Abstract
Intracellular pathogenic microorganisms and toxins exploit host cell mechanisms to enter, exert their deleterious effects as well as hijack host nutrition for their development. A potential approach to treat multiple pathogen infections and that should not induce drug resistance is the use of small molecules that target host components. We identified the compound 1-adamantyl (5-bromo-2-methoxybenzyl) amine (ABMA) from a cell-based high throughput screening for its capacity to protect human cells and mice against ricin toxin without toxicity. This compound efficiently protects cells against various toxins and pathogens including viruses, intracellular bacteria and parasite. ABMA provokes Rab7-positive late endosomal compartment accumulation in mammalian cells without affecting other organelles (early endosomes, lysosomes, the Golgi apparatus, the endoplasmic reticulum or the nucleus). As the mechanism of action of ABMA is restricted to host-endosomal compartments, it reduces cell infection by pathogens that depend on this pathway to invade cells. ABMA may represent a novel class of broad-spectrum compounds with therapeutic potential against diverse severe infectious diseases.
Similar content being viewed by others
Introduction
There is a growing need for broad-spectrum drugs to fight existing and emerging infectious diseases (EID) and to be prepared for potential bioterror attacks with toxins or microorganism1. Each new EID crisis reveals our level of unpreparedness that is due to the difficulty to predict which pathogen will emerge and to the impossibility to develop new drugs within a few months. A strategy for broad-spectrum drug discovery is the search for molecules targeting host components indispensible for entry and/or multiplication of many different toxins and pathogens into cells1,2,3,4,5,6. Such drugs may have efficacy against unknown pathogens that will emerge in the future. Moreover, molecules active against host cell components should avoid the risk of drug-resistant pathogens7.
Plant and bacterial protein toxins acting inside cells, as well as intracellular infectious pathogens such as viruses, intracellular bacteria and parasites have evolved sophisticated strategies to invade host cells that share common features8,9,10,11,12. They bind to cell-surface receptors to trigger their internalization. Then, they follow endocytic and intracellular trafficking pathways. Toxins, viruses and sometimes bacteria enter the cell cytosol from specific trafficking compartments8,9,11. Other bacteria and intracellular parasites may subvert cell compartments and trafficking components to build a comfortable vacuoles in which nutrients conducive for multiplication are found10,12. Thus, small molecules targeting intracellular trafficking pathways (e.g Retro-21,13,14 and EGA2,15,16,17) or host component (e.g amodiaquine3, bithionol4) exploited by infectious agents exhibit broad anti-infectious actions.
Here, we report the discovery of ABMA, a novel broad-spectrum inhibitor of intracellular toxins and pathogens. ABMA was identified using a cell-based high throughput screen (HTS) against cell intoxication by the plant toxin ricin14. ABMA protected mice from nasal instillation of an LD90 of ricin. Besides, ABMA protected cells from intoxication by at least four bacterial toxins and from infection by three viruses, two intracellular bacteria and one parasite. In addition, the molecule was not toxic to cells or mice at active concentrations. We further showed that the broad-spectrum anti-pathogenic action of ABMA is associated with the biogenesis of host cells’ late endosomes (LE) without affecting other organelle integrity. Hence, ABMA has the potential to inhibit any toxin or infectious pathogen relying on LE to enter the cytosol or build its intracellular vacuole.
Results
Identification by HTS of ABMA, a ricin inhibitor active in vitro and in vivo
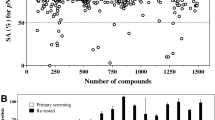
As previously described14, we performed a cell-based HTS to identify small chemical compounds active against ricin-mediated cell intoxication. We screened a library of 16,500 small molecules for those endowed with the capacity to prevent the inhibition of protein biosynthesis induced by ricin treatment. Four hits were confirmed; two hits named Retro-1 and Retro-2 were reported as inhibitors of ricin and Shiga-like toxins (Stx) by blocking their retrograde transport inside host cells14. ChemBridgeTM compound 1-Adamantyl (5-Bromo-2-Methoxybenzyl) Amine (ABMA, Fig. 1A) discussed in this article, was one of the other hits from that screen, which bears a hydrophobic adamantane and a substituted aromatic moiety.
Hit compound ABMA identified as an inhibitor of ricin by HTS. (A) Chemical structure of ABMA. (B) Intoxication of pulmonary A549 cells by increasing concentrations of ricin in the presence of 3, 10 and 30 µM of ABMA. A549 cells were incubated 4 h in DMEM with ABMA (open and half-filled circles), or solvent only as control (DMSO, black circles) before addition of increasing concentrations of ricin for 20 h. Media was removed and replaced with DMEM containing [14C]-leucine at 0.5 µCi/mL for 6 h. Protein synthesis was measured by scintillation counting as the amount of [14C]-leucine incorporated in cells. Each data point represents the mean of duplicate ± SD of a representative experiment. (C) ABMA protects mice against ricin challenge. The survival of mice treated once with the indicated doses of ABMA and then exposed to an LD90 of ricin via nasal instillation was monitored. In each experiment, treated animals received a single ip dose of ABMA (2 mg/kg, open circles; 20 mg/kg, circles with right half black; and 200 mg/kg, circles with left half black) 1 h prior to toxin exposure (2 µg/kg by nasal instillation), while control animals (black circles) received vehicle only prior to ricin administration. The curves for treated animals are statistically different from control as measured by the log rank test (p < 0.01 for 2 mg/kg of ABMA; p < 0.001 for 20 mg/kg,; p < 0.001 for 200 mg/kg).
Inhalation is considered as a major risk factor for ricin exposure18. Thus, ABMA protective activity was first tested in vitro by challenging human pulmonary alveolar basal epithelial A549 cells with increasing concentrations of ricin (Fig. 1B). In five independent experiments, ABMA treatment induced a decrease in ricin cytotoxicity with an EC50 of 3.8 µM, and a protection factor (R) at 30 µM ranging from 5 to 10. ABMA retained almost 100% of its biological activity against ricin-induced cytotoxicity up to six days after incubation in culture medium at 37 °C (Fig. S1), indicating a robust stability. As expected, ABMA had no observed inhibitory effect on cell protein synthesis up to at least 90 µM as measured by [14C]-leucine incorporation (Fig. S2). AlamarBlue® cell viability assay also confirmed its low toxicity on human cells, with a CC50 (50% cytotoxicity concentration) on cultured (HeLa) and primary human cells (Human Umbilical Vein Endothelial Cells, HUVECs) at more than 200 μM (Fig. S3).
