Abstract
Gallstone disease (GD) is a common digestive disorder that shares many risk factors with cardiovascular disease (CVD). CVD is an important public health issue that encompasses a large percentage of overall mortality. Several recent studies have suggested an association between GD and CVD, while others have not. In this report, we present a meta-analysis of cohort studies to assess the association between GD and CVD. We included eight studies published from 1980 to 2017, including nearly one million participants. The pooled relative risk (RR, 95% confidence interval [CI]) from the random-effects model associates with GD is 1.23 (95% CI: 1.17–1.30) for fatal and nonfatal CVD events. The pooled RR from the random-effects model of CVD events in female patients with GD is 1.24 (95% CI: 1.16–1.32). In male GD patients, the pooled RR from the random-effects model for CVD is 1.18 (95% CI: 1.06–1.31). Our meta-analysis demonstrates a substantially increased risk of fatal and nonfatal CVD events among patients with a medical history of GD. We suggest that interested investigators should further pursue the subject. In addition, both male and female patients with GD have a risk of CVD, and women have a higher risk than men.
Similar content being viewed by others
Introduction
Gallstone disease (GD) is one of the most common medical problems, exhibiting a prevalence of 10–20% in adults. GD is a common indication for surgical intervention in developed countries1,2. GD is also one of the most costly gastrointestinal tract disorders in the world3. According to macroscopic appearance and chemical composition, GD is divided into two major types: pigment and cholesterol gallstones4.
Cardiovascular disease (CVD) is the leading cause of death globally5. CVD is a group of disorders of the heart and blood vessels, including stroke and ischaemic heart disease (IHD)6. A number of risk factors of CVD have been identified, such as age7, obesity8, body mass index (BMI)9, low serum high density lipoprotein (HDL) cholesterol levels10, diabetes mellitus (DM)11, insufficient physical inactivity12, smoking13, excessive use of alcohol14, and elevated blood pressure15. These risk factors are also associated with an increased risk of GD.
Recently, many epidemiological studies have reported an association between GD and CVD, while others have found no association. An analysis published in 2016 by Zheng et al.16 that included five articles suggested that GD was associated with an increased risk of coronary heart disease (CHD). However, the analysis was hampered by a degree of high heterogeneity. Neither heterogeneity analysis nor further subgroup analysis was performed. Finally, these researchers’ analysis was limited to CHD, rather than to CVD. Therefore, we performed a meta-analysis of cohort studies to further explore a possible association between GD and CVD.
Methods
Search strategy
In October 2016, we searched PubMed and EMBASE for studies describing the association between GD and CVD. We updated the search in June 2017 to verify that our study was based on the most current data. We also checked the references of included studies and reviews. Only papers issued in the English language were considered. The search focused on six medical subject headings terms and key words: gallstone disease, stroke, coronary heart disease, myocardial infarction (MI), ischaemic heart disease, and cardiovascular disease. The logical operator “and” was used to combine search terms.
Study selection
Literature eligibility was assessed by two investigators independently. Discordant conclusions were settled by consensus. Inclusion criteria were as follows: (1) the study was a cohort study; (2) the authors reported data from an original, peer-reviewed study (i.e., not review articles or meeting abstracts); and (3) the authors reported risk estimates of the association between GD and CVD. When an article included multiple publications, we included the article with the longest follow-up years or the largest number of incident cases. We qualified articles for further examination by performing an initial screen of identified titles and abstracts, followed by full-text review.
Data extraction
The following information was extracted from the included studies: study name, authors, publication year, region, study population, study design, age range, percentage female patients, years of follow-up, sample size, outcomes, data collection, assessment of GD, adjusted relative risk (RR, 95% confidence interval [CI]) and confounder adjustment. The primary clinical outcome of the study was a combined endpoint including fatal and nonfatal CVD events. If the information was unavailable from the report, we attempted to collect relevant data by corresponding with the authors. We utilized the Newcastle - Ottawa Quality Assessment Scale (NOS)17 to evaluate the quality of included studies with consideration of the following aspects: selection, comparability and exposure.
