Abstract
The bacterium Helicobacter pylori was originally classified in the Campylobacter genus, which contains major periodontopathic bacterial species, and H. pylori DNA has been found in the oral cavity. Although many studies show an association between the presence of periodontal bacteria and an overweight body-mass index (BMI; >25 kg/m2), the relationship between body weight and the presence of H. pylori in the oral cavity has not been demonstrated. Herein, we analysed the relationship between H. pylori in the oral cavity and systemic conditions, including the overweight BMI. Saliva specimens and extracted teeth were obtained from 87 subjects; the distribution of H. pylori among these specimens was analysed with the polymerase chain reaction. Subjects with an overweight BMI exhibited significantly higher detection rates of H. pylori in saliva, compared with non-overweight subjects (BMI <25 kg/m2) (P < 0.05). A clinical history of digestive diseases was not associated with the presence of H. pylori in overweight subjects, whereas subjects with both severe dental caries and an overweight BMI showed a higher detection rate of H. pylori in saliva specimens, compared with other groups. These results suggest that the detection of H. pylori in the oral cavity could be associated with the overweight BMI, which was predominant among subjects with severe dental caries.
Similar content being viewed by others
Introduction
Helicobacter pylori is a Gram-negative microaerophilic bacterium which is mainly isolated from the stomach and duodenum1. H. pylori was previously classified in the Campylobacter genus, which also contains several major periodontal bacterial species; initial infection by the bacterium is considered to occur mainly in childhood, before the age of 5 years, via the oral cavity1. Although some individuals harbouring H. pylori exhibit no symptoms, chronic infection by the bacterium increases the risk of gastric diseases, such as peptic ulcers or cancer2.
The existence of H. pylori in gastric tissue is diagnosed by endoscopic biopsy, serum antibody, urea breath test, and/or stool antigen test3; polymerase chain reaction (PCR) methods are widely used for the detection of H. pylori in the oral cavity4. According to previous studies that have shown H. pylori detection in oral specimens, such as dental plaque and saliva, by using PCR methods, the oral cavity may be a potential reservoir and reinfection source of H. pylori5. The prevalence of H. pylori in saliva specimens obtained from Japanese subjects was estimated to be 6.4%, using the PCR method6. Although a large number of PCR methods are available, the detection of H. pylori from among approximately 700 oral bacterial species—with high specificity and sensitivity—is quite difficult7,8. Thus, we recently developed a novel nested PCR procedure by using reliable primer sets, which were designed based on genome sequences from approximately 50 H. pylori strains8,9.
Overweight and obese body-mass indexes (BMIs) constitute a global problem, especially in developed countries, as one of the most important risk factors for metabolic syndrome and various diseases10,11. Many studies have shown a positive association between the presence of H. pylori in gastric tissue and the onset of metabolic syndrome12,13,14. Additionally, it is widely known that periodontal bacterial species are closely associated with the presence of systemic diseases that involve weight change, such as diabetes, obesity, and non-alcoholic fatty liver disease15,16,17. Furthermore, recent studies have shown that infection with specific cariogenic bacteria is associated with increased body weight18,19. However, the relationship between H. pylori colonization in the oral cavity and increased body weight remains unknown20. In the present study, we investigated the relationship between H. pylori colonization in the oral cavity and a variety of clinical factors, with particular focus on overweight BMI.
Results
Clinical characteristics of H. pylori-positive and H. pylori-negative subjects
A total of 87 subjects were divided into two groups based on the absence (H. pylori-negative) (n = 71; 81.6%) or presence (H. pylori-positive) (n = 16; 18.4%) of H. pylori in the oral cavity. H. pylori-positive subjects were further stratified into those who exhibited H. pylori in saliva (n = 8; 9.2%) and those who exhibited H. pylori in extracted teeth (n = 13; 14.9%) (Table 1); five subjects (5.7%) exhibited H. pylori in both saliva and extracted teeth. Among these specimens, six and one H. pylori-positive saliva specimens showed 1.0 × 102–1.0 × 103 CFU and 1.0 × 103–1.0 × 104 CFU of H. pylori, respectively. Only one H. pylori-positive saliva specimens included 1.0 × 104–1.0 × 105 CFU of H. pylori. In contrast, eight and five H. pylori-positive extracted teeth showed 1.0 × 102–1.0 × 103 CFU and 1.0 × 103–1.0 × 104 CFU of H. pylori, respectively. Mean age and height were similar among all groups, whereas the body weights and BMIs were higher in subjects with H. pylori in saliva, compared with all other groups. In addition, a greater proportion of subjects with H. pylori in saliva and/or extracted teeth were male, had a history of systemic diseases, and/or had a history of gastrointestinal diseases, compared with subjects without H. pylori. Furthermore, medical history and previous eradication of H. pylori from gastric tissue did not correlate with detection of H. pylori in the oral cavity.
