Abstract
Globally, one third of prevalent chronic hepatitis B (CHB) virus infection (HBV) occurred in China. Assessing the prevalence of CHB infesction and status of HBV-related services among pre-conception women will provide insight into risks of mother to child transmission (MTCT). A cross-sectional analysis of data from the National Free Pre-pregnancy Checkups (NFPC) program in 2010–2014 was conducted. A standardized questionnaire which collected demographic information and enzyme-linked immunosorbent assays (ELISA) which tested serological HBV markers were applied. A total of 16,051,850 rural women aged 15–49 years were included. 5.2% of women were infected with CHB, among whom, 28.6% were also hepatitis B e antigen (HBeAg) positive. The most CHB concentrated places were distributed in southeastern coastal provinces. Women born after 1992 did not experience a higher level of vaccine-induced immunity compared to those born before 1992. Nine in ten rural women with CHB were not aware of their HBV status and a very small proportion of women (0.22%) had received antiviral treatment. Our data demonstrated an overall high-intermediate burden of CHB. Heterogeneity of geographic distribution, high proportion of HBeAg, insufficient awareness of HBV status, and low access to HBV treatment are challenges for preventing the MTCT.
Similar content being viewed by others
Introduction
Chronic hepatitis B (CHB) virus (HBV) infection remains a severe problem worldwide especially in China1. An estimated 240–400 million persons had chronic HBV infection and the annual mortality from HBV-related complications including cirrhosis and hepatocellular carcinoma was 600,000 persons2,3. The most recent national sero-epidemiological survey in 2006 reported 7.2% of CHB in the Chinese population with an estimated 90 million people with CHB4, which accounted for 22–38% of the global burden of CHB. Evaluating the prevalence of CHB in key populations in China is critical to inform better prevention policies. The Chinese government recommended routine hepatitis B immunization for newborns in 1992, included it in the National Immunization Program as a free vaccine in 2002 and removed all of the administration fees in 20055. Investigating the prevalence of CHB would also help to evaluate the potential impact of this national HBV vaccination policy.
Rural women in China often had poor education and limited resources6 and were likely to resemble populations from other low and middle income countries in terms of education and available resources. Knowing their status of CHB and status of hepatitis B-related services will have important implications onglobal control of CHB. Worldwide, most of CHB has been acquired perinatally or in early childhood7, and up to 50% of new HBV infections were obtained through mother-to-child-transmission (MTCT) in China8. Identifying women with CHB prior to their pregnancy and gaps of policy implementation are crucial for the prevention of MTCT.
In this study, we reported the prevalence of CHB, geographic distribution and status of hepatitis B-related services among 16 million rural women aged 15–49 years in China, evaluated the effect of the national HBV immunization program on serological outcome in women born before and after 1992 and main focused on challenges on mother to child transmission of HBV.
Methods
Study design and study population
A cross-sectional study was conducted, using data from the National Free Pre-pregnancy Checkups (NFPC) program. Women aged 15–49 years who planned to conceive and attended NFPC between January 2010 and December 2014 were included. It is noted that a previous report using 2014 data has demonstrated the burden of HBV in this population. Here we used expanded samples from 2010–2014 to see if the conclusions remain and to explore other prioritized questions9. The NFPC, supported by the Chinese National Health and Family Planning Commission and Ministry of Finance, is a nationwide free preconception medical examination service for rural couples in China. It was first carried out in 100 counties of 18 provinces in 2010 in China, and was gradually extended to 2790 counties in 2013 with high coverage across the country. Since the NFPC is a free program aiming to improve the health of pregnancy and reduce birth defects, and women voluntarily came to obtain the service, the selection of study population would belong to the convenience sampling.