Data synthesis and analysis
The fully adjusted RR was used to estimate the association between GD and CVD. Forest plots were created to visually assess the RRs and corresponding 95% CIs across studies. In the forest plots, each study as well as its summary effect was depicted as a point estimate bounded by a confidence interval. This representation showed whether the effects for all studies were consistent or whether they varied substantially from one study to the next. RR > 1 and 95% CI excluding 0 meant a positive correlation18. Heterogeneity across studies was assessed by the Cochrane Q statistic (significance level of p < 0.10) and the I2 statistic (ranges from 0–100%, with lower values representing less heterogeneity)19. The RRs were pooled using random-effects models20.
Pre-specified subgroup analyses were performed to examine the impacts of various study characteristics, including region, years of follow-up, sample size, rate of CVD events and the degree of adjustment for the most important confounders. A sensitivity analysis was conducted to assess the influence of each individual study on the summary risk estimate using the trim and fill method21. Remaining studies were reanalysed following the omission of one study at a time. Finally, the potential publication bias was examined by visual inspection of the funnel plot and the result of Egger’s test (p < 0.10)22. A roughly symmetrical funnel plot suggested no publication bias23. All analyses were performed using STATA version 14.1 (Stata Corp, College Station, Texas). A p-value < 0.05 was considered statistically significant, except where otherwise specified24.
Results
Literature search
A total of 566 articles were retrieved in the initial search. Of these, 20 duplicate articles were excluded. After a first round of screening based on titles and abstracts, 12 articles remained for further review. After comprehensive full-text examination, four articles were excluded as they were reviews. Ultimately, eight articles16,25,26,27,28,29,30,31 were eligible for analysis (Table 1).
Study characteristics
There were 11 retrospective cohort studies among the eight articles: one article16 included three cohort studies, and another article25 included two cohort studies. The characteristics of the 11 studies among the eight articles are displayed in Table 2. Five studies were questionnaire-based, and six studies were reviews of hospital records. Five studies specifically reported results on CHD; two studies reported CVD mortality; one study reported IHD; one study reported stroke; and two studies reported multiple outcomes. The assessment of GD varied across studies: one study used definite hospital diagnosis; two studies relied on ICD codes; two studies relied on evidence of a cholecystectomy or a definite hospital diagnosis; one study relied on evidence of a cholecystectomy and imaging diagnosis; three studies relied on evidence of a cholecystectomy, a definite hospital diagnosis, or an imaging diagnosis; and one study relied on evidence of a cholecystectomy, a definite hospital diagnosis, an imaging diagnosis, or postmortem pathologic examination. Eight studies were published after 2010. With regard to the study region, three studies were published in Asia, seven in the US, and one in Germany. Three studies included only female patients. Two studies included only males. Follow-up duration ranged from 6 to 30 years. The age range of participants in most studies included young and middle-aged patients, and the upper limit for one study was 8028. The maximum sample size was 487,37327, and the minimum sample size was 60526. The average sample size was 107,057. Adjustment for potential confounding factors varied among studies. Most risk estimates were adjusted for age and gender. The study types of included studies were all retrospective cohort studies.
GD and risk of CVD
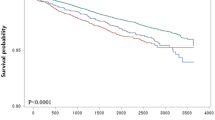
The majority of studies reported a positive association, but the RRs reported by three articles were not statistically significant25,26,29. Patients with GD had a 23% higher risk of CVD than the patients in the control groups [95% CI = 1.17–1.30, Fig. 1]. We detected substantial heterogeneity among studies (I2 = 74.2%; p < 0.000).
Subgroup and sensitivity analyses
We conducted subgroup analyses by length of follow-up, sample size, region, rate of CVD events, and the degree of adjustment for the most important confounders (Table 3). The subgroups of ≦10 years follow-up (I2 = 13.4%, RR: 1.26, 95% CI: 1.20–1.31), ≦50,000 participants (I2 = 20.8%, RR: 1.27, 95% CI: 1.24–1.31), CVD mortality (I2 = 0%, RR: 1.05, 95% CI: 0.94–1.16), and incomplete adjustment (I2 = 39%, RR: 1.30, 95% CI: 1.21–1.39) showed a marked decrease in heterogeneity. We observed a non-significant association between GD and fatal CVD events, but this result was not reliable due to a lack of data (only three studies reported the fatal CVD events). We therefore speculated that heterogeneity might result from years of follow-up, number of participants and the degree of adjustment for the most important confounders.