In regard to dental caries status, the number of decayed teeth was higher in H. pylori-negative subjects, compared with H. pylori-positive subjects. In contrast, the numbers of missing teeth, filled teeth, and decayed, missing, or filled teeth (DMFT, combination of the three previous values) were higher in H. pylori-positive subjects (Table 2). The mean depth of the periodontal pocket around the extracted teeth (prior to extraction) was greater in subjects with H. pylori in saliva and in H. pylori-negative subjects, compared with subjects with H. pylori in extracted teeth.
Distribution of H. pylori in subjects with or without overweight BMI
BMI >25 kg/m2 was defined as overweight in the present study21. Subjects were classified into a non-overweight group (BMI <25 kg/m2; n = 74) and an overweight group (BMI >25 kg/m2; n = 13). In terms of H. pylori detection from saliva, the overweight group exhibited a significantly higher rate of detection than the non-overweight group (P < 0.05; Fig. 1A). A similar trend was observed regarding the rate of H. pylori detection in extracted teeth, although the statistical evidence was weak (Fig. 1B). In addition, a significant difference was observed in rates of H. pylori detection between extracted teeth and saliva (P < 0.05; Fig. 1C).
Distribution of H. pylori in relation to other clinical factors
Subjects were classified into two groups: those with digestive diseases in their clinical history (n = 16) and those without (n = 71). The group with a history of digestive diseases showed higher rates of H. pylori detection, compared with the group without a history of digestive diseases (Fig. 2A).
Comparison of the rates of H. pylori detection in oral specimens obtained from subjects with different clinical statuses. (A) The rates of H. pylori detection in subjects with or without digestive disease. (B) The rates of H. pylori detection in subjects with decayed, missing, or filled teeth (DMFT) values of <12.7 or >12.7. Rates of H. pylori detection are shown in centres of pie graphs.
Next, all subjects were divided into two groups based on the severity of dental caries status. The average DMFT for all subjects was 12.7; thus, we stratified subjects into a group with DMFT < 12.7 (low DMFT, n = 42) and a group with DMFT > 12.7 (high DMFT, n = 43) (Fig. 2B). Higher detection rates of H. pylori were observed in the high DMFT group, compared with the low DMFT group. We further stratified H. pylori detection rates based on periodontal pocket depths of the extracted teeth; subjects were divided into two groups as follows: subjects with periodontal pockets <4 mm (n = 37) and subjects with periodontal pockets >4 mm (n = 34) (Supplemental Fig. 1). Greater periodontal pocket depth did not correlate with a higher rate of H. pylori detection.
Distribution of H. pylori according to BMI and clinical history of digestive disease
Subjects were divided into four groups according to BMI and clinical history of digestive diseases, as follows: digestive disease-negative and non-overweight BMI (n = 61), digestive disease-negative and overweight BMI (n = 10), digestive disease-positive and non-overweight BMI (n = 12), and digestive disease-positive and overweight BMI (n = 4). Among all oral specimens, there were no significant differences in rates of H. pylori detection between overweight subjects with or without digestive disease (Fig. 3A–C). Overweight subjects without digestive disease showed significantly higher rates of H. pylori detection in saliva alone and in saliva and extracted teeth combined, compared with non-overweight subjects without digestive disease (P < 0.05).
