Abstract
Obesity, overweight and autism spectrum disorder (ASD) remain serious public health problems. Although lots of studies have recently explored the association among obesity, overweight and ASD, the findings are inconsistent. Thus, we conducted a meta-analysis of epidemiological studies to examine the association among obesity, overweight and ASD. PubMed, Embase, and the Cochrane Library were used for literature searches to identify eligible studies published in English before November 15, 2016. Relevant studies estimating the association among obesity, overweight and ASD were included. Fifteen studies encompassing 49,937,078 participants and 1,045,538 individuals with ASD were included in this study. A random effects model was chosen to synthesize the effect sizes of individual studies. The prevalence of obesity was significantly higher in individuals with ASD than in controls (OR = 1.84, 95% confidence interval [CI]: 1.37–2.48, P < 0.001). However, the prevalence of overweight in individuals with ASD was not significantly different from that in controls (OR = 1.07, 95% CI: 0.83–1.38, P = 0.62). Both sensitivity analysis and publication bias testing revealed that the findings were robust. The meta-analysis showed a significant association between obesity and ASD. However, no significant association was identified between overweight and ASD.
Similar content being viewed by others
Introduction
Obesity is a significant public health problem that affects 17% of children and 35% of adults in the United States1. Obesity can cause health problems including sleep-disordered breathing, orthopedic problems, hypertension, type 2 diabetes, and dyslipidemia2,3,4,5,6,7. Obesity is defined as an age-adjusted and gender-specific body mass index at or over the 95th percentile. Overweight is considered an age-adjusted and gender-specific body mass index between the 85th and 95th percentiles. Obesity or overweight harms psychosocial functions and is associated with significant societal and familial economic burdens2,8. Obese or overweight children are more susceptible to isolation and bullying than normal weight children8. Thus, obesity and overweight are becoming severe social issues and have a significant influence on quality of life and independent functioning.
Recently, scientists have reported that obesity and overweight are more likely to be related to psychiatric disorders in children, such as attention deficit/hyperactivity disorder and autism spectrum disorder (ASD)9,10. ASD is a complex disorder which manifests as difficulty in social interactions and communication, along with restrictive and repetitive behaviors. ASD is a complex and heterogeneous disorder that is due to the interaction effect between genetic vulnerability and environmental factors. The overall prevalence of ASD is 1 in 68 children11. Additionally, ASD is co-morbid with mental health disorders such as anxiety disorder and attention deficit/hyperactivity disorder but not with medical condition such as asthma and allergy12,13,14,15. Since ASD is a serious public health problem, scientists have attempted to identify biomarkers to achieve an earlier diagnosis and enable earlier treatment. We and other researchers have shown that biomarkers such as brain-derived neurotrophic factor and glutamate are sensitive markers for the early diagnosis of ASD and bipolar disorder16,17,18,19. However, specific biomarkers relevant only to ASD are still needed. Furthermore, specific and effective treatment for ASD in the clinic is scarce. ASD begins at an early age and lasts throughout the lifespan, which increases the economic burden on both family and society. Thus, ASD is also a significant global public health problem.
Individuals with ASD have several issues, including food selectivity, gastrointestinal symptoms, less physical activity, and medication use, which may result in abnormal anthropometric measurements20,21,22,23. Recently, some studies have focused on the association among obesity, overweight and ASD9,24,25,26. However, the findings are inconsistent. Some scientists have reported that BMI in individuals with ASD is not different from that in controls9,24, while other scientists have reported the prevalence of obesity and overweight is higher in individuals with ASD than in controls25,26. Therefore, we performed a meta-analysis to examine the association among obesity, overweight and ASD. We believe that a comprehensive evaluation of this critical public health problem may promote efforts to develop adequate interventional strategies in this population.
Results
Literature search
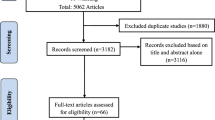
We initially identified a total of 2,720 potential articles, of which 936 were from PubMed, 1,670 were from Embase, 109 were from the Cochrane Library and 5 were from screening the references in the included articles. We identified 72 articles after excluding 421 duplicate articles, 2,177 irrelevant articles, 6 reviews and 44 letters/meetings. Then, those 72 articles were screened carefully. Eleven articles were excluded because their topics were irrelevant. Twenty-three articles were excluded because they lacked a control comparison group. Seventeen articles were excluded because they did not provide sufficient data and 6 articles were excluded because of overlap. Ultimately, 15 articles encompassing 49,937,078 participants and 1,045,538 individuals with ASD were included in this study. The flow diagram of the literature search is shown in Fig. 1.