All couples who planned to conceive were enrolled by trained staff, and informed consent was obtained before the checkups. A face-to-face interview was then carried out by qualified nurses using a standardized procedure. Socioeconomic information including age, occupation, education, ethnicity, and residence was collected by a structured questionnaire. A 5 mL-blood sample was obtained and tested for HBV serologic markers at local laboratories. Tests included hepatitis B surface antigen (HBsAg), hepatitis B surface antibody (anti-HBs), hepatitis B e antigen (HBeAg), hepatitis B e antibody (anti-HBe) and hepatitis B core antibody (anti-HBc) using ELISA kits approved by the China Food and Drug Administration. Quality control was completed by the National Center of Clinical Laboratories with reagents produced by Abbott (Abbott Park, IL, USA), as the reference standard. Study protocols and forms were approved by the Institutional Research Review Board at the National Research Institute for Family Planning. The study was carried out under the guidance of the protocols strictly.
Definition of outcomes
The primary outcomes included the prevalence of chronic HBV infection, defined as positivity of HBsAg (less commonly indicative of acute infection)2, self-reported awareness of HBV status, and initiation of antiviral therapy against HBV. Secondary outcomes comprised past/present HBV infection (positivity of anti-HBc), high infectivity (positivity of HBeAg) and vaccine-induced immunity (isolated positivity of anti-HBs).
Definition of covariates
Participants’ characteristics included: age (15–19, 20–24, 25–29, 30–34, 35–39, 40–44 and 45–49 years) education level (illiterate, primary school, junior school, senior school and college or higher), ethnic group (Han and others), migrant population (yes, no), region of residence (eastern, central and western)10, a self-reported history of HBV immunization (yes, no) and parity (0, ≥ 1). To explore the impact of the national HBV immunization program beginning in 1992, study population were divided into a cohort born before 1992 and a cohort born after 1992.
Statistical analysis
We present the distribution of participants’ socio-demographic characteristics using proportions. The prevalence of each outcome and 95% confidence interval (CI) were calculated in the entire population, as well as in subgroups. We employed Poisson regression models to assess the crude and adjusted prevalence ratio (PR) of outcomes. Adjusted variables for awareness of HBV status were age, education, ethnic group, occupation, migrant population, region and parity. The effect of the national HBV immunization program was analyzed by comparing the difference of each serological outcome in women born before and after 1992. In addition, to describe the geographical distribution, we estimated the prevalence of CHB in each of 2,421 counties after exclusion of counties with no data or sample size less than 100 (assume unstable), and then county-specific prevalence of HBsAg was mapped in four tiers (low: <2%, low intermediate: 2–4%, high intermediate: 5–8% and high: >8%) using ArcGIS 10.3 (ESRI, Redlands, California, USA).A two-tailed p value < 0.05 was considered to reach statistical significance. SPSS version 20.0 (IBM Inc., Armonk, NY) and Stata 13.1 (College Station, Texas, USA) were used for all analyses.
Results
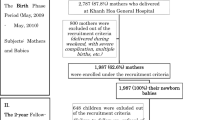
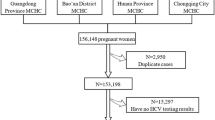
Figure 1 presents a flowchart of the study population and analytical scheme. Between 2010 and 2014, a total of 17,066,759 women were recorded in the NFPC program. 16,830,893 (98.6%) of them completed HBV serological testing, and 16,051,850 (94.1%) women with complete demographic information were included in the analysis. The majority of 16,051,850 women were aged 20–29 years (77.3%), Han ethnicity (88.1%), farmers (77.5%), and non-migrant population (96.6%), and had education of junior school (65.0%). Locations where participants currently live were approximately evenly distributed across the eastern (33.9%), central (37.6%) and western (28.5%) regions. 26.8% of women reported a history of HBV immunization (Table 1).
The crude prevalence of CHB among all women was 5.2% and age-adjusted prevalence based on population weight from China 2010 Census Data is 5.0% (Table 2). The prevalence of HBeAg among women with CHB was 28.6%. Of the total 2,421 counties across China, there are 439 (18.1%) high, 463 (19.1%) high-intermediate, 1102 (45.5%) low-intermediate, and 417 (17.2%) low CHB endemic counties, and the top 10 county-specific prevalence of HBsAg ranged from 17.6% to 22.4%. The majority of high endemic counties were concentrated in five provinces including Guangxi, Guangdong, Fujian, Hainan and Jiangxi (Fig. 2). Women who were born after 1992 had a lower prevalence of CHB (4.7% vs 5.3%), past/present HBV infection (8.3% vs 10.5%), and vaccine-induced immunity (26.2% vs 29.3%) compared to those born before1992 Table 3).