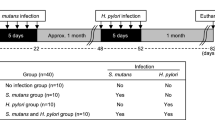
Distribution of H. pylori according to BMI and dental caries status
Subjects were divided into four groups according to BMI and number of DMFT, as follows: DMFT < 12.7 and non-overweight BMI (n = 37), DMFT < 12.7 and overweight BMI (n = 5), DMFT > 12.7 and non-overweight BMI (n = 34), and DMFT > 12.7 and overweight BMI (n = 9). Overweight subjects with high numbers of DMFT demonstrated the highest rates of H. pylori detection in all oral specimens (Fig. 4A–C); this rate was significantly higher than in non-overweight subjects with low numbers of DMFT (P < 0.05). Overweight subjects with high numbers of DMFT showed significantly higher rates of H. pylori detection in saliva alone and in saliva and extracted teeth combined, compared with non-overweight subjects with high numbers of DMFT (P < 0.05).
Detection of H. pylori in oral specimens obtained from overweight subjects, with or without high numbers of decayed, missing, or filled teeth (DMFT). Saliva (A), teeth (B) and saliva and teeth combined (C) were analysed. Significant differences were determined by using ANOVA with Bonferroni correction. *P < 0.05 and **P < 0.01 between two groups.
Discussion
The oral cavity has been recognized as a possible reservoir for H. pylori, and therefore might serve as a source of bacteria for gastric infection or transmission to others1. Prior epidemiological studies have reported an association between the presence of H. pylori in gastric tissues and the occurrence of digestive diseases and metabolic syndromes2,22. In addition, the effects of H. pylori from the oral cavity on the pathogenesis of digestive diseases have also been investigated23. However, there have been no studies regarding the relationship between H. pylori in the oral cavity and body weight. Notably, altered body weight has a relationship with various systemic diseases, especially digestive diseases and metabolic syndromes. To the best of our knowledge, this is the first study to demonstrate that the presence of H. pylori in the oral cavity is associated with overweight BMI.
Recently, oral bacteria were reported to be associated with various systemic diseases24. Moreover, significant associations between the presence of specific periodontal bacterial species and the occurrence of systemic diseases (e.g., diabetes, obesity, cardiovascular disease, and non-alcoholic fatty liver disease) have been reported15,16,17,25. H. pylori was originally classified in the Campylobacter genus, which contains multiple major periodontopathic bacteria2. Campylobacter rectus, a common Campylobacter species in the oral cavity, is associated with systemic diseases, such as low birth weight26; furthermore, C. rectus DNA has been detected within atheromatous plaque27,28. Therefore, it is reasonable to speculate that the presence of H. pylori in the oral cavity may be associated with the occurrence of overweight BMI, thereby acting as an exacerbating factor for subsequent systemic diseases.
Overweight and obese BMI (i.e., increased BMI) is considered a major risk factor for periodontal diseases, and the reverse association has also been reported29. In obese subjects, inflammatory cytokines are produced by adipose cells and secreted into the bloodstream30, resulting in immunodeficiency against infectious periodontal bacteria and subsequent destruction of periodontal tissue31. Moreover, bacterial profiles in saliva were altered in obese subjects, compared with those in healthy individuals32; the levels of some periodontopathic bacteria were significantly higher in obese subjects than in healthy individuals33. Although blood analyses were not performed in the present study, inflammatory cytokines secreted from adipose cells may also affect the detection of H. pylori in overweight subjects.
There were significant differences between overweight (28.6%) and non-overweight subjects (5.5%) with respect to the rates of H. pylori detection in saliva. The detection rate of H. pylori in overweight patients in the present study was also higher than the detection rate of H. pylori in saliva obtained from Japanese subjects without gastric diseases (6.4%; 21 of 326 subjects)6. However, no significant differences were observed in the rates of H. pylori detection in extracted teeth. These results indicate that the presence of H. pylori in saliva is related to the occurrence of overweight BMI.