Flow diagram of the literature search. A total of 2,720 potential studies were initially identified in databases. 72 studies were identified after excluding 421 duplicate studies, 2,177 irrelevant studies, 6 reviews and 44 letters/meetings. Then, 57 studies were removed after a careful screening. Ultimately, 15 studies were adopted in this meta-analysis.
Study characteristics
The extracted data from the fifteen studies are shown in Table 1. Fifteen studies were published between 2010 and 20169,24,25,26,27,28,29,30,31,32,33,34,35,36,37. Four studies were case-control24,27,31,33 and eleven studies were cross-section9,25,26,28,29,30,32,34,35,36,37. The studies encompassed a total of 49,937,078 participants and 1,045,538 individuals with ASD. Ten studies were carried out in the United States24,25,26,27,29,30,34,35,36,37, two in Brazil9,31, one in Turkey32, one in Spain33, and one in China28. The sample sizes ranged from 4033 to 986,35230 individuals with ASD and from 199 to 48,598,46630 controls. Additionally, the mean ages of the samples ranged from 2 years old25,27,34 to 29.4 ± 12.1 years old35.
For the method of ascertaining ASD, four studies used parental reports26,29,30,36, and the other studies based on their diagnoses on the Diagnostic and Statistical Manual (DSM-IV)31,32,34, DSM-V9,28,32, Social Communication Questionnaire (SCQ)24, International Classification of Diseases, 9th Revision (ICD-9)25, International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM)27,35, Autism Diagnostic Interview-Revised (ADI-R)24,33,37, Autism Diagnostic Observation Schedule (ADOS)24,34, and Autism Diagnostic Observation Schedule-Generic (ADOS-G)33. For the method of ascertaining BMI, three studies included parentally reported data26,30,36, ten studies objectively measured the data9,24,27,28,29,31,32,33,34,37, and two studies extracted the information from the participants’ medical records25,35.
The prevalence of obesity and overweight in individuals with ASD
The prevalence of obesity was significantly higher in individuals with ASD than in controls (OR = 1.84, 95% confidence interval [CI]: 1.37–2.48, P < 0.001). Significant heterogeneity was found across studies (I2 = 96.0%, P < 0.001) (Fig. 2). However, the prevalence of overweight in individuals with ASD was not significantly different from that in controls (OR = 1.07, 95% CI: 0.83–1.38, P = 0.62). Significant heterogeneity was found across studies (I2 = 78.0%, P < 0.001) (Fig. 3).
Forest plot of odds ratios for the association between obesity and ASD. Fourteen studies encompassing 1,045,485 individuals with ASD and 48,891,482 controls were included. The prevalence of obesity was higher in individuals with ASD than in controls. There was a significant association between obesity and ASD.
Forest plot of odds ratios for the association between overweight and ASD. Thirteen articles encompassing 995,269 individuals with ASD and 48,632,660 controls were included. The prevalence of overweight was not significantly different between individuals with ASD and controls. There was no significant association between overweight and ASD.
Quality evaluation
As presented in Table 2, eleven studies were considered high quality, while four studies were considered moderate quality. The mean score of all studies was 7.1.
Publication bias
The funnel plot showed slight asymmetry (Figs 4 and 5). However, Begg’s test (P = 0.913) and Egger’s test (P = 0.925) showed no significant publication bias among the studies examining the association between obesity and ASD. Similarly, Begg’s test (P = 0.246) and Egger’s test (P = 0.773) showed no significant publication bias among the studies examining the association between overweight and ASD.
Subgroup analysis and sensitivity analysis
Subgroup analyses by study design, geographic locations, method of ascertaining of ASD, method of ascertaining BMI, and adjustment factors for age and gender were shown in Table 3.
Among the studies examining the association between obesity and ASD, the tests for subgroup differences were not significant in the subgroup analyses by study design, geographic locations, method of ascertaining ASD, method of ascertaining BMI, and adjustment factors for age and gender.
Among the studies examining the association between overweight and ASD, the tests for subgroup differences showed significant different in the subgroup analyses by study design, geographic locations, and method of ascertaining BMI.
The sensitivity analysis was conducted by removing each study individually and comparing the results from the rest of studies with the overall result. The results showed that there was consistently a higher prevalence of obesity in individuals with ASD than in controls, while there was no significant different in the prevalence of overweight between individuals with ASD and controls. The omission of any single study did not change the overall result.
Discussion
This meta-analysis included 15 studies with a total of 49,937,078 participants and 1,045,538 cases of ASD. The results showed that obesity but not overweight was associated with ASD.
In this study, we adopted a random-effects model to synthesize the effect sizes of individual studies because significant heterogeneity between studies existed. Sensitivity analysis revealed the findings were robust. In addition, both Begg’s and Egger’s tests indicated no significant publication bias existed.