There were five articles with eight studies reporting the relative risk for males and/or females. One study reported a RR < 1.00, but this estimate was not statistically significant. Pooled RR from the random-effects model for women was 1.24 (95% CI: 1.16–1.32, I2 = 78.5%, Fig. 2). The pooled RR from the random-effects model for men was 1.18 (95% CI: 1.06–1.31, I2 = 90.7%, Fig. 2). Both sexes with GD had a risk of CVD, but the risk for women was higher than that of men.
A sensitivity analysis of omitting one study at a time showed no substantial change in the results. The trim and fill method showed no trimming, and the data were unchanged (Fig. 3).
Cholecystectomy and risk of CVD
Wirth et al.31 and Ruhl et al.29 reported that cholecystectomy increased the risk of CVD, with a rate of surgery of 66.2% and 74.6% among GD patients. The RRs were 1.32 (95% CI: 1.05–1.65) and 1.3 (95% CI: 1.1–1.6), respectively. Olaiya et al.28 and Zheng et al.23 suggested a trend towards no differences among groups, but there were insufficient data to perform a statistical analysis.
Publication bias
There was no publication bias according to the visual inspection of the funnel plot (Fig. 4) and the result of Egger’s test (p = 0.467).
Discussion
In this meta-analysis comprising approximately one million participants, we demonstrate that a history of GD gives a 1.23-fold increased risk of CVD. We also demonstrate that women may have a higher risk of CVD than men. In addition, patients undergoing cholecystectomy may have a higher risk of CVD than GD patients without surgical treatment, but the data are insufficient to draw a statistically significant conclusion.
Most of the studies attribute both GD and CVD to common risk factors. However, the RRs collected from included studies were all adjusted for these common risk factors, such as age, obesity, BMI, diabetes, hypertension, unhealthy diet and physical inactivity. All but two articles16,27 show a decline in RR after adjustment, but the results still were significant, these two articles suggest that hypertension, obesity and diabetes mellitus are protective factors. Two studies28,30 suggest that younger patients are at higher risk than older patients, but that the elderly in general tend to have more risk factors. Taken together, these results suggest aetiologies apart from the known common risk factors. Cholesterol accumulation is a major feature of both GD and atherosclerosis. The association between GD and CVD may due to a shared metabolic pathway involving cholesterol and other pathophysiological features. Low HDL level is known to increase risk of CVD morbidity and mortality32 and has been shown to play a role in the development of GD33. One study suggests that insulin-like growth factor one (IGF-1) is involved in gallbladder emptying and may have an anti-atherosclerotic effect, which suggests that low plasma levels of IGF-1 may result in both GD and CHD34. Oxidative stress also plays an important role in the development of GD35 and has been implicated in the pathogenesis of CVD as well36.
Many studies indicate that the gut microbiota influences host health. A recent study suggests that altered composition of gut microbiota increase the risk of CVD by derived signalling molecules37, and GD is related to microbiota dysbiosis in the gut and biliary tract38. Mounting evidence suggests that non-alcoholic fatty liver disease (NAFLD) is a risk factor for IHD39. Additionally, a recent study shows an association between GD and NAFLD40, and preliminary evidence suggests that GD is associated with more severe liver damage in NAFLD patients41,42. Although the mechanisms have not been fully elucidated, these studies suggest new avenues for prevention and treatment.
Traditionally, CVD has been thought of as a male disease. According to our study, however, women with GD may have a higher risk of CVD than men. The explanation for this phenomenon is unknown, but we speculate that it may be related to the following factors. Low HDL levels contribute to the development of GD33 and CVD, peak total cholesterol levels occur later in men than in women, and HDL levels decrease in postmenopausal women. Diabetes increases the risk of GD43 and death from CHD44, and the incidence of diabetes in women is higher than in men. Elderly women with CHD are more likely to suffer from metabolic syndrome44. Low socioeconomic status increases the risk of CVD45 and GD46.
There are two distinct points of view regarding whether cholecystectomy increases the risk of CVD in GD patients. Wirth et al.31 and Ruhl et al.29 suggest that cholecystectomy increases the risk, while Olaiya et al.28 and Zheng et al. [23] find no significant difference. We agree with the former viewpoint, though there are not enough data to support this conclusion. Our reasons are as follows: cholecystectomized mice have elevated serum levels of very low-density lipoprotein47; cholecystectomy may impact lipid and glucose metabolism48,49; gallbladder-related hormones have a beneficial effect on metabolic syndrome50; and cholecystectomy changes bile flow to the intestine and therefore alters the microbiota between bile acids and the intestine51. More studies are needed to establish a connection more firmly.
