Abstract
Laparoscopic appendectomy (LA) for treatment of acute appendicitis has gained acceptance with its considerable benefits over open appendectomy. LA, however, can involve some adverse outcomes: morbidity, prolonged length of hospital stay (LOS) and hospital readmission. Identification of predictive factors may help to identify and tailor treatment for patients with higher risk of these adverse events. Our aim was to identify risk factors for serious morbidity, prolonged LOS and hospital readmission after LA. A database compiled information of patients admitted for acute appendicitis from eighteen Polish and German surgical centers. It included factors related to the patient characteristics, peri- and postoperative period. Univariate and multivariate logistic regression models were used to identify risk factors for serious perioperative complications, prolonged LOS, and hospital readmissions in acute appendicitis cases. 4618 laparoscopic appendectomy patients were included. First, although several risk factors for serious perioperative complications (C-D III-V) were found in the univariate analysis, in the multivariate model only the presence of intraoperative adverse events (OR 4.09, 95% CI 1.32–12.65, p = 0.014) and complicated appendicitis (OR 3.63, 95% CI 1.74–7.61, p = 0.001) was statistically significant. Second, prolonged LOS was associated with the presence of complicated appendicitis (OR 2.8, 95% CI: 1.53–5.12, p = 0.001), postoperative morbidity (OR 5.01, 95% CI: 2.33–10.75, p < 0.001), conversions (OR 6.48, 95% CI: 3.48–12.08, p < 0.001) and reinterventions after primary procedure (OR 8.79, 95% CI: 3.2–24.14, p < 0.001) in the multivariate model. Third, although several risk factors for hospital readmissions were found in univariate analysis, in the multivariate model only the presence of postoperative complications (OR 10.33, 95% CI: 4.27–25.00), reintervention after primary procedure (OR 5.62, 95% CI: 2.17–14.54), and LA performed by resident (OR 1.96, 95% CI: 1.03–3.70) remained significant. Laparoscopic appendectomy is a safe procedure associated with low rates of complications, prolonged LOS, and readmissions. Risk factors for these adverse events include complicated appendicitis, postoperative morbidity, conversion, and re-intervention after the primary procedure. Any occurrence of these factors during treatment should alert the healthcare team to identify the patients that require more customized treatment to minimize the risk for adverse outcomes.
Similar content being viewed by others
Introduction
One of the most common intraabdominal conditions requiring surgical intervention is acute appendicitis (AA). According to the Global Burden of Disease Study (2016), 114.44 to 481.60 surgeries were required per 100 000 incidences of AA, depending on the socio-economic level of countries1. The incidence of appendicitis in newly industrialized countries is rising rapidly2. Appendectomy is the standard treatment of choice for acute appendicitis3,4. Although open appendectomy (OA) performed through the right lower quadrant incision remained nearly unchanged for over a century because of its safety and efficacy, laparoscopic appendectomy (LA) has gradually gained acceptance. Recent studies show that laparoscopic appendectomy provides considerable benefits over open appendectomy, including a lower complication rate, a shorter length of hospital stay (LOS), less postoperative pain and earlier postoperative recovery5,6. Laparoscopy also was associated with lower surgical site infection (SSI) rates7,8.
As with any surgical procedure, however, LA is associated with some risk of unfavorable outcomes. In general, the rate of perioperative complications and the length of hospital stay are universal measures of quality of treatment. Special attention was also paid to the readmission rates. Despite the constant improvements in perioperative care and increasing popularity of laparoscopy, certain patients still develop complications after LA. Although these unfavorable postoperative courses occur rather rarely in appendectomy comparison to other abdominal procedures, patients with these outcomes suffer delayed recovery.
Although laparoscopic appendectomy is slowly becoming the gold standard in acute appendicitis treatment thanks to growing evidence from the results of randomized controlled trials comparing LA with open surgery, data from large cohorts is still lacking. Such analyses may reflect more realistic populations without the restrictions commonly present in clinical trials. Therefore, we designed a multicenter cohort study to analyze the risk factors for unfavorable postoperative outcomes: morbidity, prolonged length of stay and readmissions after LA.
Methods
Study design
A study was performed over a 6-month period involving 18 Polish and German surgical centers. A database compiled the data of patients admitted for acute appendicitis9. The local team of nurses, anesthesiologists, and assistants along with the coordinating surgeon acquired data in each participating surgical unit.