In the present study, H. pylori ranges between 1.0 × 102–1.0 × 105 CFU/mL were observed in H. pylori-positive saliva specimens from overweight subjects. Daily production of saliva in a healthy person is approximately 0.5–1.5 L34. Therefore, approximately 5 × 104–1.5 × 108 CFUs of H. pylori may be present in secreted saliva each day. These bacteria could be swallowed and reach gastric tissue, thereby contributing to the occurrence of overweight BMI. Indeed, periodontal bacteria that were swallowed in saliva have been reported to induce systemic diseases, and some of these diseases exhibit altered gut microbial composition associated with obesity35. Although we only focused on H. pylori in the oral cavity in the present study, comparison of quantification data between H. pylori in the oral cavity and that in gastric tissue may be important for determining how many H. pylori in the oral cavity are related to the colonization of H. pylori in gastric tissue.
In our previous study, we sampled oral specimens from eight H. pylori-positive specimens in the first sampling9; seven of these eight specimens were H. pylori-positive in the second sampling. Furthermore, among twelve H. pylori-negative specimens in the first sampling, only one showed positive results in the second sampling. Based on these results, we concluded that H. pylori was not transiently present, but that it colonized the oral cavity for an extended period. However, in that study, the intervals between first and second samplings were short (approximately 1–2 weeks) and the sample sizes were quite low; moreover, that study did not focus on overweight subjects. Thus, further studies are needed to confirm whether H. pylori is transient, using oral samples taken from overweight subjects at two or three separate times.
Periodontal inflammation induced by periodontal bacteria in subjects with periodontitis causes inflammatory responses in systemic diseases36. In addition, higher levels of inflammatory cytokines have been detected in the periodontal pockets of subjects with periodontitis and obesity, compared with those of non-obese subjects37. In the present study, there was no correlation between periodontal pocket depth and the rates of H. pylori detection. Our results suggest that daily swallowing of H. pylori in saliva may be a major cause of overweight BMI, and that this BMI may not be related to the production of inflammatory cytokines associated with the presence of H. pylori in severe periodontitis.
When we analysed subjects without a clinical history of digestive diseases, the rate of H. pylori detection in overweight subjects was significantly higher than in non-overweight subjects. This indicates that a clinical history of digestive diseases may not be involved in the relationship between the presence of H. pylori in the oral cavity and overweight BMI. Thus, in some cases, oral H. pylori may be non-specifically involved in overweight BMI and related systemic diseases simply through its role as an oral bacterial species, in contrast to its role in the onset of digestive diseases induced in gastric tissue.
Dental caries may be a risk factor for infection by H. pylori in the oral cavity8,38, consistent with the present results. Among subjects with high numbers of DMFT, overweight subjects showed significantly higher rates of H. pylori detection, compared with non-overweight subjects. Although it remains unclear why dental caries and overweight BMI are risk factors for the presence of H. pylori in the oral cavity, daily dietary habits may be involved: excessive food intake, especially in terms of sugar, is associated with increased risks for dental caries and overweight BMI. Thus, other factors, such as dietary habits, should be analysed in future studies.
There are some limitations in the present study. First, this study enrolled a small number of subjects and none were defined as obese (BMI >30). Therefore, we focused on the detection of oral H. pylori in overweight subjects (BMI >25). In addition, the relationship between H. pylori infection in gastric tissue and the presence of H. pylori in the oral cavity was ambiguous, as few subjects reported a medical history of H. pylori infection in gastric tissue (n = 8) or previous eradication of H. pylori from gastric tissue (n = 4). Further studies should be performed with a larger number of samples; moreover, it may be more relevant to construct a collaborative study involving both dentists and gastroenterologists. Second, we revealed that detection of H. pylori in the oral cavity was associated with a high frequency of overweight BMI. Unfortunately, the present study did not demonstrate a mechanism by which oral H. pylori might contribute to the development of overweight BMI. It is possible that H. pylori in the oral cavity may induce overweight BMI in a similar manner to canonical periodontal bacteria. Therefore, we should perform confirmatory in vitro and in vivo experiments, similar to those previously used to show the mechanism by which obesity was induced by periodontal bacterial species18,39. Third, since this was a retrospective study with a limited number of subjects, prospective studies involving larger numbers of subjects should be performed to confirm our hypotheses.
In summary, detection of H. pylori in the oral cavity was associated with overweight BMI, especially in subjects with a severe dental caries status.
Methods
Ethics statement
This study was conducted in full adherence to the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Osaka University Graduate School of Dentistry (approval no. H23-E1-5). Prior to specimen collection, all subjects were informed of the study protocol and provided written informed consent.