Several limitations of this meta-analysis should be acknowledged. First, we find substantial heterogeneity across studies, possibly arising from years of follow-up, number of participants and the degree of adjustment for the most important confounders. Second, the meta-analysis is restricted to English-language publications, and the possibility of unpublished reports is not yet identified. Third, although the assessment of GD varies across these cohort studies, most studies include evidence of a cholecystectomy or a definite hospital diagnosis. Therefore, we do not believe that differences in assessments will reverse the results. Fourth, the varying degree of confounder adjustments across the individual studies hampers a systematic assessment of the impact of known risk factors on the outcome of interest. Finally, the observational retrospective design does not allow for establishing causality. The strengths of our study include the following: we performed a comprehensive systematic search for eligible studies; literature eligibility was assessed by two investigators independently; we included sufficient numbers of participants with ample follow-up time; no significant publication bias was found; and the sensitivity analysis showed no substantial change in the results.
Conclusions
Our meta-analysis demonstrates a substantially increased risk of CVD among patients with a medical history of GD. We suggest that interested investigators should further pursue the subject. We show that the women may have a higher risk of CVD than men and that cholecystectomy may increase the risk of CVD. Further research is warranted.
References
Freeman, J., Boomer, L., Fursevich, D. & Feliz, A. Ethnicity and insurance status affect health disparities in patients with gallstone disease. The Journal of surgical research 175, 1–5, https://doi.org/10.1016/j.jss.2011.06.064 (2012).
Liu, J. et al. Non-alcoholic fatty liver disease associated with gallstones in females rather than males: a longitudinal cohort study in Chinese urban population. BMC Gastroenterol. 14, 1–7 (2014).
Li, X., Guo, X., Ji, H., Yu, G. & Gao, P. Gallstones in Patients with Chronic Liver Diseases. BioMed research international 2017, 9749802, https://doi.org/10.1155/2017/9749802 (2017).
Lammert, F. et al. Gallstones. Nature reviews. Disease primers 2, 16024, https://doi.org/10.1038/nrdp.2016.24 (2016).
Kalra, A. et al. Overview of Coronary Heart Disease Risk Initiatives in South Asia. Current atherosclerosis reports 19, 25, https://doi.org/10.1007/s11883-017-0662-1 (2017).
Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (London, England) 385, 117–171, doi:https://doi.org/10.1016/s0140-6736(14)61682-2 (2015).
Van, L. R., Klaver, C. C., Vingerling, J. R., Hofman, A. & de Jong, P. T. The risk and natural course of age-related maculopathy: follow-up at 6 1/2 years in the Rotterdam study. Archives of Ophthalmology 121, 519 (2003).
Klein, B. E., Klein, R., Lee, K. E. & Jensen, S. C. Measures of obesity and age-related eye diseases. Ophthalmic Epidemiology 8, 251 (2001).
Kharga, B. et al. Obesity Not Necessary, Risk of Symptomatic Cholelithiasis Increases as a Function of BMI. Journal of clinical and diagnostic research: JCDR 10, Pc28–pc32, https://doi.org/10.7860/jcdr/2016/22098.8736 (2016).
Jain, A., Puri, R. & Nair, D. R. South Asians: why are they at a higher risk for cardiovascular disease? Current opinion in cardiology 32, 430–436, https://doi.org/10.1097/hco.0000000000000411 (2017).
Shukla, S. K. et al. HMGCS2 is a key ketogenic enzyme potentially involved in type 1 diabetes with high cardiovascular risk. Scientific reports 7, 4590, https://doi.org/10.1038/s41598-017-04469-z (2017).
Grotemeyer, K. C. & Lammert, F. [Gallstones - Causes and Consequences]. Deutsche medizinische Wochenschrift (1946) 141, 1677–1682, https://doi.org/10.1055/s-0042-113238 (2016).
Mitchell, P., Wang, J. J., Smith, W. & Leeder, S. R. Smoking and the 5-year incidence of age-related maculopathy: the Blue Mountains Eye Study. Clinical & Experimental Ophthalmology 32, 255–258 (2004).