The prevalence of chronic hepatitis B in different geographic regions. The Fig. 2 was created using ArcGIS 10.3 (ESRI, Redlands, California, USA). We used the China 2010 Census GIS shapefile as the basic layer, and linked it with the count-level prevalence of HBsAg, collected by National Free Pre-conception Check-up (NFPC) program, by county name. Then the burden of HBsAg was displayed into predefined four tiers with four different colors. The China 2010 Census GIS shapefile is derived from the China Data Center production: 2010 China County Population Census Data with GIS Maps (Version I). This dataset is in GBK encoding. Publication date: May 2013. Harvard Acquisition date: Jan 2014. http://hollis.harvard.edu/primo_library/libweb/action/dlDisplay.do?vid=HVD&search_scope=default_scope&docId=HVD_ALEPH013684533&fn=permalink.
Of 837,372 women with CHB, only 85,725 (10.2%) were aware of their HBV status. Age 15–24 years and 30–49 years (vs 25–29 years), education of senior school or less (vs college or higher), living in eastern or central region (vs western region) and zero parity (vs ≥ 1) were significantly associated with a lower prevalence of awareness of HBV status (Table 4). 1874 (0.22%) women had received some therapies related to hepatitis B. Using alanine transaminase (ALT) > 2 upper limits of normal (2 ULN = 76 U/L) and HBeAg positivity as criteria for the initiation of treatment for CHB10,11, 7.4% (62,343/837,372) women with CHB actually need antiviral therapy for their active HBV infection. The most common antiviral drug used was Telbivudine (16.1%, 301/1,874), followed by Lamivudine (11.8%, 222/1,874), Adefovir (10.7%, 201/1,874), Entecavir (5.3%, 100/1,874), Peg-IFN-2a (2.0%, 37/1,874) and Tenofovir (1.0%, 18/1,874).
Discussion
This study reports a high-intermediate burden of chronic HBV infection in a large sample of women aged 15–49 years from rural China who planned to conceive. Superimposed on this, the heterogeneity of geographic distribution and low vaccine induced immunity even among women born after 1992 when China began to recommend HBV vaccination, are barriers to prevention of MTCT of HBV infection. Most women (90%) with CHB were not aware of their status, and only a very small proportion of them had a history of antiviral therapy despite a substantial proportion (7.4%) who may qualify, which acts as additional barriers to prevent MTCT. Although CHB can be controlled with timely and careful monitoring and appropriate treatment, these data show that preventive education and access to the clinical care among rural women with CHB are not far from optimum.
The overall prevalence of CHB (5.2%) was lower than 8.7% in 20064 and 9.7% in 199212 in the same age groups, reported in two latest national HBV seros urveys. Also, the prevalence of CHB among rural men from the same data source was higher than rural women (7.0% vs 5.2%)13.
Geographically, 16% of provinces and 18% of counties in China still had high endemicity of HBV infection ( >8%) among rural women aged 15–49 years. The most HBV concentrated places are southeastern coastal provinces, including Guangxi, Guangdong, Fujian, Hainan, and Jiangxi. It is hard to distinguish whether individual factors, like low socio-economic status and inter-province migration14, or factors related to geographical locations, like historical HBV endemicity and higher risk of sexual transmission in these places, contribute to this aggregation. Besides figuring out contributing factors, preventive efforts, like screening and education, targeting on these clustered locations are recommended.
The Chinese government recommended HBV immunization for newborns in 1992. Because of high prices and unequal access to vaccines in early years15, people born before or close to 1992, would not benefit from this policy. Our results showed that even for women born after 1992, either overall immunity or vaccine-induced immunity against HBV did not improve compared to that of women born before 1992. Of note, women who reported a history of HBV immunization had a lower prevalence of CHB (4.4% vs 5.5%) and higher proportion of overall immunity (41.4% vs 31.3%) versus those without a self-reported history of HBV immunization. This reminds that although women missed their immunization at birth or early childhood, being vaccinated later in adulthood may still be protective.
