhood make a biological imprint on the human organism in a way that makes it more susceptible to illness later in life. For example, Hertzman1 hypothesised that in utero and early life circumstances could affect the structure and functioning of the central nervous system, which interacts with the immune, hormonal, and clotting systems to increase or decrease susceptibility to disease.
In contrast, the pathway model proposes that early-life exposure indirectly relates to adult health outcomes through effects on health determinants and health-related behaviours. Ben-Shlomo35 discussed the pathway model in terms of “chains of risk” where one adverse exposure conditions the individuals’ response and leads to other adverse events. Negative childhood experiences may lead to unhealthy behaviours and poor school performance in adolescence, and limited opportunities in adulthood. Inadequate resources and stressful life circumstances in adulthood, in turn, increase the risk of morbidity and mortality. This pathway model is closely linked to the notion of allostatic load35, a concept used to explain how experiences become biologically embedded to influence health. The healthy functioning of a body requires ongoing adjustment through fluctuations in the physiologic system to respond to stressors. This process is referred to as allostasis36 and involves the sympathetic nervous system, the neuroendocrine system (in particular the hypothalamic-pituitary-adrenal axis), and the immune system. Internal needs are temporarily subjugated to external ones37, which is essential for survival but may have negative long-term effects, promoting illness in the case of individuals exposed to multiple acute or chronic stressors38. Multiple recurring stressors leave a physiologic stamp on the body39, which is reflected in bio-markers and in derangement of the body systems they have affected. This physiological stamp is the allostatic load, and it impairs the body’s ability to adapt to future stressors40.
The latency and pathway models are not competing explanations, but are thought to be intertwined in a complex manner. Chronic disease may be the long-term outcome of childhood conditions and experiences combined with cumulative exposures across adulthood41. Susceptibility to diseases is embedded in individuals’ biological makeup, but diseases are expressed and maintained in particular social, economic, and cultural environments2,42,43. Our findings are compatible with both the predictions of the latency and pathway models. We found a direct association between early-life exposure and later-life risk of diabetes and hypertension, which appears to persist when adjusting for health determinants recorded in E3N (i.e. education and health-affecting behaviours). We also found that exposure was linked to differences in these health determinants which, in turn, are likely to influence health18,44,45.
We investigated associations between early-life exposure to hunger and later life risk of diabetes and hypertension using verified data on health as opposed to self-declared data which is most commonly used in the literature. Our results are therefore not subject to potential bias from misreported health. The richness of the E3N data allowed us to adjust for a large range of family and individual characteristics including, most importantly, socioeconomic status which has been shown to be an important determinant of adult health outcomes46. We have also been able to explore the possibility that early-life food deprivation affected health determinants such as educational achievement, and health-affecting behaviours including sleeping duration, diet, and tobacco smoking, which may mediate the effects on health. In the existing literature, relatively little information is available on the association between famine exposure and changes in health determinants and behaviours later in life.
Our study has certain limitations. Despite having adjusted the regression models for a wide range of cofactors, we cannot conclude that the effects we find are causal. Exposure to hunger may still be correlated with unobserved individual and household characteristics which may also drive health determinants and/or health outcomes and may therefore bias our estimates. We also note that individuals who suffered from food deprivation could have been exposed to other WII-related stressors. We were not able to control for exposure to such stressors and their potential effects on health determinants and health outcomes. Finally, many potentially important health determinants are absent from the E3N data although they could have been affected by exposure to hunger and have influenced health outcomes. Our findings of a direct association between early-life exposure and adult health could be due to not being able to adjust for important unobserved factors which may have mediated the health outcomes. Finally, the estimates in our study are likely to be a lower bound for the effects of exposure to hunger on health outcomes as there may have been a change in the composition of the population caused by differential mortality. If the least healthy are more likely to die, the pool of survivors may on average be of better health. In such a case, the average health in a population that was intensely affected by hunger could be better than the average health of a less affected population, leading us to underestimate the impact of exposure to hunger on health.
To conclude, we briefly summarise our findings and provide policy recommendations as follows. We found that early-life exposure to food deprivation during childhood and especially during the first five years of life increased the risk of suffering from hypertension and type 2 diabetes at adulthood. This still held true when we adjusted for health determinants and health-related behaviours at adulthood. Exposure was also associated with differences in health determinants and behaviours, such as lower educational achievement, lesser amount of sleep, and higher probability of ever smoking tobacco at adulthood. Our findings are compatible with both the latency and the pathway models proposed in the Developmental Origins of Health and Disease framework which theorise the existence of both a direct link between early-life exposure and adult health outcomes due to the programming of long-term or permanent changes in biological systems, and an indirect link where early-life exposure affects health determinants such as health-related behaviours which, in turn, impact health outcomes. This new empirical evidence for the predictions of the Developmental Origins of Health and Disease hypothesis is potentially useful information for the targeting of policy interventions to improve the health outcomes of vulnerable individuals. Our results suggest that it is reasonable for policy makers to shift away from an emphasis on treatment in the later stages of disease to earlier, more effective preventive strategies and interventions to maximise health development, for example by increasing investments in early-childhood prevention programmes. In addition, policy-makers could target their policies at improving health-affecting behaviours (e.g. smoking, sleep hygiene), as health effects appear to be partially mediated by changes in these behaviours.