Bardach, A. E., Caporale, J. E., Rubinstein, A. L. & Danaei, G. Impact of level and patterns of alcohol drinking on coronary heart disease and stroke burden in Argentina. PLoS One 12, e0173704, https://doi.org/10.1371/journal.pone.0173704 (2017).
Hogg, R. E. et al. Cardiovascular Disease and Hypertension Are Strong Risk Factors for Choroidal Neovascularization. Ophthalmology 115, 1046 (2008).
Zheng, Y. et al. Gallstones and Risk of Coronary Heart Disease: Prospective Analysis of 270 000 Men and Women From 3 US Cohorts and Meta-Analysis. Arteriosclerosis Thrombosis & Vascular Biology 36, 1997 (2016).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European journal of epidemiology 25, 603–605, https://doi.org/10.1007/s10654-010-9491-z (2010).
Sutton, A. J. et al. Methods for meta-analysis in medical research. (2000).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. British Medical Journal 327, 557–560 (2003).
Dersimonian, R. & Laird, N. Meta-analysis in clinical trials. Controlled Clinical Trials 7, 177–188 (1986).
Duval, S. & Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455 (2000).
Schnee, S. et al. Bias in meta-analysis detected by a simple, graphical test. Bmj 315, 629 (1997).
Sterne, J. A., Becker, B. J. & Egger, M. The funnel plot. Publication bias in meta-analysis: Prevention, assessment and adjustments, 75–98 (2005).
Wang, J. et al. Relation of phosphodiesterase type 5 inhibitors and malignant melanoma: a meta-analysis and systematic review (2017).
Bortnichak, E. A. et al. The association between cholesterol cholelithiasis and coronary heart disease in Framingham, Massachusetts. American Journal of Epidemiology 121, 19–30 (1985).
Grimaldi, C. H. et al. Increased mortality with gallstone disease: results of a 20-year population-based survey in Pima Indians. Annals of internal medicine 118, 185–190 (1993).
Lv, J. et al. Gallstone Disease and the Risk of Ischemic Heart Disease. Arteriosclerosis Thrombosis & Vascular Biology 35 (2015).
Muideen Tunbosun Olaiya, H.-Y. C., Jiann-Shing, J., Li-Ming, L. & Fang-I, H. Significantly Increased Risk of Cardiovascular Disease among Patients with Gallstone Disease: A Population-Based Cohort Study. Plos One 8, e76448 (2013).
Ruhl, C. E. & Everhart, J. E. Gallstone Disease is Associated with Increased Mortality in the United States. Gastroenterology 140, 508–516 (2011).
Wei, C. Y. et al. Gallstone disease and the risk of stroke: a nationwide population-based study. Journal of Stroke & Cerebrovascular Diseases 23, 1813–1820 (2014).
Wirth, J. et al. Presence of gallstones and the risk of cardiovascular diseases: The EPIC-Germany cohort study. European Journal of Preventive Cardiology 22, 326 (2015).
Cohen, J. B. & Cohen, D. L. Cardiovascular and Renal Effects of Weight Reduction in Obesity and the Metabolic Syndrome. Current Hypertension Reports 17, 1–7 (2015).
Serin, H. İ. et al. The association between gallstone disease and plaque in the abdominopelvic arteries. Journal of Research in Medical Sciences the Official Journal of Isfahan University of Medical Sciences 22, 11 (2017).
Twickler, M. T., Cramer, M. J. & van Erpecum, K. J. Insulin-like growth factor-1: a common metabolic pathway in the origin of both gallstones and coronary heart disease. American Journal of Gastroenterology 100, 2363–2364 (2005).
Geetha, A. Evidence for Oxidative Stress in the Gall Bladder Mucosa of Gall Stone Patients. J Biochem Mol Biol Biophys 6, 427–432 (2002).
Otani, H. Oxidative stress as pathogenesis of cardiovascular risk associated with metabolic syndrome. Antioxidants & Redox Signaling 15, 1911 (2011).
Tang, W. H., Kitai, T. & Hazen, S. L. Gut Microbiota in Cardiovascular Health and Disease. Circulation Research 120, 1183 (2017).
Wu, T. et al. Gut microbiota dysbiosis and bacterial community assembly associated with cholesterol gallstones in large-scale study. BMC genomics 14, 669, https://doi.org/10.1186/1471-2164-14-669 (2013).