The database included following patient characteristics: sex, age, and body mass index (BMI). It also followed many operative metrics: type of acute appendicitis (uncomplicated or complicated as determined by the presence of gangrenous appendicitis or perforated appendix with or without abscess)10, intraoperative adverse events (IAE), and postoperative outcomes (postoperative morbidity, need for surgical reintervention, LOS, and need for readmission to the original surgical department for whatever reason).
It was built along several parameters: ASA score, history of smoking, diabetes mellitus (DM), timing from onset of symptoms to surgery, operative parameters. The study adhered to the guidelines of The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement11. Complicated AA was diagnosed relying imaging diagnostics and/or visualization during relaparoscopy/relaparotomy performed due to patient’s condition.
The Videosurgery Chapter of the Association of Polish Surgeons supported this project. No changes in treatment strategy were included in the study protocol. A chief investigator had the responsibility of monitoring this study, by verifying missing or unclear data entered into the database. The database was anonymous as any information that could possibly identify the patients was excluded. Due to the observational nature and lack of patient personal data the study did not need informed consent. Approval by the ethics committee has been obtained from each of the participating centers for conducting this study. The presence of major complications (Clavien-Dindo III-V)12 in the postoperative period, prolonged LOS (LOS equal or longer than 2*upper quartile was recognized as prolonged LOS) and the need for readmission within 30 days were analyzed in order to identify potential risk factors.
Statistical analysis
Statistical analyses were done using Statsoft STATISTICA 13.0 PL (Statsoft Inc., Tulsa, Oklahoma, USA). Continuous variables were presented using means with standard deviations (SD) or medians with inter-quartile ranges (IQR) for skewed variables. Groups were compared using Kruskal-Wallis’ ANOVA test with multiple comparison of ranges. Then, comparisons between groups were done using t-student tests for normally distributed variables and Mann-Whitney’s tests for skewed variables. Dichotomous variables were included in chi-squared Pearson’s, Yates’, and Fisher’s exact tests, depending on the quantities in the subgroups. Finally, univariate and multivariate logistic regression models were built to determine odds ratios for risk factors depending on postoperative complications, prolonged LOS and need for readmission. Results were considered statistically significant when p-values were <0.05. In the case of missing data, pairwise deletion was used.
Ethics approval and consent to participate in the study
Ethics approval of the ethics committee of Jagiellonian University Medical College was obtained (nr 1072.6120.204.2018 20.09.2018). The data was completely anonymized, and no patient or hospital information was collected in the database. The study protocol was approved by the board of the Videosurgery Chapter of the Association of Polish Surgeons, and the study was conducted under its supervision. All procedures have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments (Fortaleza).
Results
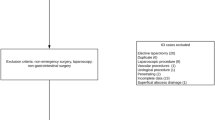
4618 patients qualified for laparoscopic appendectomy. Table 1 presents the demographic data for these patients.
In terms of gender differences, the number of males, 2409 (52.2%), exceeded that of females, 2209 (47.8%). The median age of patients was 33 years (IQR 24–47). Median BMI was 24.8 (IQR 22.03–28.5). 794 (19.19%) were active smokers and 147 (3.18%) had diabetes mellitus. The majority of patients, 3214 (69.60%), were classified as ASA I patients. The remainder were sorted as such: 1213 (26.27%) patients as ASA II, 184 (3.98%) patients as ASA III, and 7 (0.15%) patients as ASA IV. In 1463 (31.68%) patients, symptoms of AA were present 48 hours before surgery. The number of patients with postoperative morbidity were 310 (6.71%); according to the Clavien-Dindo (C-D) classification of surgical complications there were 3 (0.06%) patients with class V complications, 4 (0.09%) class IV, 77 (1.67%) class III, 80 (1.73%) class II, and 146 (3.16%) class I. As for complications; there were surgical site infection (1.97%,), intraabdominal abscess (1.3%), ileus (0.54%), intraabdominal bleeding (0.41%), pneumonia (0.39%), urinary tract infection (0.39%), diffuse peritonitis (0.17%), deep vein thrombosis (0.06%), bowel perforation (0.04%), pulmonary embolism (0.02%) and other (1.41%). Median length of stay (LOS) in the entire cohort was 32,3,4 days. Prolonged LOS (LOS ≥8 days) was necessary in 227 (4.92%) of them, whereas readmission was recorded in 110 (2.56%) cases.