Based on these in vitro results, we investigated whether ABMA could protect mice against a lethal ricin challenge. ABMA was non-toxic to animals after one intra-peritoneal (ip) administration up to 200 mg/kg. A model of ricin intoxication by nasal instillation14 was used to mimic exposure by aerosols, as would occur during an intentional release. Briefly, mice were challenged by an LD90 of ricin (2 μg/kg) at day 0 (Fig. 1C, closed circles). The first clinical signs of intoxication appeared within 24 h, all mice displaying bristly and greasy hairs. From day 2, weight loss was observed. At later time points other signs were noticed such as prostration, shaking and respiratory distress, with animals needing to be euthanized starting from day 7 post exposure. A statistically significant protection according to survival curves was observed with a single ip dose of 2 mg/kg of ABMA 1 h prior toxin challenge (p < 0.01 versus control, Fig. 1C, open circles). Forty eight % (n = 25; 3 independent experiments) of ABMA-treated mice survived, while in the control group, survival was 11.5% (n = 130, from 10 independent experiments). Based on this result, additional experiments were performed with escalating doses of ABMA. Administration of a single ip dose of 20 mg/kg and 200 mg/kg of ABMA prior to ricin intoxication gave improved, statistically significant, levels of protection as compared to the control group (p < 0.001, n = 5 for both groups). The 20 mg/kg dose fully protected animals through to day 21 (Fig. 1C). The 200 mg/kg dose resulted in 80% of protection of mice against ricin challenge with a single animal succumbing on day 15. The lower protection seen with the higher dose may be due to solubility issues of ABMA in aqueous solution resulting in uncertain biodistribution at the highest dose.
ABMA, a broad-spectrum inhibitor active in vitro against various bacterial toxins
The mechanism of action of ricin toxin shares common general principles with those of intracellular-acting bacterial protein toxins: binding to a cell-surface receptor, internalization in endocytic compartments, trafficking through intracellular transport pathways, translocation from transport vesicles or compartments into the cytosol and catalytic modification of a cellular target. Thus, investigating the effect of ABMA on bacterial toxins may lead to identify other sensitive toxins and hence, get some insights into ABMA mechanism of action4,5. Table S1 summarizes the features of the tested toxins.
Appropriate model cell lines were pretreated with solvent alone (DMSO) or various concentrations of ABMA, then respectively incubated with increasing concentrations of diphtheria toxin from Corynebacterium diphtheriae (DT), lethal toxin from Bacillus anthracis (LT), toxin B from Clostridium difficile (TcdB), lethal toxin from Clostridium sordellii (TcsL), Shiga-like toxin 2 from Escherichia coli (Stx2) or Botulinum neurotoxin A (BoNT/A) from Clostridium botulinum (Table S1 and Fig. 2). The inhibitory effect of DT on protein biosynthesis was measured by the incorporation of [14C]-leucine into newly synthesized proteins. We observed higher levels of protein biosynthesis on A549 cells exposed to DT in the presence of ABMA than in its absence (Fig. 2A) with an EC50 of 62.5 ± 0.3 µM (n = 3). At 90 µM of ABMA, DT toxicity was reduced more than 100-fold in the assay conditions. We also found that ABMA protected other cell lines (e.g. Vero, PC3, A431 and DLD1) as well as HUVEC primary cells against DT (data not shown). This indicates that the inhibitory effect of ABMA on DT is not cell type-specific. Anthrax LT cleaves the mitogen-activated protein kinase MEK219. Figure 2B shows that MEK2 cleavage by LT in HUVECs was partially inhibited in the presence of ABMA at 30 µM. TcdB and TcsL inactivate small GTPases by their glucosyltransferase activity. This disrupts the actin cytoskeleton and induces cell rounding20. ABMA reduced Vero cells rounding 4 and 8 folds, respectively, following a challenge by TcdB for 4 h and by TcsL for 18 h (Fig. 2C,D). The EC50s were 73.3 ± 9.1 µM for TcdB and 86.7 ± 6.8 µM for TcsL (n = 3).
ABMA inhibits cytotoxicity of several bacterial toxins. Cells were incubated with the indicated concentrations of ABMA and then challenged with increasing concentrations of the indicated toxins. (A) A549 cells were exposed to DT for 18 h. Culture media was removed and replaced with DMEM containing [14C]-leucine at 0.5 µCi/mL for 3 h before protein biosynthesis determination. (B) Immunoblots showing the levels of MEK2 in HUVEC cells left untreated (line 1) or treated with Anthrax LT (lines 2–3, LT = PA 3 µg/mL + LF 1 µg/mL) in the absence and presence of 30 µM of ABMA. Immmunoblot of anti-actin show equal protein loading. (C,D) Vero cells were intoxicated with TcdB for 4 h or TcsL for 18 h and morphological changes of intoxicated cells were imaged and analyzed. (E) HeLa cells were exposed to Stx2 for 16 h before protein biosynthesis determination as for DT. (F) ABMA or DMSO were added to rat cerebellar granule neurons (CGNs) 1 h prior to BoNT/A exposure (500 pM) in the presence of compounds for 24 h. Immunoblots showing the levels of SNAP-25 and its cleaved form in the absence and presence of ABMA. Immunoblots images from single experiment (B and E) were spliced to rearrange the order of samples. Full-length blots are presented in Supplementary Figure S8.
Stx2 blocks cell protein biosynthesis by cleaving adenine 4324 of the 28 S ribosomal RNA with the same N-adenine glycohydrolase activity as ricin14. ABMA at 30 and 60 µM had barely any protective effect on intoxication of HeLa cells by Stx2 and a very weak protection at 90 µM (Fig. 2E). Botulinum neurotoxin A (BoNT/A) cleaves the SNARE protein SNAP25 that is essential for the fusion of neuromediator vesicles to the presynaptic membrane of nerve termini, inducing paralysis of the neuromuscular junction21. Figure 2F shows that ABMA at 30 µM was unable to prevent SNAP25 cleavage by BoNT/A in rat cerebellar granule primary cultured neurons, a model for BoNT/A activity.
Taken together, our results show that ABMA had no effect against Stx2 and BoNT/A cell intoxication. Nevertheless, it displays a broad-spectrum antitoxin activity against potent plant and bacterial toxins acting inside cells: ricin, DT, LT, TcdB and TcsL.
Various steps of the toxins’ mechanism of action may be considered as the target of ABMA: receptor binding, internalization, intracellular trafficking, translocation into the cell cytosol and catalytic modification of a cell substrate. The toxins sensitive to ABMA have different catalytic activities: N-adenine glycohydrolase for ricin and Stx2, ADP-ribosyltransferase for DT, Zn2+ metalloprotease for anthrax LT and BoNT/A and glucosyltransferase for TcdB and TcsL. Thus, it is very unlikely that ABMA inhibits the toxins’ catalytic activities. Each of those toxins uses a different cell-surface component as a receptor for cell binding and internalization (see Table S1). Thus, ABMA probably doesn’t inhibit the binding of the toxins to their receptors. Nevertheless, we investigated whether ABMA could inhibit the binding of DT receptor binding domain, named DTR822, to its receptor pro-HB-EGF (Precursor of heparin binding epidermal growth factor analog) as a model for toxin-receptor interaction23. A fluorescent DTR8 was made by chemical coupling with Alexa488 (DTRA488). FACS analysis showed that ABMA did not affect binding of Alexa488 labeled-DTR8 (DTRA488) with its receptor on Vero cells (Fig. S4), suggests that the inhibition of DT cytotoxicity induced by ABMA is not due to a reduced binding of DT to its receptor.