An association between obesity and ASD was confirmed in this study. These findings are supported by previous studies. First, individuals with ASD often have eating problems, such as food selectivity and specialized dietary habits, which make healthy dietary interventions less effective38,39. Second, individuals with ASD spend less time on physical activities and more time on sedentary activities29. They also have difficulty in participating in standard obesity prevention initiatives due to behavioral problems. Third, individuals with ASD have more chances to be treated with various antipsychotic medications, which are known to be associated with weight gain40,41. Fourth, individuals with ASD also have comorbidities associated with obesity, such as sleep problems, gastrointestinal disorders, ADHD13,23,42,43. Finally, some individuals with ASD have been reported to have 16p11.2 or 11p14.1 microdeletions, which encompass genes related to obesity susceptibility44,45. These results indicated that obesity is related to ASD, which is consistent with our findings.
However, we found significant heterogeneity in this meta-analysis. Thus, we performed subgroup analyses to find the source of heterogeneity. But we could not find the source of heterogeneity among the studies examining the association between obesity and ASD (Table 3). Residual confounding factors such as different ages and genders across studies need to be considered. In addition, we found three factors that may explain the heterogeneity among the studies examining the association between overweight and ASD. First, the overall result indicated that there was no difference in the prevalence of overweight between individuals with ASD and controls in the USA samples, whereas the prevalence of overweight in individuals with ASD was lower than that in controls in the non-USA samples (Table 3). The result may be because of different genetic backgrounds and lifestyles. Second, different study designs (case-control or cross-section) were a cause of the heterogeneity (Table 3). Third, the different methods of ascertaining BMI (objectively measured, extracted from medical records or parentally reported) used in these studies contributed to heterogeneity (Table 3). The measures of ascertaining BMI in several studies biased the results because the data were collected from parental reports rather than objectively measured.
Although the heterogeneity is high, the analysis has certain obvious advantages. First, we are the first to conduct a meta-analysis to explore the association among obesity, overweight and ASD. Second, the meta-analysis included a huge amount of samples, making it more likely to draw a reasonable conclusion about obesity and overweight in ASD. Third, the sensitivity analysis showed that removing any study did not change the final results, suggesting that our findings were robust. Finally, publication bias was not found, which increased the reliability of the findings.
However, some limitations existed in this study. First, weight status was reported by parents in three studies. Therefore, the BMI may not be accurate in those studies. Future work should attempt to have the BMI measured objectively by trained clinicians. Second, there was significant heterogeneity across studies, which may reduce the conclusiveness of the results. Finally, adjustments were not made for confounding factors including dietary habits, physical activity participation, family history of obesity and secondary conditions. ASD is a heterogeneous disorder. Secondary conditions, including physical status, mental health status, developmental delay, intellectual and learning disabilities, attention deficit/hyperactivity disorder, IQ and drugs use might influence the association between obesity and ASD30. Therefore, future research should systematically adjust for a broad set of possible confounding factors.
In conclusion, this meta-analysis showed a significant association between obesity and ASD. However, no significant association was identified between overweight and ASD. Further prospective studies with more accurate measures of weight status and better control of confounding factors are warranted.
Materials and Methods
Strategy of literature search
We performed a literature search of PubMed, Embase and the Cochrane Library for the potential articles. The search was restricted to articles published before November 15, 2016. The search terms were as follows: [“ASD” OR “autism spectrum disorder” OR “autistic disorder” OR “autism” OR “Asperger syndrome” OR “pervasive developmental disorder”] and [“obesity” OR “obese” OR “overweight” OR “adipose” OR “adiposity” OR “body weight” OR “body mass index” OR “BMI”]. Furthermore, we searched the references of the related articles to attain other potential studies.
Only studies published in English were considered. In addition, we only considered studies performed on human. We reviewed the titles and abstracts to exclude the irrelevant studies. Then, we read the text carefully based on the inclusion criteria. If two authors reached inconsistent conclusions about inclusion/exclusion, a third author would be asked to make a decision.
Study selection criteria
Any study that reached all the following criteria was included: (1) assessing the association among obesity, overweight and ASD; (2) reporting the raw data or OR with 95% CI; and (3) case-control, cohort or cross-sectional designs.
The following studies were excluded: (1) reviews, non-human studies, case reports, case-only studies, or meetings/letters; and (2) overlapping data.
Data extraction
The data were extracted from the studies as follows: first author’s surname, year of publication, country, study design, numbers of cases and controls, number of males, age, methods of ascertaining ASD and BMI, outcome variable and adjusted confounders. If multiple studies contained overlapping data from the same population, the one with the largest sample size was adopted.
Quality evaluation
We conducted Newcastle-Ottawa Scale (NOS) to evaluate the quality of the studies. The NOS evaluated the following aspects: selection of participants, comparability, exposure of participants, and outcome. The score ranged from 0 to 9. Scores of 7–9 indicate high quality, scores of 4–6 indicate medium quality and scores of 0–3 indicate low quality. When raters disagreed, the inconsistencies were settled by discussion.