Subjects and clinical data
Saliva and extracted teeth were obtained from 87 subjects (46 males and 41 females, age range: 20–83 years; median: 40 years; mean age: 45.3 ± 20.2 years) who were referred to the Department of Oral and Maxillofacial Surgery at Osaka University Dental Hospital from March 2016 to June 2017 due to dental problems requiring tooth extraction, such as dental caries and periodontitis. Approximately 1 mL of saliva or extracted teeth in 2.5 mL sterile saline were collected in sterile disposable tubes and used in the following study. The following information was collected from all subjects: height, weight, medical history, prior incidence of H. pylori infection in gastric tissue, and incidence of previous eradication of H. pylori from gastric tissue.
Evaluation of dental caries status
The dental caries status of all subjects was evaluated by a single dentist following visual inspection and findings from panoramic photographs. The clinical dental examination included the number of total teeth, decayed teeth, missing teeth and filled teeth. The numbers of DMFT were calculated as described previously40. In addition, probing depth in the deepest periodontal pocket of the extracted teeth was measured by using a round-ended probe before extraction.
Bacterial strains and growth condition
H. pylori reference strain J99 (ATCC 700824) was used as a positive control for nested PCR. J99 was cultured on blood agar plates (Becton Dickinson, Franklin Lakes, NJ, USA) at 37 °C for 3 days, as described previously8. Colonies were then inoculated in 5 mL tryptic soy broth (Difco Laboratories, Detroit, MI, USA), and incubated at 37 °C for 3–5 days under microaerophilic conditions.
Molecular biological analysis
Bacterial DNA was extracted from 1 mL saliva and extracted teeth in 2.5 mL sterile saline from each of the 87 subjects and resuspended in 100 μL distilled water, as described previously8. Then, nested PCR was performed on the bacterial DNA by using primer sets designed in our previous study9. Briefly, first-step PCR was performed with 1 μL bacterial DNA in reactions of 20 μL total volume by using primers ureA-aF (5′-ATG AAA CTC ACC CCA AAA GA-3′) and ureA-bR (5′-CCG AAA GTT TTT TCT CTG TCA AAG TCT A-3′). Second-step PCR was performed with 1 μL of the first PCR product as a template in reactions of 20 μL total volume by using primers ureA-bF (5′-AAA CGC AAA GAA AAA GGC ATT AA-3′) and ureA-aR (5′-TTC ACT TCA AAG AAA TGG AAG TGT GA-3′). The first and second-step PCR amplifications were performed by using the TaKaRa Ex Taq (Takara Bio. Inc., Otsu, Japan) with the following cycling parameters: an initial denaturation at 95 °C for 4 minutes and then 30 cycles of 95 °C for 30 seconds, 55 °C for 30 seconds, and 72 °C for 30 seconds; the final extension was performed at 72 °C for 7 minutes. All PCR products were checked by electrophoresis in a 1.5% agarose gel. The limit of H. pylori detection by nested PCR was 1–10 CFU9. Therefore, nested PCR could detect H. pylori at levels of more than 1.0 × 102–1.0 × 103 CFU in 1 mL saliva, or in the saline rinse of an extracted tooth. Based on the information from the previous analysis9, we performed nested PCR using serially diluted bacterial DNA, as in our previous studies9,41; this enabled determination of the approximate numbers of H. pylori in oral specimens.
Statistical analysis
Statistical analyses were performed by using the computational software package GraphPad Prism 6 (GraphPad Software Inc., La Jolla, CA, USA). Intergroup differences in each analysis were determined by using analysis of variance (ANOVA) with Bonferroni correction. A P value of < 0.05 was considered to be statistically significant.
Data Availability
The data are not available for public access because of patient privacy concerns, but are available from the corresponding author on reasonable request.
References
Prasanthi, C., Prasanthi, N., Manikiran, S. & Rao, N. R. Focus on current trends in the treatment of Helicobacter pylori infection: An update. Int J Phar Sci Rev Res 9, 42–51 (2011).
Fennerty, M. B. Helicobacter pylori. Arch Intern Med 154, 721–727 (1994).