Since ABMA can inhibit several toxins with different catalytic activities and different receptors, we hypothesized that the inhibitor is not acting directly on the toxin itself but rather on a common host target, necessary for the toxins to reach the host cell’s cytosol and exert their toxicity. Our results demonstrate that ABMA has a pronounced inhibitory effect on DT, LT, TcdB and TcsL, which are all well-characterized acidic endosome-dependent toxins. They require low-pH endosomes (early endosomes (EE) and LE) where they undergo a conformational change, leading to the interaction of their transmembrane and catalytic domains with the compartments’ membrane and translocation of their catalytic domain into the cytosol8. In contrast, ABMA had barely any protective effect on the intoxication of HeLa cells by Stx2. Stx2 follows exclusively the retrograde route from the EE to the endoplasmic reticulum (ER) via the Golgi apparatus after internalization into cells8. Finally, ABMA is not able to inhibit BoNT/A, which relies on peculiar synaptic vesicle recycling and endocytosis processes to enter into neurons24,25. Thus, we hypothesized that ABMA is targeting host’s endosomal trafficking pathway between EE and the lysosomes.
ABMA inhibits cell infection by viruses that enter the host cytosol from acidified endosomes
Knowing that ABMA protects cells from multiple toxins that rely on acidic endosomes to translocate into the cytosol, we investigated whether ABMA was able to inhibit cell infection by viruses that have a pH-dependent mechanism of capsid release from these compartments. We tested Ebola virus (EBOV), Rabies virus (RABV), Dengue-4 virus (DENV4) and Chikungunya virus (CHIKV) (Table S2), which bear a surface glycoprotein that mediates fusion of the virus membrane with that of the endosome after which the capsid is released to the cell cytosol to initiate infection26. HeLa cells were incubated 1 h with increasing concentrations of ABMA before infection with a recombinant EBOV Mayinga strain carrying an enhanced green fluorescent protein (eGFP). ABMA treatment inhibited EBOV-eGFP infection with an EC50 of 3.3 µM (Fig. 3A). Baby hamster kidney (BSR) cells were incubated 4 h with ABMA before infection with the Pasteur vaccins/PV strain of RABV, ABMA inhibited the infection with an EC50 of 19.4 µM (Fig. 3B). Ribavirin, an antiviral drug inhibiting viral RNA synthesis and viral mRNA capping was used as a reference molecule and exhibited a similar EC50. Finally, Vero cells were incubated 1 h with ABMA before infection with DENV4, ABMA inhibited infection with an EC50 of 8.2 µM, while Ribavirin was about four fold less efficient in protecting cells from the infection (Fig. 3C). ABMA reduced cell infection by the three viruses up to at least 90% at 20 µM for EBOV and DENV4 and at 100 µM for RABV. In contrast, ABMA up to 100 µM did not inhibit infection of HEK293 cells by Chikungunya virus (CHIKV) (Fig. S5, see discussion section). In summary, we observed that ABMA inhibited three endosomal acidification–dependent viruses.
ABMA inhibits EBOV, RABV and DENV4. (A) HeLa cells were pre-incubated with increasing concentrations of ABMA solubilized in DMSO, or DMSO only, for 1 h and then challenged with EBOV-eGFP in the presence of the drug for 24 h. Cells were fixed, stained with DAPI, and numbers of nuclei and eGFP-positive (infected) cells were counted using the CellProfiler software. The relative infection efficiencies were calculated by dividing the number of infected cells by the number of nuclei. The percentages of infected cells in DMSO- and ABMA-treated samples were reported relative to the infection efficiency in non-treated cell. Data are representative of three independent experiments. (B) BSR cells were pretreated for 4 h with increasing concentrations of ABMA or ribavirin solubilized in DMSO, then challenged with the PV strain of RABV (MOI = 14) for 1 h. Cells were washed to remove the non-fixed virus, then incubated again in the presence of the same concentrations of the compounds for 24 h. Cells were fixed, nuclei were stained with Hoechst and infected cells were detected by immunostaining of the RABV ribonucleocapsid. RABV-positive cells were counted and their number was reported to that of non-treated cell, allowing calculating a percentage of inhibition. The average of three independent experiments and standard deviations are shown. (C) Vero cells were treated with ABMA or ribavirin solubilized in DMSO and then challenged with 125 TCID50 of a DENV4 serotype virus for 7 days. Viral replication was detected by ELISA using specific serum from DENV4-infected non-human primate.
ABMA inhibits cell infection by Simkania negevensis and Chlamydia trachomatis
Simkaniaceae and Chlamydiaceae from the order Chlamydiales are obligate intracellular Gram-negative pathogenic bacteria. They use host-cell materials to form a distinct, degradation-resistant but replication-permissive membranous compartment, the vacuole or inclusion. Despite differences, their intracellular life-styles share several common features. Proteomic characterization of the Simkania negevensis (Sn) containing vacuole (SnCV) has shown that it contains proteins from several main host transport pathways including the endosomal pathway13. Chlamydia trachomatis (Ctr) recruits multiple Rab proteins from the endosomes to the inclusion membrane and avoids travelling to the phago-lysosome as a final destination27. Besides the Golgi apparatus, multi-vesicular bodies (MVBs), also known as LE, are another essential source of cholesterol and sphingomyelin for the development of Ctr inclusions28,29. Thus, we tested whether ABMA could inhibit the infection of cells by Sn and Ctr.
Figure 4A shows that 75 µM of ABMA sharply reduced the amount of Sn in infected cells as revealed by immunoblotting of Sn heat-shock protein 60 (snHSP60). In parallel, inclusion sizes were smaller as revealed by immunofluorescence (Fig. 4B). The Sn progeny harvested from ABMA-treated cells reduced the amount of Sn (Fig. 4C) and the number of inclusions upon infection of fresh, untreated cells (Fig. 4D,E). ABMA at 75 µM slightly reduced the cellular load of GFP-expressing Ctr strain in the primary infection as seen by Ctr HSP60 (ctrHSP60) immunoblotting (Fig. 5A). However, ABMA treatment dramatically reduced chlamydial progeny infectivity indicated by the reduced inclusion number and bacterial load (Fig. 5A,B). Together, our results show that ABMA inhibits the capacity of Sn and Ctr to develop properly during cell infection and leads to a progeny with reduced infectivity.