The high proportion of positivity of HBeAg, an indication of high infectivity16, among women with chronic HBV infection could facilitate the risk of MTCT. Although administration of hepatitis B vaccination in conjunction with HBIG among newborns is highly effective to prevent transmission7,about 7% of infants born to mothers with high viral load, indicated by positivity of HBeAg, could still be infected with HBV17. Our data showed that 29% of rural women with CHB were also HBeAg positive. It means not only is the burden of CHB high, but women infected with CHB are at higher risk of transmitting the disease to others, like their future babies.
As outlined by WHO in 2015, in the management of chronic HBV infection7, being tested and diagnosed is the first step to link people to care. Those subjects with active hepatic inflammation should be linked to care and evaluated for antiviral therapy. Our results showed that nine in ten rural women with chronic HBV infection were not aware of their status and a very small proportion of women had received treatment (0.22%) despite more women in need of antiviral therapy (7.4%). A recent study showed that Tenofovir regimen in pregnant women during their pregnancy in conjunction with a standard newborn immunoprophylaxis could significantly decrease the rate of MTCT compared to group who only had a newborn immunoprophylaxis17. This suggests that decreasing viral load to a suppressed level among pregnant or prenatal women through antiviral treatment is key to add further protection from MTCT. However, rural women with CHB in this study had a very low rate of receiving antiviral treatment, which makes it impossible to suppress their viral load to a safe level and prevent MTCT effectively.
The data includes a very large sample of rural women who planned to conceive, who represent a critical reservoir for the continued MTCT of HBV in China. Also, this is the first study to evaluate the status of HBV care among rural women in China, which can inform better prevention and treatment service delivery. Limitations include inability of generalizing results to the entire population since the study population comprised only rural women from a convenience sample; a potential selection bias as women who participated in the study may differ from those who had not participated; lack of quantification of viral load and anti-HBs titer; lack of continuous monitoring to confirm eligibility of antiviral treatment; a recall bias of self-reported awareness of HBV status and antiviral treatment experience.
In conclusion, our data demonstrate a high-intermediate burden of chronic HBV infection in China. The heterogeneity of geographic distribution, high proportion of HBeAg, insufficient awareness of HBV status, and low rate of antiviral treatment are deteriorating health among rural women with CHB and they will also be reservoirs for the continued MTCT of HBV in China. Public health efforts to improve awareness of HBV, to provide a catch-up vaccination and to increase uptake of appropriate antiviral treatment should be scaled up immediately.
References
Liu, J. & Fan, D. Hepatitis B in China. Lancet (London, England) 369, 1582–1583 (2007).
Roberts, H. et al. Prevalence of chronic hepatitis B virus (HBV) infection in U.S. households: National Health and Nutrition Examination Survey (NHANES), 1988-2012. Hepatology (Baltimore, Md.) 63, 388–397 (2016).
Schweitzer, A., Horn, J., Mikolajczyk, R. T., Krause, G. & Ott, J. J. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet (London, England) 386, 1546–1555 (2015).
Liang, X. et al. Reprint of: Epidemiological serosurvey of Hepatitis B in China–declining HBV prevalence due to Hepatitis B vaccination. Vaccine 31(Suppl 9), J21–28 (2013).
Liang, X. et al. Evaluation of the impact of hepatitis B vaccination among children born during 1992-2005 in China. The Journal of infectious diseases 200, 39–47 (2009).
Tang, S. et al. Tackling the challenges to health equity in China. Lancet (London, England) 372, 1493–1501 (2008).
World Health Organization. Who Guidelines for the Prevention, Care and Treatment of Persons with Chronic Hepatitis B Infection. (World Health Organization, 2015).
Thio, C. L., Guo, N., Xie, C., Nelson, K. E. & Ehrhardt, S. Global elimination of mother-to-child transmission of hepatitis B: revisiting the current strategy. The Lancet Infectious Diseases 15, 981–985 (2015).