References
Hertzman, C. The biological embedding of early experience and its effects on health in adulthood. Annals New York Acad. Sci. 896, 85–95 (1999).
Halfon, N. & Hochstein, M. Life course health development: an integrated framework for developing health, policy, and research. The Milbank Quarterly 80, 433–479 (2002).
Baird, J. et al. Developmental origins of health and disease: a lifecourse approach to the prevention of non-communicable diseases. In Healthcare, vol. 5, 14 (Multidisciplinary Digital Publishing Institute, 2017).
Fall, C. H. & Kumaran, K. Metabolic programming in early life in humans. Philos. Transactions Royal Soc. B 374, 20180123 (2019).
Elias, S. G., Peeters, P. H., Grobbee, D. E. & Noord, P. A. V. Breast cancer risk after caloric restriction during the 1944–1945 dutch famine. Journal of the National Cancer Institute 96, 539–546 (2004).
Elias, S. G., Peeters, P. H., Grobbee, D. E. & van Noord, P. A. The 1944–1945 dutch famine and subsequent overall cancer incidence Cancer Epidemiology and Prevention Biomarkers14, 1981–1985 (2005).
Dirx, M. J., Van Den Brandt, P. A., Goldbohm, R. A. & Lumey, L. Diet in adolescence and the risk of breast cancer: results of the netherlands cohort study. Cancer Causes & Control 10, 189–199 (1999).
Dirx, M. J., van den Brandt, P. A., Goldbohm, R. A. & Lumey, L. Energy restriction in childhood and adolescence and risk of prostate cancer: results from the netherlands cohort study. American journal of epidemiology 154, 530–537 (2001).
Dirx, M. J., van den Brandt, P. A., Goldbohm, R. A. & Lumey, L. Energy restriction early in life and colon carcinoma risk: Results of the netherlands cohort study after 7.3 years of follow-up Cancer: Interdisciplinary. International Journal of the American Cancer Society 97, 46–55 (2003).
Portrait, F., Teeuwiszen, E. & Deeg, D. Early life undernutrition and chronic diseases at older ages: the effects of the dutch famine on cardiovascular diseases and diabetes. Social science & medicine 73, 711–718 (2011).
Koupil, I. et al. Blood pressure, hypertension and mortality from circulatory disease in men and women who survived the siege of leningrad. European journal of epidemiology 22, 223–234 (2007).
Sparén, P. et al. Long term mortality after severe starvation during the siege of leningrad: prospective cohort study. bmj 328, 11 (2004).
Dowd, J. B. & Zajacova, A. Does self-rated health mean the same thing across socioeconomic groups? evidence from biomarker data. Annals of epidemiology 20, 743–749 (2010).
Dowd, J. B. & Todd, M. Does self-reported health bias the measurement of health inequalities in us adults? evidence using anchoring vignettes from the health and retirement study Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 66, 478–489 (2011).
Jürges, H. True health vs response styles: exploring cross-country differences in self-reported health. Health economics 16, 163–178 (2007).
Jyoti, D. F., Frongillo, E. A. & Jones, S. J. Food insecurity affects school children’s academic performance, weight gain, and social skills. The Journal of nutrition 135, 2831–2839 (2005).
Leigh, J. P. Direct and indirect effects of education on health. Social Science & Medicine 17, 227–234 (1983).
Ezzati, M. & Riboli, E. Behavioral and dietary risk factors for noncommunicable diseases. New England Journal of Medicine 369, 954–964 (2013).
Murray, C. J. et al. Disability-adjusted life years (dalys) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010 The lancet 380, 2197–2223 (2012).
Mouré, K. & Schwartz, P. On vit mal: Food shortages and popular culture in occupied france, 1940–1944. Food, Culture & Society 10, 261–295 (2007).
Mouré, K. Food rationing and the black market in france (1940–1944). French history 24, 262–282 (2010).
Guariguata, L. et al. Global estimates of diabetes prevalence for 2013 and projections for 2035 Diabetes research and clinical practice 103, 137–149 (2014).
Bommer, C. et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes care 41, 963–970 (2018).
Organization, W. H. et al. A global brief on hypertension: silent killer, global public health crisis: World health day 2013. Tech. Rep., World Health Organization (2013).
Clavel-Chapelon, F. & Group, E. S. Cohort profile: the french e3n cohort study. International journal of epidemiology 44, 801–809 (2014).
Mancini, F. R. et al. Dietary antioxidant capacity and risk of type 2 diabetes in the large prospective e3n-epic cohort. Diabetologia 61, 308–316 (2018).