In univariate regression models, factors were identified that increase the risk of perioperative serious complications (C-D III-V) whose parameters are presented in Table 2. When a multivariate model was built taking into consideration parameters significant in univariate calculations, only intraoperative adverse events (OR 4.09, 95% CI 1.32–12.65, p = 0.014) and complicated appendicitis (OR 3.63, 95% CI 1.74–7.61, p = 0.001) remained significant (Table 2).
Table 3 shows the details of univariate logistic regression models for increases in the risk of prolonged LOS. In the later multivariate model, only complicated appendicitis (OR 2.8, 95% CI: 1.53–5.12, p = 0.001), postoperative morbidity (OR 5.01, 95% CI: 2.33–10.75, p < 0.001), conversions (OR 6.48, 95% CI: 3.48–12.08, p < 0.001) and reinterventions after primary procedure (OR 8.79, 95% CI: 3.2–24.14, p < 0.001) were statistically significant.
In univariate logistic regression analysis following risk factors for hospital readmissions were identified and presented in Table 4. However, in multivariate regression, only postoperative complications (OR 10.33, 95% CI: 4.27–25.00), reintervention after primary procedure (OR 5.62, 95% CI: 2.17–14.54), and LA performed by resident (OR 1.96, 95% CI: 1.03–3.70) remained significant.
Discussion
In our study we identified risk factors for serious morbidity, prolonged length of hospital stay and hospital readmission after LA. The risk factors for serious morbidity were complicated appendicitis and IAE; for prolonged hospital stay, they were complicated appendicitis, postoperative morbidity, conversion, and reintervention after primary surgery; and for hospital readmission: operation performed by surgical resident, perioperative morbidity and reintervention were risk factors. Interestingly, complicated appendicitis was an independent risk factor for complications and prolonged hospital stay as well, but it was not associated with a higher hospital readmission rate.
Our study reported an overall complications rate of about 6%. It is comparable with data reported in large cohorts that allows objective analysis of our results13,14,15,16. Importantly, LA in our cohort is characterized by low mortality (0.06%) and by a very low percentage (1.82%) of severe morbidity expressed as Clavien Dindo III-V, which proves the safety of the procedure. Andert et al. reported similar data. In this study, 1.7% of patients presented with major complications17. In an Australian study, 2.7% presented with an intra-abdominal abscess and 1.5% patients needed further intervention15. Large cohorts showed higher mortality up to 0.6%18,19,20. Although univariate logistic regression models showed several risk factors for severe postoperative complications, in the multivariate model only the presence of complicated appendicitis (OR 3.63) and intraoperative adverse events (OR 4.09) proved to be an independent risk factors associated with postoperative morbidity. Tiwari et al. observed that the severity of appendicitis correlated with higher morbidity and mortality independent of whether OA or LA was performed21. What has to be emphasized is that some clinical conditions have been previously identified as related to complicated AA, such as the co-existence of diabetes mellitus, elevated CRP, and leukocytosis22,23. Moreover, complicated appendicitis is often the reason to conversion and longer operative time24,25. It seems, therefore, that complicated AA may be simply considered a different condition that has the most significant impact on outcomes.
This observation regarding complicated AA has also been confirmed when prolonged LOS was analyzed. This condition remained the only independent factor for delayed recovery, apart from factors that are inevitably associated with longer hospital stay such as conversion or complications. LOS frequently depends on the traditional attitude and model of perioperative care26. Median LOS in the entire cohort in our study was 3 days, similar to previous reports19,26. On the other hand, there are studies reporting LA in uncomplicated acute appendicitis in an ambulatory setting27,28,29,30. Therefore, to confirm the real prolonged LOS we used 2*75 IQR of the entire cohort (8 days). Only less than 5% had prolonged LOS. In our opinion, this period was associated with either postoperative complications or delayed recovery. In addition, we confirmed that conversion might contribute to prolonged LOS. This obvious fact has been extensively studied before in comparative studies and randomized controlled trials including LA and open procedure31. The reason for conversion was often severe inflammatory process, periappendiceal abscess or intraoperative adverse events. These may be the real cause of longer hospital stay, not the conversion itself. In the majority of cases such patients required longer antibiotic treatment or developed postoperative complications. So prolonged LOS was a consequence of these circumstances.