Xin, X. et al. Seroepidemiological survey of hepatitis B virus infection among 764,460 women of childbearing age in rural China: A cross-sectional study. J Clin Virol 81, 47–52 (2016).
Liu, J. et al. Seroepidemiology of hepatitis B virus infection in 2 million men aged 21-49 years in rural China: a population-based, cross-sectional study. Lancet Infect Dis1 6, 80–86 (2016).
Sarin, S. K. et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatology international 10, 1–98 (2016).
Xia, G.-L. et al. Prevalence of hepatitis B and C virus infections in the general Chinese population. Results from a nationwide cross-sectional seroepidemiologic study of hepatitis A, B, C, D, and E virus infections in China, 1992. International Hepatology Communications 5, 62–73 (1996).
Zhang, L. et al. Status of HBsAg seroprevalence in 15 million rural couples in China: a cross-sectional study. Scientific reports 7, 42822 (2017).
Yang, Y. et al. Prevalence of hepatitis B and knowledge about hepatitis B among migrant workers in shandong province, china: a cross-sectional study. Iranian Red Crescent medical journal 17, e26725 (2015).
Cui, F. et al. Preventing hepatitis B though universal vaccination: reduction of inequalities through the GAVI China project. Vaccine 31(Suppl 9), J29–35 (2013).
Ott, J. J., Stevens, G. A. & Wiersma, S. T. The risk of perinatal hepatitis B virus transmission: hepatitis B e antigen (HBeAg) prevalence estimates for all world regions. BMC infectious diseases 12, 131 (2012).
Pan, C. Q. et al. Tenofovir to Prevent Hepatitis B Transmission in Mothers with High Viral Load. The New England journal of medicine 374, 2324–2334 (2016).
Acknowledgements
We thank health workers and countless participants throughout 31 provinces in NFPC for great efforts and collaboration. This study was supported by National Key Research and Development Program (No. 2016YFC1000307 and No. 2016YFC1000300) from Ministry of science and technology of the people’s republic of China.
Author information
Authors and Affiliations
Contributions
Yuanyuan Wang, Hong Zhou and Long Zhang framed the concept of the study. Yuanyuan Wang and Hong Zhou contributed to the study design, analysis and composing the manuscript. Yuanyuan Wang, Hong Zhou, Long Zhang,QiuyueZhong, Yanjie Huang, Kenrad Nelson, Anqi Wang and Xiaoli Liu searched the literature, interpreted the results, and helped to revise the draft. Qiaomei Wang, Haiping Shen and Man Zhang led the data collection and laboratory testing monitoring. Yiping Zhang, Donghai Yan, Zuoqi Peng, Ya Zhang, Xiaona Xin, Hongguang Zhang, Jun Zhao, Yan Wang, Ying Yang, Yuan He and Jihong Xu were responsible for data collection and management. Yan Wang and Xu Ma supervised the study process and provided overall guidance. Yuanyuan Wang and Zhouhong contributed equally. All authors contributed to the writing of the report.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Zhou, H., Zhang, L. et al. Prevalence of chronic hepatitis B and status of HBV care among rural women who planned to conceive in China. Sci Rep 7, 12090 (2017). https://doi.org/10.1038/s41598-017-12005-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12005-2
This article is cited by
-
The prevalence of hepatitis B in Chinese general population from 2018 to 2022: a systematic review and meta-analysis
BMC Infectious Diseases (2024)
-
The effectiveness of 20 μg hepatitis B vaccine used for the prevention of HBV vertical transmission
Scientific Reports (2022)
-
Asian Pacific association for the study of liver (APASL) guidelines: hepatitis B virus in pregnancy
Hepatology International (2022)
-
Prevalence of congenital microcephaly and its risk factors in an area at risk of Zika outbreaks
BMC Pregnancy and Childbirth (2021)
-
Maternal age and educational level modify the association between chronic hepatitis B infection and preterm labor
BMC Pregnancy and Childbirth (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.