Effects of ABMA on SnCV during Sn infection. HeLa 229 cells were infected with Sn (MOI = 0.5) for 3 days in the presence of ABMA or DMSO control at the indicated concentrations. Bacterial were released and transferred to infect fresh cells for 3 days in the absence of compounds. (A) Effect of ABMA on the Sn bacterial load of infected cells measured by snHSP60 immunoblot. Actin was used as loading control. (B) Effect of ABMA on the inclusion sizes of Sn during primary infection. Relative Sn incusion sizes were determined via snHSP60 immunostaining and quantitative analysis using ImageJ. (C) Effect of ABMA on the Sn bacterial load of progeny infected HeLa cells measured by snHSP60 immunoblot. Actin was used as loading control. (D) Effect of ABMA on the number of Sn inclusions during progeny infection. (E) Immunofluorescence images of cells infected by Sn progeny from cells treated with 75 µM ABMA after 3 days of incubation. Nuclei were stained for DAPI (green) and SnCVs were stained for HSP60 (red). Images are representative of 3 independent experiments. Full-length blots (A and C) are presented in Supplementary Figure S9.
Effects of ABMA on Ctr primary and progeny infections. HeLa 229 cells were pretreated with ABMA or DMSO control at the indicated concentrations for 1 hour prior to infection with Ctr (MOI = 1). Cells were lysed 48 h post infection and lysates were used to infect fresh cells. ABMA was present during primary infection. (A) Immunoblotting analysis of lysed HeLa 229 cells after Ctr primary and progeny infections following ABMA treatment during the primary infection. Bacterial load was detected with antibodies against ctrHSP60 protein and actin was used as a loading control. (B) Immunofluorescence analysis of infectivity with 75 µM ABMA treatment during primary infection. 24 h post progeny infection; cells were fixed and stained for DAPI (blue). Ctr inclusions were detected by their GFP-expression signal (green). Immunoblots image (A) were spliced to rearrange the order of samples. Full-length blots are presented in Supplementary Figure S10.
ABMA inhibits the development of Leishmania infantum in macrophages
Monocytes and macrophages are important target cells in the pathophysiology of Leishmania parasite infections30. The parasite is internalized and develops into an amastigote form within a parasitophorous vacuole that incorporates endo-lysosomal pathway components30,31. Thus, we investigated whether ABMA could inhibit the infection of RAW 264.7 macrophages by Leishmania infantum amastigotes. Amphotericin B and miltefosine, which are approved drugs for the clinical management of Leishmaniasis, were used as reference drugs. Table 1 shows that all three drugs inhibited L. infantum intramacrophage amastigotes development with various EC50s. The EC50 for ABMA was around 7 µM. Interestingly, the two reference drugs were capable of inhibiting axenic amastigotes with an efficacy similar to that found on intramacrophage amastigotes, whereas ABMA had no direct effect on the axenic parasite, up to 100 µM. In addition, the ABMA cytoxicity was lower than those of the reference drugs. These results strongly suggest that ABMA blocks L. infantum intracellular development by an action on host cell while the other drugs are directly toxic to the parasite.
ABMA induces accumulation of late endocytic compartments
We have determined that ABMA can inhibit the intoxication or infection of cells by a variety of toxins, viruses and intracellular microorganisms. The toxins and the viruses rely on endosome acidification to enter the cytosol. The bacteria and parasite build a vacuole that incorporates endosome membranes and proteins to acquire their nutrients and proliferate. This may suggest that ABMA targets and modifies acidic endosomes and their homeostasis. We observed by confocal microscopy that live A549 cells treated with ABMA and stained by LysoTracker® Deep Red exhibited more intensely labeled and enlarged fluorescent puncta than cells treated with DMSO only (Fig. 6A, middle and left panels respectively). In contrast, bafilomycin A1 (Baf A1), a highly specific v-ATPase inhibitor that prevents endosome acidification, decreased fluorescence staining of cells (Fig. 6A, right panel). We obtained similar results with ABMA and Baf A1 on HeLa and RAW 264.7 cells (data not shown). To confirm that ABMA is affecting acidic endosomes, we used acridine orange, another cell-permeant dye for acidic organelles (Fig. 6A, central and lower panels). Similarly, ABMA induced larger and brighter red fluorescent vesicles in A549 cells, in contrast to the effect of Baf A1, which strongly decreased red fluorescence in cytoplasmic vesicles. Altogether, ABMA had an effect on acidic compartments different from that of Baf A1. Baf A1 is known to inhibit DT toxicity by inhibiting endosome acidification. It might be expected that combined effect of both molecules might annihilate the impact of each other: increased endosome acidification for ABMA versus decreased acidification for BafA1. Surprisingly, ABMA combined with Baf A1 had an inhibitory effect on DT cytotoxicity twenty fold higher than for each molecule alone (Fig. S6). This strongly suggests that ABMA and Baf A1 have different mechanisms of action and distinct targets. Moreover, this indicates that the anti-toxin and anti-pathogenic effect of ABMA is not linked to the increase in endosome acidification; otherwise it would be counter balanced by Baf A1.
ABMA induces the accumulation of late endocytic compartments and affects cholesterol transport. (A) LysoTracker® Deep Red (50 nM, 30 min), acridine orange (10 µg/mL, 10 min) staining of A549 cells pretreated with DMSO or ABMA at 60 µM for 2 h. BafA1 at 100 nM was used as a control. (B) DMSO or ABMA 24 h-treated A549 cells were fixed, permeabilized by 0.1% Saponin and stained with antibodies against EEA1, Rab7 or Lamp1. Arrows indicate larger Rab7-positive vesicles. (C) A549 and HeLa cells were treated respectively with ABMA (30 µM), U18666A (10 µg/mL) or DMSO for 18 h, then fixed and stained with the cholesterol-avid fluorophore Filipin III. Nuclei were stained with Hoechst 33342 (blue).
To further characterize the effect of ABMA on intracellular acidic compartments, immunostaining of protein markers of the EE to lysosomes pathway were performed on A549 cells. Immunostaining of EEA1 (EE marker, Fig. 6B upper panel) and Lamp1 (lysosome marker, Fig. 6B lower panel) were unchanged in ABMA-treated cells and vehicle alone, while Rab7 (LE marker, important GTPase in the late endocytic pathway) staining was visibly enhanced in ABMA-treated cells compared to vehicle alone (Fig. 6B, central panel). Importantly, we did not observe morphological changes on other important cellular organelles such as the Golgi apparatus or ER (stained for Trans-Golgi Network 46 (TGN 46) and Protein disulfide isomerase (PDI), respectively; Fig. S7) as well as endocytosis-related membrane protein (clathrin, adaptin-α, epsin I; data not shown). Altogether, the data show that ABMA targets late endosomal compartments, without affecting the morphology of other organelles: EE, Golgi apparatus, ER and lysosomes.