Patients who developed complications or required reintervention had higher rates of readmission. This fact should be taken under consideration when discharging such patients even if in good condition. On the contrary, complicated appendicitis was not a risk factor for readmission. Interestingly, patients operated by residents had a higher risk of readmission. In all centers participating in the study, hospital discharge is based on the decision of the attending surgeon, not the resident. We can exclude any erroneous assessment of the patient’s condition by residents before discharge. On the basis of our study we could not clearly identify any causal explanation for that finding. Nevertheless, Jolley et al. also concluded that the involvement of resident in operation was associated with higher risk of readmission (OR 1.54 (1.23–1.94)32. They were, however, not able to explain this phenomenon. On the other hand, Advani et al. reported lower risk of hospital readmission when the resident was involved in operation33. Other studies show that appendectomy performed by residents is not associated with more complications34,35. Even though whether residents performed LA is linked with readmission rates, it is still considered a perfect model for training in laparoscopic surgery35. Those contradictory results suggest that the evidence on the impact of residents in performing LA is rather weak and requires further investigation.
Our study does have certain limitations as in other observational multicenter reports. First, most of the patients were included retrospectively, rendering it impossible to analyze accurately each participating center’s perioperative protocol, such as antibiotic regimens or discharge criteria. As shown in other large observational studies, management of AA among surgical centers significantly varied19. The design of the study did not introduce any changes in the perioperative protocols in each participating centers. It is likely the surgical care, antibiotic regimens and perhaps even the technique differed in each center. We, however, believe it has little impact on final outcomes and allowed us to draw more universal conclusions. Second, the readmission rate in our data only represents readmissions to the original surgical department due to complications, instead of the overall rate that included readmissions to other departments or hospitals, which could underestimate the true readmission rate. The readmission statistics, however, are combined from all study groups, reducing bias. Third, the surgical procedures were performed by surgeons with different surgical skills. Subsequently, we did not differentiate between types of diabetes and we did not take into account complications related to diabetes. Although type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) have different backgrounds, the mechanism leading to complications (e.g. infectious) is relatively similar. Therefore, we have decided not to differentiate between types of DM. Lastly, in our study the diagnosis of complicated AA was based on intraoperative and pathological visualization of the appendix36. Imran et al. reported that even 40% of patients were incorrectly classified when comparing intraoperative image of the appendix to results of pathological examination37.
Conclusions
Our study confirmed that laparoscopic appendectomy is a safe procedure associated with low rates of complications, prolonged LOS, and readmissions. We identified risk factors for those events such as complicated appendicitis, postoperative morbidity, conversion and reintervention after primary procedure. Occurrence of these events during treatment should alert the surgeons and help select patients that might require customized treatment to minimize the risk of these adverse events.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
06 December 2019
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Salomon, J. A. et al. Healthy life expectancy for 187 countries, 1990–2010: a systematic analysis for the Global Burden Disease Study 2010. Lancet. 380(9859), 2144–62 (2012).
Ferris, M. et al. The Global Incidence of Appendicitis: A Systematic Review of Population-based Studies. Ann Surg. 266(2), 237–41 (2017).
Sartelli, M. et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 12(1), 29 (2017).
Poon, S. H. T. et al. The current management of acute uncomplicated appendicitis: should there be a change in paradigm? A systematic review of the literatures and analysis of treatment performance. World J Emerg Surg. 12, 46 (2017).
Li, X. et al. Laparoscopic versus conventional appendectomy–a meta-analysis of randomized controlled trials. BMC Gastroenterol. 10, 129 (2010).
Di Saverio, S. et al. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg. 11, 34 (2016).
Collaborative, GlobalSurg. Laparoscopy in management of appendicitis in high-, middle-, and low-income countries: a multicenter, prospective, cohort study. Surg Endosc. 32(8), 3450–66 (2018).