Laouali, N. et al. Dietary inflammatory index and type 2 diabetes risk in a prospective cohort of 70,991 women followed for 20 years: the mediating role of bmi Diabetologia 1–11, https://doi.org/10.1007/s00125-019-04972-0 (2019).
Villaverde, P. et al. High dietary total antioxidant capacity is associated with a reduced risk of hypertension in french women. Nutrition journal 18, 31 (2019).
van Abeelen, A. F. et al. Famine exposure in the young and the risk of type 2 diabetes in adulthood. Diabetes 61, 2255–2260 (2012).
Fransen, H. P. et al. Exposure to famine at a young age and unhealthy lifestyle behavior later in life. PloS one 11, e0156609 (2016).
Bader, K., SchÄfer, V., Schenkel, M., Nissen, L. & Schwander, J. dverse childhood experiences associated with sleep in primary insomnia. Journal of sleep research 16, 285–296 (2007).
Chapman, D. P. et al. Adverse childhood experiences and frequent insufficient sleep in 5 us states, 2009: a retrospective cohort study BMC public health 13, 3 (2013).
Barker, D. Fetal origins of diseases of old age European journal of clinical nutrition. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Fetal+origins+of+diseases+of+old+age&btnG=. (1992).
Barker, D. J. et al. Fetal nutrition and cardiovascular disease in adult life. The Lancet 341, 938–941 (1993).
Ben-Shlomo, Y. et al. Immediate postnatal growth is associated with blood pressure in young adulthood: the barry caerphilly growth study. Hypertension 52, 638–644 (2008).
Sterling, P. & Eyer, J. Biological basis of stress-related mortality. Social Science & Medicine Part E: Medical Psychology 15, 3–42 (1981).
Porges, S. W. Cardiac vagal tone: a physiological index of stress. Neuroscience & Biobehavioral Reviews 19, 225–233 (1995).
McEwen, B. S. & Stellar, E. Stress and the individual: mechanisms leading to disease. Archives of internal medicine 153, 2093–2101 (1993).
Seplaki, C. L., Goldman, N., Weinstein, M. & Lin, Y.-H. How are biomarkers related to physical and mental well-being? The Journals Gerontol. Ser. A: Biol. Sci. Med. Sci. 59, B201–B217 (2004).
Szanton, S. L., Gill, J. M. & Allen, J. K. Allostatic load: a mechanism of socioeconomic health disparities? Biological Research for Nursing 7, 7–15 (2005).
Blackwell, D. L., Hayward, M. D. & Crimmins, E. M. Does childhood health affect chronic morbidity in later life? Social science & medicine 52, 1269–1284 (2001).
Power, C. & Hertzman, C. Social and biological pathways linking early life and adult disease. British medical bulletin 53, 210–221 (1997).
Hamil-Luker, J. & Angela, M. Gender differences in the link between childhood socioeconomic conditions and heart attack risk in adulthood. Demography 44, 137–158 (2007).
Hu, F. B. et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. Obstetrical & gynecological survey 57, 162–164 (2002).
Gangwisch, J. E. et al. Short sleep duration as a risk factor for hypertension: analyses of the first national health and nutrition examination survey. hypertension 47, 833–839 (2006).
Everson, S. A., Maty, S. C., Lynch, J. W. & Kaplan, G. A. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J. psychosomatic research 53, 891–895 (2002).
Acknowledgements
The authors are grateful to all participants for providing the data used in the E3N cohort study. The E3N cohort is being carried out with the financial support of the “Mutuelle Générale de l’Education Nationale”, European Community, French League against Cancer, Gustave Roussy, and French Institute of Health and Medical Research. This present study was also supported by the French Research Agency (Agence Nationale de la Recherche) via an “Investissement d’Avenir” grant (investment for the future grant, ANR-10-COHO-0006) that supports the E4N study and by the Strategic Research Initiative NutriPerso from the University Paris-Saclay. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of this manuscript.
Author information
Authors and Affiliations
Contributions
J.M., O.A., G.F. conceived the study. J.M. and G.F. wrote the first and successive drafts of the manuscript. J.M. modelled and analysed the data. G.F. collected the data. All authors including M.-C.B.-R. and M.-A.C. revised the manuscript for important intellectual content. G.F. had full access to the data and takes full responsibility for the integrity of the data and the accuracy of the data analysis. G.F. is the study guarantor.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mink, J., Boutron-Ruault, MC., Charles, MA. et al. Associations between early-life food deprivation during World War II and risk of hypertension and type 2 diabetes at adulthood. Sci Rep 10, 5741 (2020). https://doi.org/10.1038/s41598-020-62576-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-62576-w
This article is cited by
-
Childhood and Infant exposure to famine in the Biafran war is associated with hypertension in later life: the Abia NCDS study
Journal of Human Hypertension (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.