Goodwin, C. S., Mendall, M. M. & Northfield, T. C. Helicobacter pylori infection. Lancet 349, 265–269 (1997).
Westblom, T. U. & Bhatt, B. D. Diagnosis of Helicobacter pylori. infection. Cur Top Microbiol Immunol 241, 215–235 (1999).
Urban, J., Koszowski, R., Plachetka, A. & Wiczkowski, A. An evaluation of selected oral health indicators and cariogenic bacteria titer in subjects with Helicobacter pylori. Adv Clinical Experimental Med 26, 401–407 (2017).
Suzuki, N. et al. Detection of Helicobacter pylori DNA in the saliva of patients complaining of halitosis. J Med Microbiol 57, 1553–1559 (2008).
Palmer, R. J. Jr. Composition and development of oral bacterial communities. Periodontol 2000 64, 20–39 (2014).
Ogaya, Y., Nomura, R., Watanabe, Y. & Nakano, K. Detection of Helicobacter pylori DNA in inflamed dental pulp specimens from Japanese children and adolescents. J Med Microbiol 64, 117–123 (2015).
Nomura, R., Ogaya, Y., Matayoshi, S., Morita, Y. & Nakano, K. Molecular and clinical analyses of Helicobacter pylori colonization in inflamed dental pulp. BMC Oral Health 18, 64 (2018).
Grundy, S. M., Brewer, H. B. Jr., Cleeman, J. I., Smith, S. C. Jr. & Lenfant, C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 109, 433–438 (2004).
Zukiewicz-Sobczak, W. et al. Obesity and poverty paradox in developed countries. Ann Agric Environ Med 21, 590–594 (2014).
Gunji, T. et al. Helicobacter pylori infection is significantly associated with metabolic syndrome in the Japanese population. Am J Gastroenterol 103, 3005–3010 (2008).
Shin, D. W. et al. Association between metabolic syndrome and Helicobacter pylori infection diagnosed by histologic status and serological status. J Clin Gastroenterol 46, 840–845 (2012).
Chen, T. P. et al. Helicobacter pylori infection is positively associated with metabolic syndrome in Taiwanese adults: a cross-sectional study. Helicobacter 20, 184–191 (2015).
Loesche, W. J. & Grossman, N. S. Periodontal disease as a specific, albeit chronic, infection: diagnosis and treatment. Clin Microbiol Rev 14, 727–752 (2001).
Genco, R. J., Grossi, S. G., Ho, A., Nishimura, F. & Murayama, Y. A proposed model linking inflammation to obesity, diabetes, and periodontal infections. J Periodontol 76, 2075–2084 (2005).
Yoneda, M. et al. Involvement of a periodontal pathogen, Porphyromonas gingivalis on the pathogenesis of non-alcoholic fatty liver disease. BMC Gastroenterol 12, 16 (2012).
Naka, S. et al. A specific Streptococcus mutans strain aggravates non-alcoholic fatty liver disease. Oral Dis 20, 700–706 (2014).
Naka, S. et al. Contributions of Streptococcus mutans Cnm and PA antigens to aggravation of non-alcoholic steatohepatitis in mice. Sci Rep 6, 36886 (2016).
Pataro, A. L. et al. Frequency of periodontal pathogens and Helicobacter pylori in the mouths and stomachs of obese individuals submitted to bariatric surgery: a cross-sectional study. J Appl Oral Sci 24, 229–238 (2016).
WHO Expert Constraction. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363, 157–163 (2004).
Vafaeimanesh, J. et al. Effect of Helicobacter pylori on metabolic syndrome parameters in diabetic subjects. Gastroenterol Hepatol Bed Bench 9, S36–S41 (2016).
Medina, M. L. et al. Molecular detection of Helicobacter pylori in oral samples from subjects suffering digestive pathologies. Med Oral Patol Oral Cir Bucal 15, e38–42 (2010).
Li, X., Kolltveit, K. M., Tronstad, L. & Olsen, I. Systemic diseases caused by oral infection. Clin Microbiol Rev 13, 547–558 (2000).
Beck, J., Garcia, R., Heiss, G., Vokonas, P. S. & Offenbacher, S. Periodontal disease and cardiovascular disease. J Periodontol 67, 1123–1137 (1996).