Lasek, A. et al. Risk factors for intraabdominal abscess formation after laparoscopic appendectomy – results from the Pol-LA (Polish Laparoscopic Appendectomy) multicenter large cohort study. Videosurgery and Other Miniinvasive Techniques. 13(1), 70–78 (2018).
Lasek, A. et al. The significant impact of age on the clinical outcomes of laparoscopic appendectomy: Results from the Polish Laparoscopic Appendectomy multicenter large cohort study. Medicine (Baltimore). 97(50), e13621, https://doi.org/10.1097/MD.0000000000013621 (2018).
Pedziwiatr, M. et al. Complicated appendicitis: Risk factors and outcomes of laparoscopic appendectomy-Polish laparoscopic appendectomy results from a multicenter, large-cohort study. Ulusal travma ve acil cerrahi dergisi= Turkish journal of trauma & emergency surgery: TJTES. 25(2), 129–136 (2019).
Von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 370(9596), 1453–7 (2007).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of Surgical Complications: A New Proposal With Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann Surg. 240(2), 205–213 (2004).
Childers, C. P., Dworsky, J. Q., Maggard-Gibbons, M. & Russell, M. M. The contemporary appendectomy for acute uncomplicated appendicitis in adults. Surgery. 165(3), 593–601 (2019).
Faiz, O. et al. Traditional and laparoscopic appendectomy in adults: outcomes in English NHS hospitals between 1996 and 2006. Ann Surg. 248(5), 800–806 (2008).
Arthur, T., Gartrell, R., Manoharan, B. & Parker, D. Emergency appendicectomy in Australia: findings from a multicentre, prospective study. ANZ J Surg. 87(9), 656–60 (2017).
Ukai, T. et al. Evidence of surgical outcomes fluctuates over time: results from a cumulative meta-analysis of laparoscopic versus open appendectomy for acute appendicitis. BMC Gastroenterol. 16(1), 37 (2016).
Andert, A. et al. Risk factors for morbidity after appendectomy. Langenbecks Arch Surg. 402(6), 987–993 (2017).
Andersson, R. E. Short and long-term mortality after appendectomy in Sweden 1987 to 2006. Influence of appendectomy diagnosis, sex, age, co-morbidity, surgical method, hospital volume, and time period. A national population-based cohort study. World J Surg. 37(5), 974–981 (2013).
Sartelli, M. et al. Prospective Observational Study on acute Appendicitis Worldwide (POSAW). World J Emerg Surg. 13, 19 (2018).
Bregendahl, S., Norgaard, M., Laurberg, S. & Jepsen, P. Risk of complications and 30-day mortality after laparoscopic and open appendectomy in a Danish region, 1998–2007; a population-based study of 18,426 patients. Pol Przegl Chir. 85(7), 395–400 (2013).
Tiwari, M. M., Reynoso, J. F., Tsang, A. W. & Oleynikov, D. Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg. 254(6), 927–932 (2011).
Moon, H. M., Park, B. S. & Moon, D. J. Diagnostic Value of C-reactive Protein in Complicated Appendicitis. J Korean Soc Coloproctol. 27(3), 122–126 (2011).
Tsai, S. H., Hsu, C. W., Chen, S. C., Lin, Y. Y. & Chu, S. J. Complicated acute appendicitis in diabetic patients. Am J Surg. 196(1), 34–39 (2008).
Malagon, A. M., Arteaga-Gonzalez, I. & Rodriguez-Ballester, L. Outcomes after laparoscopic treatment of complicated versus uncomplicated acute appendicitis: a prospective, comparative trial. J Laparoendosc Adv Surg Tech A. 19(6), 721–725 (2009).
Finnerty, B. M. et al. Conversion-to-open in laparoscopic appendectomy: A cohort analysis of risk factors and outcomes. Int J Surg. 40, 169–175 (2017).
Andersson, R. E. Short-term complications and long-term morbidity of laparoscopic and open appendicectomy in a national cohort. Br J Surg. 101(9), 1135–1142 (2014).
Millien, J. E., Townsend, M., Goldberg, J. & Fuhrman, G. M. An Analysis of Factors that Predict Hospital Readmission after Surgery for Perforated Appendicitis. Am Surg. 83(9), 991–995 (2017).