Besides EE, LE is considered as important and complex sorting stations for proteins and lipids in the endocytic pathway. Cholesteryl esters in LE/Lysosomes are hydrolyzed by lysosomal acid lipase to free cholesterol, before egress from the endo-lysosomal system, allowing for its distribution to other cellular compartments32. We investigated if LE modified by ABMA is consequently accompanied by alterations of cholesterol transport, which may potentially interfere with nutrition of intracellular pathogens12. Filipin III, a fluorescent probe with high affinity for cholesterol was applied to cells treated respectively with DMSO, ABMA and U18666A, an intracellular cholesterol transport inhibitor. Both ABMA and U18666A induced an accumulation of cholesterol inside A549 and HeLa cells as observed by fluorescent microscopy (Fig. 6C). Together, these data show that ABMA affects LE and induces cholesterol accumulation, likely within late endosomal compartments.
The enhanced LysoTracker acidification dye and Rab7 staining led us to further investigate how ABMA affects the number and morphology of LE. We used transmission electron microscopy to examine the ultrastructure morphology of organelles in both DMSO- and ABMA-treated A549 cells. We observed that ABMA induced the accumulation of compartments with a >200 nm size, containing a variable number of smaller intraluminal vesicles (ILVs) but lacking a multilamellar morphology (Fig. 7D–F). These structures are characteristic of multivesicular bodies/LE (MVBs/LE)33. Other organelles appearing as electron-dense multi-lamellar membrane compartments characteristic of lysosomes were visualized in both DMSO- and ABMA-treated cells without observed difference in amount and morphology (Fig. 7). Altogether, the results show that ABMA induces the accumulation of MVBs/LE.
ABMA induces MVBs/LE accumulation. DMSO (A and B) or ABMA (D and E) 24 h-treated A549 cells were processed for electron microscopy and representative electron micrographs of sections are shown. Endocytic compartments are marked as follows: MVBs/LE (arrowheads), lysosomes (arrows). Enlarged figures from B and E show representative lysosomes (C) and MVBs/LE (F).
Discussion
Here we report that the small molecule ABMA, originated from a cell-based HTS assay to identify ricin inhibitors14, protects cells from a wide range of bacterial toxins, viruses and intracellular micro-organisms including bacteria and parasite. The efficacy of ABMA is variable according to the pathogens and toxins investigated. EC50 values varied from 60 to 90 µM in the bacterial toxin assays and down to ~7 µM against intra-macrophagic L. infantum amastigotes or ~ 3 µM against Ebola virus and ricin toxin. However, another key parameter must be taken into account to evaluate efficacy: the level of reduction of intoxication or infection for a given pathogen. For instance, DT toxicity was reduced more than two logs by ABMA; cell infection was decreased below 10% for RABV and down to 0 for EBOV and DENV4. The capacity of Ctr progeny to infect new cells was practically abolished by 75 µM of ABMA. All these agents and the corresponding cell assays to measure the compound efficacy are very different, which make comparison difficult. Finally, the ricin in vivo assay demonstrates that an inhibitor with a limited efficacy in vitro (5 to 10-fold reduction of ricin toxicity) can be enough to protect mice against a lethal toxin challenge. These findings suggest that ABMA may impair Ebola infection in mice, considering its lowest EC50 on Ebola among all tested pathogens and toxins in vitro.
Several broad-spectrum anti-pathogen compounds have recently been identified from cell-based HTS. They all have direct actions on host cells instead of on the pathogen itself, at µM level1,2,3,4,5. Amodiaquine, a clinically approved drug to treat malaria, protects cells against multiple toxins (anthrax lethal toxin, DT, TcdB) and viruses (Ebola, SARS coronavirus, Rabies, Chikungunya) by inhibiting host cathepsin B3. Bithionol, an anthelmintic approved drug, inhibits host caspases and also reduces the toxicity of anthrax lethal toxin, DT, cholera toxin, Pseudomonas aeruginosa exotoxin A, botulinum neurotoxin, ricin, and Zika virus4. EGA, an active molecule against anthrax lethal toxin also blocks in vitro trafficking of various toxins (DT, exotoxin A, cytolethal distending toxin, Botulinum Neurotoxins, Clostridium toxins) and viruses (influenza virus and lymphocytic choriomeningitis virus) to acidified endosomes2,15,17. Retro-2 was proved to have a broad-spectrum action on toxins (ricin, Stx, cholera toxin), viruses (Ebola, Marburg, vaccinia virus, enterovirus 71, adeno-associated virus, polyoma and papillomaviruses), intracellular bacteria (Sn, Ctr), and parasite (Leishmania) by interfering with the intracellular trafficking machinery at the EE-trans Golgi interface1,34,35. It is worth noting that ABMA and Retro-2 have demonstrated efficacy in vivo. Even if the list of pathogens tested do not overlap in these publications preventing insightful comparisons, distinct mode of action of inhibitors on host cells, and particularly on trafficking pathway, may explain the variety of anti-pathogen spectra observed. Thus, in some instances combinations of these inhibitors may increase, additionally or synergistically, the protection efficacy.
Altogether, our results show that the HTS hit ABMA has a remarkable potential for the development of broad-spectrum drugs against toxins, viruses, and intracellular bacteria and parasites. ABMA being a hit from HTS, there is reasonable hope to obtain other, more powerful, broad-spectrum inhibitors by medicinal chemistry optimization. Activity may be improved both in terms of decreasing the concentration giving maximum efficacy and increasing the level of pathogen inhibition.
ABMA carries a hydrophobic adamantane substituent. Adamantane derivatives have been developed since the 1960s as antiviral drugs against influenza virus infection36. However, amantadine, memantine and 1-(1-adamantyl) ethylamine were inactive against DT intoxication and against EBOV infection (data not shown). This indicates that the adamantane group is not sufficient to explain ABMA activity. ABMA and the antiviral adamantine derivatives must display different mechanisms of action to achieve antiviral effects.
The specific cellular target of compound ABMA has not yet been identified. Electron microscopy revealed the intracellular accumulation of MVBs/LE. The increase of LysoTracker, acridine orange and Rab7 staining, as well as the accumulation of cholesterol also demonstrate ABMA acts on the endosome pathway, by inducing the accumulation of acidic late endosomal compartments. Importantly, the integrity of other organelles was unaffected: EE, lysosomes, Golgi, ER and the nucleus.
The nature of the viruses inhibited by ABMA also suggests that LE is targeted by ABMA. EBOV needs the Niemann-Pick disease, type C1 protein (NPC1), a cholesterol transporter and LE/lysosomal protein, to enter cell cytosol37. RABV and DENV cell entry are less well characterized. However, it was described that DENV3 must enter Rab7-regulated LE to productively infect Vero cells38. In contrast, CHIKV is not sensitive to ABMA. Ninety-five % of CHIKV are internalized through clathrin-coated vesicles, the main internalization pathway for this virus, and then the virus exclusively fuse with EE membranes39,40.