Byrne, C. D. & Targher, G. Ectopic fat, insulin resistance, and nonalcoholic fatty liver disease: implications for cardiovascular disease. Arteriosclerosis Thrombosis & Vascular Biology 34, 1155 (2014).
Ahmed, M. H. & Ali, A. Nonalcoholic fatty liver disease and cholesterol gallstones: which comes first? Scandinavian Journal of Gastroenterology 49, 521–527 (2014).
Fracanzani, A. L. et al. Gallstone Disease Is Associated with More Severe Liver Damage in Patients with Non-Alcoholic Fatty Liver Disease. Plos One 7, e41183 (2012).
Targher, G. & Byrne, C. D. G. Disease and Increased Risk of Ischemic Heart Disease: Causal Association or Epiphenomenon? Arteriosclerosis, thrombosis, and vascular biology 35, 2073–2075, https://doi.org/10.1161/atvbaha.115.306339 (2015).
Aune, D. & Vatten, L. J. Diabetes mellitus and the risk of gallbladder disease: A systematic review and meta-analysis of prospective studies. Journal of diabetes and its complications 30, 368–373, https://doi.org/10.1016/j.jdiacomp.2015.11.012 (2016).
Graham, I. et al. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representa). European journal of cardiovascular prevention and rehabilitation: official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology 14(Suppl 2), S1 (2007).
Murphy, M. O. & Loria, A. S. Sex-Specific Effects of Stress on Metabolic and Cardiovascular Disease: Are women at a higher risk? American Journal of Physiology Regulatory Integrative & Comparative Physiology, ajpregu.00185.02016 (2017).
Mendez Sanchez, N., Uribe Esquivel, M., Jessurun Solomou, J., Cervera Ceballos, E. & Bosques Padilla, F. [Epidemiology of gallstone disease in Mexico]. Revista de investigacion clinica; organo del Hospital de Enfermedades de la Nutricion 42(Suppl), 48–52 (1990).
Amigo, L. et al. Cholecystectomy increases hepatic triglyceride content and very-low-density lipoproteins production in mice. Liver International Official Journal of the International Association for the Study of the Liver 31, 52–64 (2011).
Almond, H. R. et al. Bile acid pools, kinetics and biliary lipid composition before and after cholecystectomy. N Engl J Med 289, 1213–1216 (1973).
Roda, E. et al. Enterohepatic circulation of bile acids after cholecystectomy. Gut 19, 640 (1978).
Zweers, S. J. et al. The human gallbladder secretes fibroblast growth factor 19 into bile: towards defining the role of fibroblast growth factor 19 in the enterobiliary tract. Hepatology 55, 575 (2012).
Keren, N. et al. Interactions between the intestinal microbiota and bile acids in gallstones patients. Environmental microbiology reports 7, 874–880, https://doi.org/10.1111/1758-2229.12319 (2015).
Acknowledgements
We acknowledge that the Second Affiliated Hospital of Wenzhou Medical University for supporting this research.
Author information
Authors and Affiliations
Contributions
Lai lai Fan and Zhi juan Dai designed the study. Lai lai Fan and Bai hui Chen completed the extraction and analysis of data. Zhi juan Dai reviewed the results. Lai lai Fan and Zhi juan Dai wrote the report. All authors approved the final version of the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fan, L.l., Chen, B.h. & Dai, Z.j. The relation between gallstone disease and cardiovascular disease. Sci Rep 7, 15104 (2017). https://doi.org/10.1038/s41598-017-15430-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-15430-5
This article is cited by
-
The association between the volume of the gallbladder based on sonographic findings and demographical data in the PERSIAN Guilan cohort study (PGCS)
BMC Research Notes (2023)
-
Gallbladder disease is associated with the risk of cardiovascular disease among Uyghurs in Xinjiang: a prospective cohort study
BMC Public Health (2023)
-
Impact of cholecystectomy on acute coronary syndrome according to metabolic condition: a nationwide population-based cohort study
Scientific Reports (2023)
-
Cholecystectomy reduces the risk of myocardial and cerebral infarction in patients with gallstone-related infection
Scientific Reports (2022)
-
C-reactive protein in gallbladder diseases: diagnostic and therapeutic insights
Biophysics Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.