Arce, R. M., Caron, K. M., Barros, S. P. & Offenbacher, S. Toll-like receptor 4 mediates intrauterine growth restriction after systemic Campylobacter rectus infection in mice. Mol Oral Microbiol 27, 373–381 (2012).
Okuda, K., Kato, T. & Ishihara, K. Involvement of periodontopathic biofilm in vascular diseases. Oral Dis 10, 5–12 (2004).
Nakano, K. et al. Detection of cariogenic Streptococcus mutans in extirpated heart valve and atheromatous plaque specimens. J Clin Microbiol 44, 3313–3317 (2006).
Dahiya, P., Kamal, R. & Gupta, R. Obesity, periodontal and general health: Relationship and management. Indian J Endocrinol Metab 16, 88–93 (2012).
Wisse, B. E. The inflammatory syndrome: the role of adipose tissue cytokines in metabolic disorders linked to obesity. J Am Soc Nephrol 15, 2792–2800 (2004).
Suvan, J. E. et al. Association between overweight/obesity and increased risk of periodontitis. J Clinical Periodontol 42, 733–739 (2015).
Goodson, J. M., Groppo, D., Halem, S. & Carpino, E. Is obesity an oral bacterial disease? J Dent Res 88, 519–523 (2009).
Al-Rawi, N. & Al-Marzooq, F. The relation between periodontopathogenic bacterial levels and resistin in the saliva of obese type 2 diabetic subjects. J Diabetes Res 2017, 2643079 (2017).
Iorgulescu, G. Saliva between normal and pathological. Important factors in determining systemic and oral health. J Med Life 2, 303–307 (2009).
Arimatsu, K. et al. Oral pathobiont induces systemic inflammation and metabolic changes associated with alteration of gut microbiota. Sci Rep 4, 4828 (2014).
Kim, J. & Amar, S. Periodontal disease and systemic conditions: a bidirectional relationship. Odontology 94, 10–21 (2006).
Akram, Z., Abduljabbar, T., Abu Hassan, M. I., Javed, F. & Vohra, F. Cytokine profile in chronic periodontitis subjects with and without obesity: A systematic review and meta-analysis. Dis Markers 2016, 4801418 (2016).
Liu, Y. et al. Study on the relationship between Helicobacter pylori in the dental plaque and the occurrence of dental caries or oral hygiene index. Helicobacter 13, 256–260 (2008).
Amar, S. & Leeman, S. Periodontal innate immune mechanisms relevant to obesity. Mol Oral Microbiol 28, 331–341 (2013).
Blinkhorn, A. S. & Davies, R. M. Caries prevention. A continued need worldwide. Int Dent J 46, 119–125 (1996).
Shirai et al. Short communication: Distribution of Porphyromonas gulae fimA genotypes in oral specimens from dogs with mitral regurgitation. Res Vet Sci 102, 49–52 (2015).
Acknowledgements
The authors thank Prof. Howard K. Kuramitsu, State University of New York at Buffalo, for editing the manuscript. We also thank Ms. Rewa Yanagisawa, WDB Co., Ltd., for technical support with molecular analyses. This work was supported by JSPS KAKENHI Grant Number JP15H05049 and JP18K17252.
Author information
Authors and Affiliations
Contributions
M.H. and R.N. designed the entire study under the supervision of N.U. and K.N. M.H. collected clinical samples; R.N., Y.O., S.M., T.K. and Y.M. performed the experiments. Data interpretation was conducted by M.H., R.N., and K.N. M.H., R.N. and K.N. wrote the manuscript, which all authors read and approved.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hamada, M., Nomura, R., Ogaya, Y. et al. Potential involvement of Helicobacter pylori from oral specimens in overweight body-mass index. Sci Rep 9, 4845 (2019). https://doi.org/10.1038/s41598-019-41166-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-41166-5
This article is cited by
-
The Associations between Helicobacter Pylori immunoglobulin G seropositivity and body mass index in adults
BMC Infectious Diseases (2023)
-
Distribution of periodontopathic bacterial species between saliva and tonsils
Odontology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.