Trejo-Avila, M. E. et al. Enhanced recovery after surgery protocol allows ambulatory laparoscopic appendectomy in uncomplicated acute appendicitis: a prospective, randomized trial. Surg Endosc. 33(2), 429–436 (2019).
Rosen, D. R. et al. Outpatient Laparoscopic Appendectomy: Feasible in a Public County Hospital? J Am Coll Surg. 224(5), 862–867 (2017).
Gignoux, B. et al. Should ambulatory appendectomy become the standard treatment for acute appendicitis? World J Emerg Surg. 13, 28 (2018).
Kim, J. K. et al. Does Conversion Adversely Impact the Clinical Outcomes for Patients with Complicated Appendicitis? J Laparoendosc Adv Surg Tech A. 26(8), 635–640 (2016).
Jolley, J., Lomelin, D., Simorov, A., Tadaki, C. & Oleynikov, D. Resident involvement in laparoscopic procedures does not worsen clinical outcomes but may increase operative times and length of hospital stay. Surg Endosc. 30(9), 3783–3791 (2016).
Advani, V., Ahad, S., Gonczy, C., Markwell, S. & Hassan, I. Does resident involvement effect surgical times and complication rates during laparoscopic appendectomy for uncomplicated appendicitis? An analysis of 16,849 cases from the ACS-NSQIP. Am J Surg. 203(3), 347–352 (2012).
Siam, B. et al. Comparison of Appendectomy Outcomes Between Senior General Surgeons and General Surgery Residents. JAMA Surg. 152(7), 679–685 (2017).
Perry, Z. H., Netz, U., Mizrahi, S., Lantsberg, L. & Kirshtein, B. Laparoscopic appendectomy as an initial step in independent laparoscopic surgery by surgical residents. J Laparoendosc Adv Surg Tech A. 20(5), 447–450 (2010).
Gomes, C. A. et al. Acute appendicitis: proposal of a new comprehensive grading system based on clinical, imaging and laparoscopic findings. World J Emerg Surg. 10, 60 (2015).
Imran, J. B. et al. Predictors of a histopathologic diagnosis of complicated appendicitis. J Surg Res. 214, 197–202 (2017).
Acknowledgements
The authors received no grants, equipment, or funding for this study.
Author information
Authors and Affiliations
Contributions
Conception or design of the work: P.Mi., L.An., P.M. The acquisition of data: Wal.M., L.A., B.M., My.P., A.K., B.M., C.K., C.R., C.W., D.W.N., D.J., F.P., H.W., K.A., K.W.K., K.J., K.P., K.Ar., K.Ad., K.K., K.M., L.Ag., L.L., Ma.P., M.W., M.T.P., Mi.M., Ma.M., N.A., N.D., O.R., P.Ma., P.P.M., R.M., S.T., S.A., S.P., S.R., T.S., E.T.V., Was.M., Wie.M., W.A., W.J.W., Z.L. Analysis and interpretation of data: P.Mi., Wys.M., Wal.M., L.A. Preparing tables: P.Mi., Wys.M., Wal.M. Writing draft & editing it: P.Mi., Wal.M., L.A., S.M. Writing–review & editing it: P.Mi., Wal.M.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Walędziak, M., Lasek, A., Wysocki, M. et al. Risk factors for serious morbidity, prolonged length of stay and hospital readmission after laparoscopic appendectomy - results from Pol-LA (Polish Laparoscopic Appendectomy) multicenter large cohort study. Sci Rep 9, 14793 (2019). https://doi.org/10.1038/s41598-019-51172-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-51172-2
This article is cited by
-
Beyond acute appendicitis: a single-institution experience of unexpected pathology findings after 989 consecutive emergency appendectomy
Langenbeck's Archives of Surgery (2024)
-
Single versus double Hem-o-lok clips to secure the apendiceal stump during laparoscopic appendectomy: a prospective randomized multicentric clinical trial
Langenbeck's Archives of Surgery (2024)
-
Ethnic disparities in pediatric appendicitis: the impact of hispanic ethnicity on presentation, complications, and postoperative outcomes
International Journal of Colorectal Disease (2024)
-
Is acute appendicitis more severe in foreign workers of northern Israel? A retrospective cohort study
European Journal of Trauma and Emergency Surgery (2023)
-
What happens after the kidney biopsy? The findings nephrologists should know
BMC Nephrology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.