LE have long been considered as important sorting stations in the endocytic pathway41; they determine whether particular proteins or lipids are targeted to lysosomes for degradation, or alternatively, recycled to the ER or the Golgi apparatus42. In addition, MVBs/LE may fuse with the plasma membrane to release exosomes43. The endosomal pathway is essential for several toxins and viruses to translocate into the cytosol41. Importantly, LE could also supply nutrition (i.e. cholesterol, membrane proteins) for the development of bacteria and parasites inside host cells30,44,45. Moreover, similarly to what we observe on human cells with ABMA (Figs 6 and 7), knock-down of Rab7 in HeLa cells results in enlarged MVBs/LE with increased ILVs, which consequently blocks EGFR exiting from MVBs/LE46. Thus, the pharmacologic interference of ABMA with the cellular function of Rab7, a key regulator of late endocytic trafficking, might explain its broad-spectrum anti-pathogen activity. Designing drugs that target LE may constitute an advantageous strategy to obtain broad-spectrum drugs against many intracellular pathogens.
U18666A, an inhibitor of cholesterol transport, induces cholesterol accumulation in LE and thereby inhibits toxins (anthrax LT), bacteria (Chlamydiae) and viruses (Vesicular Stomatitis Virus, DENV and Hepatitis C Virus)44,45,47. ABMA also induces cholesterol accumulation (this work). Both ABMA and U18666A inhibit DT cytotoxicity with similar protection factors (data not shown). Besides, the loss of NPC1 disrupts LE/lysosomes morphology and inhibits EBOV entry48. Thus, the mechanism of action of ABMA on host LE may produce multiple consequences to inhibit various pathogens.
In summary, we identified a broad-spectrum chemical inhibitor that hindered several toxins and pathogens by interfering with host specific late endosomal compartments. It protected mice from a lethal ricin challenge without showing toxicity to the animals. Our work highlights that a chemical harboring an action on a cellular component of the host has the potential of a broad-spectrum drug against various pathogens.
Methods
Chemicals and materials
1-adamantyl (5-bromo-2-methoxybenzyl) amine (ABMA) was purchased from Chembridge (ID: 5570320, San Diego, CA, USA). Ricin for screening, animal experiments and for in vitro validations was supplied by Bruno Beaumelle14. Toxin B (TcdB) was produced from Clostridium difficile VPI10463, lethal toxin (TcsL) was produced from Clostridium sordellii IP8249 and anthrax toxin were produced and purified as described previously50.
The following products were purchased from the indicated commercial sources: [14C]-leucine (Perkin-Elmer); Stx-2 (List Lab, USA); DMSO (D4540), diphtheria toxin DT (D0564), bafilomycin A1 (B1793), Hoechst 33342 (14533), filipin III (F4767), Acridine Orange (A6014), gelatin (G7765) were purchased from Sigma. The following commercial antibodies were used in this study: rabbit anti-Rab7 (ab137029) were from Abcam; Rabbit anti-Rab7 (D95F2) (#9367), rabbit anti-EEA1 (#3288) were from Cell Signaling, Rabbit anti-Lamp1 (L1418) and mouse anti-beta-actin (A2228) from Sigma-Aldrich; rabbit anti-MEK2 (N-20, sc-524), mouse anti-chlamydial trachomatis HSP60 protein (clone A57-B9, sc-57840) from Santa Cruz Technologies; mouse anti-SNAP-25 (SMI-81, 836304) from Biolegend; mouse anti-RNP (ribonucleoprotein) conjugated with FITC from Fujirebio; Alexa 488-donkey anti-rabbit (A10042), Alexa 546-donkey anti-mouse (A10036) and LysoTracker Deep Red (L12492) were from ThermoFisher Scientific.
HTS
For a full description of the HTS procedure see our previous work14.
In vivo experiments
Animal studies were done at French Health Products Safety Agency (ANSM) animal care facility and in compliance with ANSM committee policies according to European regulations. Pathogen-free six week-old female BALB/c mice were purchased from Charles River Laboratories (L’Arbresle, France). Mice were housed under a 12-hour light-dark cycle and fed a standard diet ad libidum. Standardized groups of mice were injected intraperitoneally with 500 µL of sterile saline solution (0.9% NaCl) supplemented with 1–10% DMSO alone (control) or with various doses of ABMA one hour prior to toxin administration. Mice were anesthetized by intraperitoneal injection (100 µL) of ketamine (1.15 mg final)-rompun (xylazine, 0.28 mg final) solution and exposed to 50 µL of ricin (2 µg/kg) by intranasal instillation corresponding to one DL90 at day 0. Each drug-treated group contained five to ten mice, and normal controls contained ten mice. Survival was recorded daily. Data for mice in each test group were compared to those for untreated ricin-challenged mice by the log rank test (Prism, Graphpad Inc., San Diego, Calif.) and p-values ≤ 0.05 were considered statistically significant.
Ethics Statement
Animal experiments are carried out in accordance with decrees (Decree No. 2013–118 of 1 February 2013 on the protection of animals used for scientific purposes), national orders (Articles L214-3, R214-87 to R214-10 of the Code rural) and European directives (86/609 EEC of 24 November 1986 and Directive 2010/63/EU of the European Parliament and of the Council of 22 September 2010 on the protection of animals used in For scientific purposes). The ethics committee “Comité d'éthique régional Languedoc Roussillon” CEEA-LR reviewed and approved the study and its protocols under the permit to experiment CEEA-LR-1035.
Evaluation of broad-spectrum anti-toxin and anti-intracellular microorganism activity
The procedures of all experiments are described in supplementary information, see Supplemental Material and Methods.
Immunocytochemistry and live staining
Cells were grown on glass coverslips one day before. Following treatments cells were rinsed with PBS, fixed with 4% paraformaldehyde-PBS for 20 min at room temperature. After three times washes with PBS, cells were permeabilized in 0.1% Saponin or 0.2% Triton for 5 min. Subsequently, cells were blocked and stained with antibodies. Finally, the slides were mounted on glass slides and imaged with an inverted microscope (Ti-U, Nikon) or confocal microscope (SP8X, Leica). For live staining, fluorophore labeled-cells in the presence of compound or DMSO were washed and visualized under confocal microscope immediately.
Electron microscopy
Confluent cultures of A549 cells (ATCC) treated with 30 µM ABMA or DMSO for 22 h were fixed by 2.5% glutaraldehyde in 0.1 M cacodylate buffer (pH 7.4) for 2 h. Cells were scraped, collected and rinsed with 0.1 M cacodylate buffer for 3 times, then the pellets were post fixed with 1% osmium and 1.5% potassium ferrocyanide for 1 h, processed for dehydration in graded ethanol series and infiltrated in Epon resin mixed with propylene oxide. Ultrathin sections (80 nm) were stained with Oolong Tea extracts (OTE) for 30 min, followed by lead citrate staining for 6 min, and examined by JEOL1400 transmission electron microscope operating at 80 kV.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
References
Gupta, N. et al. Inhibitors of retrograde trafficking active against ricin and Shiga toxins also protect cells from several viruses, Leishmania and Chlamydiales. Chem Biol Interact 267, 96–103, https://doi.org/10.1016/j.cbi.2016.10.005 (2017).
Gillespie, E. J. et al. Selective inhibitor of endosomal trafficking pathways exploited by multiple toxins and viruses. Proc Natl Acad Sci USA 110, E4904–4912, https://doi.org/10.1073/pnas.1302334110 (2013).
Zilbermintz, L. et al. Identification of agents effective against multiple toxins and viruses by host-oriented cell targeting. Sci Rep 5, 13476, https://doi.org/10.1038/srep13476 (2015).
Leonardi, W. et al. Bithionol blocks pathogenicity of bacterial toxins, ricin, and Zika virus. Sci Rep-Uk 6, https://doi.org/10.1038/Srep34475 (2016).
Saenz, J. B., Doggett, T. A. & Haslam, D. B. Identification and characterization of small molecules that inhibit intracellular toxin transport. Infection and Immunity 75, 4552–4561, https://doi.org/10.1128/IAI.00442-07 (2007).
Spooner, R. A. & Watson, P. Drug targeting: Learning from toxin entry and trafficking in mammalian cells. Curr Opin Drug Disc 13, 86–95 (2010).
Bekerman, E. & Einav, S. Infectious disease. Combating emerging viral threats. Science 348, 282–283, https://doi.org/10.1126/science.aaa3778 (2015).
Sandvig, K. & van Deurs, B. Delivery into cells: lessons learned from plant and bacterial toxins. Gene Ther 12, 865–872, https://doi.org/10.1038/sj.gt.3302525 (2005).
Miller, S. & Krijnse-Locker, J. Modification of intracellular membrane structures for virus replication. Nature reviews. Microbiology 6, 363–374, https://doi.org/10.1038/nrmicro1890 (2008).
Barbier, J., Cintrat, J. C. & Gillet, D. Intracellular pathogens convert macrophages from death traps into hospitable homes. FEBS J 283, 595–597, https://doi.org/10.1111/febs.13657 (2016).
Sandvig, K., Torgersen, M. L., Engedal, N., Skotland, T. & Iversen, T.-G. Protein toxins from plants and bacteria: Probes for intracellular transport and tools in medicine. FEBS Letters 584, 2626–2634, https://doi.org/10.1016/j.febslet.2010.04.008 (2010).
Samanta, D., Mulye, M., Clemente, T. M., Justis, A. V. & Gilk, S. D. Manipulation of Host Cholesterol by Obligate Intracellular Bacteria. Front Cell Infect Mi 7, https://doi.org/10.3389/Fcimb.2017.00165 (2017).
Herweg, J. A. et al. Proteomic analysis of the Simkania-containing vacuole: the central role of retrograde transport. Mol Microbiol 99, 151–171, https://doi.org/10.1111/mmi.13222 (2016).
Stechmann, B. et al. Inhibition of retrograde transport protects mice from lethal ricin challenge. Cell 141, 231–242, https://doi.org/10.1016/j.cell.2010.01.043 (2010).
Tehran, D. A. et al. A Novel Inhibitor Prevents the Peripheral Neuroparalysis of Botulinum Neurotoxins. Sci Rep-Uk 5, https://doi.org/10.1038/Srep17513 (2015).
Schnell, L. et al. Semicarbazone EGA Inhibits Uptake of Diphtheria Toxin into Human Cells and Protects Cells from Intoxication. Toxins 8, https://doi.org/10.3390/Toxins8070221 (2016).
Schnell, L. et al. EGA Protects Mammalian Cells from Clostridium difficile CDT, Clostridium perfringens Iota Toxin and Clostridium botulinum C2 Toxin. Toxins 8, https://doi.org/10.3390/Toxins8040101 (2016).
Audi, J., Belson, M., Patel, M., Schier, J. & Osterloh, J. Ricin poisoning: a comprehensive review. Jama 294, 2342–2351 (2005).
Tonello, F. & Montecucco, C. The anthrax lethal factor and its MAPK kinase-specific metalloprotease activity. Mol Aspects Med 30, 431–438, https://doi.org/10.1016/j.mam.2009.07.006 (2009).
Popoff, M. R. et al. Ras, Rap, and Rac small GTP-binding proteins are targets for Clostridium sordellii lethal toxin glucosylation. J Biol Chem 271, 10217–10224 (1996).
Rossetto, O., Pirazzini, M. & Montecucco, C. Botulinum neurotoxins: genetic, structural and mechanistic insights. Nature reviews. Microbiology 12, 535–549, https://doi.org/10.1038/nrmicro3295 (2014).
Gillet, D., VILLIERS, B., Pichard, S., Maillere, B. & Sanson, A. Hb-egf inhibitor derived from the R domain of diphtheria toxin for the treatment of diseases associated with the activation of the HB-EGF/EGFR pathway (US Patent 9,758,552, 2017)
Gillet, D. & Barbier, J. in The Comprehensive Sourcebook of Bacterial Protein Toxins (Fourth Edition) (eds Daniel Ladant & Michel R. Popoff) 111–132 (Academic Press, 2015).
Patil, S. et al. Botulinum Toxin: Pharmacology and Therapeutic Roles in Pain States. Current pain and headache reports 20, 15, https://doi.org/10.1007/s11916-016-0545-0 (2016).
Dolly, J. O. & Lawrence, G. W. Chapter 3: Molecular basis for the therapeutic effectiveness of botulinum neurotoxin type A. Neurourology and Urodynamics 33, S14–S20, https://doi.org/10.1002/nau.22634 (2014).
White, J. M. & Whittaker, G. R. Fusion of Enveloped Viruses in Endosomes. Traffic 17, 593–614, https://doi.org/10.1111/tra.12389 (2016).
Damiani, M. T., Gambarte Tudela, J. & Capmany, A. Targeting eukaryotic Rab proteins: a smart strategy for chlamydial survival and replication. Cell Microbiol 16, 1329–1338, https://doi.org/10.1111/cmi.12325 (2014).
Beatty, W. L. Trafficking from CD63-positive late endocytic multivesicular bodies is essential for intracellular development of Chlamydia trachomatis. J Cell Sci 119, 350–359, https://doi.org/10.1242/jcs.02733 (2006).
Robertson, D. K., Gu, L., Rowe, R. K. & Beatty, W. L. Inclusion biogenesis and reactivation of persistent Chlamydia trachomatis requires host cell sphingolipid biosynthesis. PLoS Pathog 5, e1000664, https://doi.org/10.1371/journal.ppat.1000664 (2009).
Lievin-Le Moal, V. & Loiseau, P. M. Leishmania hijacking of the macrophage intracellular compartments. FEBS J 283, 598–607, https://doi.org/10.1111/febs.13601 (2016).
Real, F. & Mortara, R. A. The diverse and dynamic nature of Leishmania parasitophorous vacuoles studied by multidimensional imaging. PLoS Negl Trop Dis 6, e1518, https://doi.org/10.1371/journal.pntd.0001518 (2012).
Marquer, C. et al. Arf6 controls retromer traffic and intracellular cholesterol distribution via a phosphoinositide-based mechanism. Nat Commun 7, 11919, https://doi.org/10.1038/ncomms11919 (2016).
White, I. J., Bailey, L. M., Aghakhani, M. R., Moss, S. E. & Futter, C. E. EGF stimulates annexin 1-dependent inward vesiculation in a multivesicular endosome subpopulation. EMBO J 25, 1–12, https://doi.org/10.1038/sj.emboj.7600759 (2006).
Dai, W. et al. Antiviral effects of Retro-2cycl and Retro-2.1 against Enterovirus 71 in vitro and in vivo. Antiviral Res 144, 311–321, https://doi.org/10.1016/j.antiviral.2017.07.001 (2017).
Carney, D. W. et al. Structural optimization of a retrograde trafficking inhibitor that protects cells from infections by human polyoma- and papillomaviruses. Bioorgan Med Chem 22, 4836–4847, https://doi.org/10.1016/j.bmc.2014.06.053 (2014).
Davies, W. L. et al. Antiviral Activity of 1-Adamantanamine (Amantadine). Science 144, 862–863, https://doi.org/10.1126/Science.144.3620.862 (1964).
Martin, B., Hoenen, T., Canard, B. & Decroly, E. Filovirus proteins for antiviral drug discovery: A structure/function analysis of surface glycoproteins and virus entry. Antiviral Res 135, 1–14, https://doi.org/10.1016/j.antiviral.2016.09.001 (2016).
Piccini, L. E., Castilla, V. & Damonte, E. B. Dengue-3 Virus Entry into Vero Cells: Role of Clathrin-Mediated Endocytosis in the Outcome of Infection. PLoS One 10, e0140824, https://doi.org/10.1371/journal.pone.0140824 (2015).
Bernard, E. et al. Endocytosis of chikungunya virus into mammalian cells: role of clathrin and early endosomal compartments. PLoS One 5, e11479, https://doi.org/10.1371/journal.pone.0011479 (2010).
Hoornweg, T. E. et al. Dynamics of Chikungunya Virus Cell Entry Unraveled by Single-Virus Tracking in Living Cells. J Virol 90, 4745–4756, https://doi.org/10.1128/JVI.03184-15 (2016).
Gruenberg, J. & van der Goot, F. G. Mechanisms of pathogen entry through the endosomal compartments. Nat Rev Mol Cell Biol 7, 495–504, https://doi.org/10.1038/nrm1959 (2006).
Gruenberg, J. The endocytic pathway: A mosaic of domains. Nat Rev Mol Cell Bio 2, 721–730, https://doi.org/10.1038/35096054 (2001).
Alenquer, M. & Amorim, M. J. Exosome Biogenesis, Regulation, and Function in Viral Infection. Viruses 7, 5066–5083, https://doi.org/10.3390/v7092862 (2015).
Sobo, K. et al. Late endosomal cholesterol accumulation leads to impaired intra-endosomal trafficking. PLoS One 2, e851, https://doi.org/10.1371/journal.pone.0000851 (2007).
Beatty, W. L. Late endocytic multivesicular bodies intersect the chlamydial inclusion in the absence of CD63. Infect Immun 76, 2872–2881, https://doi.org/10.1128/IAI.00129-08 (2008).
Vanlandingham, P. A. & Ceresa, B. P. Rab7 regulates late endocytic trafficking downstream of multivesicular body biogenesis and cargo sequestration. J Biol Chem 284, 12110–12124, https://doi.org/10.1074/jbc.M809277200 (2009).
Poh, M. K. et al. U18666A, an intra-cellular cholesterol transport inhibitor, inhibits dengue virus entry and replication. Antiviral Res 93, 191–198, https://doi.org/10.1016/j.antiviral.2011.11.014 (2012).
Cote, M. et al. Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature 477, 344–348, https://doi.org/10.1038/nature10380 (2011).
Genth, H. et al. Haemorrhagic toxin and lethal toxin from Clostridium sordellii strainvpi9048: molecular characterization and comparative analysis of substrate specificity of the large clostridial glucosylating toxins. Cell Microbiol 16, 1706–1721, https://doi.org/10.1111/cmi.12321 (2014).
Rolando, M. et al. Transcriptome dysregulation by anthrax lethal toxin plays a key role in induction of human endothelial cell cytotoxicity. Cell Microbiol 12, 891–905, https://doi.org/10.1111/j.1462-5822.2010.01438.x (2010).
Acknowledgements
We greatfully thank Anne Doye (Université de Nice Sophia-Antipolis) for technical assistance and Bruno Beaumelle for providing ricin. This work has been funded by the joint ministerial program of R&D against CBRNE risks and CEA, and benefited from the core facilities of Imagerie-Gif (http://www.i2bc.paris-saclay.fr), member of IBiSA (http://www.ibisa.net), supported by “France-BioImaging” (ANR-10-INBS-04–01) and the Labex “Saclay Plant Science” (ANR-11-IDEX-0003–02). This work was also supported by U.S. National Institutes of Health and National Institute of Allergy and Infectious Diseases grant R01AI063513; Defense Threat Reduction Agency grant HDTRA1–12–1–0002; and the Douglass and Ewing Halsell Foundations. Work on Simkania and Chlamydia was supported by the Deutsche Forschungsgemeinschaft (DFG) Priority programme 1580 to T.R. SIMOPRO and SCBM are members of the Laboratory of Excellence LERMIT supported by a grant from the Agence Nationale de la Recherche (ANR-10-LABX-33) and RetroLeishma project R3.
Author information
Authors and Affiliations
Contributions
D.G. coordinated the research. G.M., E.G., R.L., and J.B. designed and operated the HTS. V.P. and J.-C.C. conceived and designed chemistry experiments. V.P. performed the synthesis of ABMA. L.P. and D.S. conceived and operated ricin in vivo experiments. J.B. directed toxins’ research. Y.W. and A.G. performed protein biosynthesis assays. Y.W. performed DT, TcsL and TcdB assay. E.L. performed anthrax toxin experiments. Ce.B. performed BoNT/A assay. M.-R.P. prepared clostridial toxins. R.-A.D. conceived and operated Ebola virus experiments. S.K. and N.T. conceived and operated Rabies virus experiments. R.Y., C.A., P.C. and R.L.G. conceived and operated Dengue-4 experiments. A.F., J.-A.H., J.L. and T.R. conceived and operated Chlamydiales experiments. S.C., Y.W. and P.M.L. conceived and operated Leishmania experiments. Y.W., C.G. and Cl.B. performed electron microscopy experiments. Y.W. performed FACS and immunofluorescence experiments. Y.W., D.G., and J.B. drafted the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, Y., Pons, V., Goudet, A. et al. ABMA, a small molecule that inhibits intracellular toxins and pathogens by interfering with late endosomal compartments. Sci Rep 7, 15567 (2017). https://doi.org/10.1038/s41598-017-15466-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-15466-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.