Statistical analysis
We combined the effect sizes by using ORs to assess the association among obesity, overweight and ASD. We calculated the ORs by using a fixed-effects model or a random-effects model. If the heterogeneity was low, the fixed-effects model was used. If the heterogeneity was high, the random-effects model was chosen. I2 and the Q statistic were adopted to evaluate the heterogeneity. The heterogeneity was divided into the following levels according toI2 value: low (I2: 25%-50%), moderate (I2: 50–75%) and high (I2: >75%). The Q statistic was viewed significant if P < 0.1.
The funnel plot was visually inspected to evaluate publication bias. In addition, both Begg’s and Egger’s tests were conducted to evaluate publication bias. Publication bias was viewed significant if P < 0.05. Subgroup analyses were conducted to identify the sources of heterogeneity based on study design (case-control or cross-section), geographic locations (USA or non-USA), methods of ascertaining ASD (parental report or standard assessment), methods of ascertaining BMI (objective measurement or other methods), and adjustment factors for age and gender (yes or no).
Sensitivity analysis was conducted by individually omitting one study from statistical analysis. Then, the ORs and 95% CIs of the remaining studies were compared to the overall result. Statistical analyses were conducted with Stata 12.0 (Stata Corp, College Station, Texas, USA).
References
Ogden, C. L., Carroll, M. D., Kit, B. K. & Flegal, K. M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 311, 806–814 (2014).
Wang, Y. C., McPherson, K., Marsh, T., Gortmaker, S. L. & Brown, M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 378, 815–825 (2011).
Wang, S. et al. Association between obesity indices and type 2 diabetes mellitus among middle-aged and elderly people in Jinan, China: a cross-sectional study. BMJ Open. 6, e012742 (2016).
Su, M. S. et al. Obesity in children with different risk factors for obstructive sleep apnea: a community-based study. Eur J Pediatr. 175, 211–220 (2016).
Kropa, J. et al. High prevalence of obesity and high blood pressure in urban student-athletes. J Pediatr. 178, 194–199 (2016).
Hoffmann, S., Stucker, R. & Rupprecht, M. Orthopedic problems in overweight and obese children. Klin Padiatr. 228, 55–61 (2016).
Friedemann, C. et al. Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ. 345, e4759 (2012).
Bacchini, D. et al. Bullying and victimization in overweight and obese outpatient children and adolescents: an Italian multicentric study. PloS One. 10, e0142715 (2015).
Kummer, A. et al. Frequency of overweight and obesity in children and adolescents with autism and attention deficit/hyperactivity disorder. Rev Paul Pediatr. 34, 71–77 (2016).
Cortese, S. et al. Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiat. 173, 34–43 (2016).
Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill Summ. 63, 1–21 (2014).
Zheng, Z. et al. Association between asthma and autism spectrum disorder: ameta-analysis. PloS One. 11, e0156662 (2016).
Antshel, K. M., Zhang-James, Y. & Faraone, S. V. The comorbidity of ADHD and autism spectrum disorder. Expert Rev Neurothe. 13, 1117–1128 (2013).
Lyall, K., V de Water, J., Ashwood, P. & Hertz-Picciotto, I. Asthma and allergies in children with autism spectrum disorders: results from the CHARGE study. Autism Res. 8, 567–574 (2015).
van Steensel, F. J., Bogels, S. M. & Perrin, S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clin Child Fam Psychol Rev. 14, 302–317 (2011).
Zheng, Z., Zhu, T., Qu, Y. & Mu, D. Blood glutamate levels in autism spectrum disorder: a systematic review and meta-analysis. PloS One. 11, e0158688 (2016).
Zheng, Z. et al. Peripheral brain-derived neurotrophic factor in autism spectrum disorder: a systematic review and meta-analysis. Sci Rep. 6, 31241 (2016).
Qin, X. Y. et al. Association of peripheral blood levels of brain-derived neurotrophic factor with autism spectrum disorder in children: a systematic review and meta-analysis. JAMA Pediatr. 170, 1079–1086 (2016).
Munkholm, K., Vinberg, M. & Kessing, L. V. Peripheral blood brain-derived neurotrophic factor in bipolar disorder: a comprehensive systematic review and meta-analysis. Mol Psychiatry. 21, 216–228 (2016).
Pan, C. Y. et al. Objectively measured physical activity and health-related physical fitness in secondary school-aged male students with autism spectrum disorders. Phys Ther. 96, 511–520 (2016).
Madden, J. M. et al. Psychotropic medication use among insured children with autism spectrum disorder. J Autism Dev Disord. 47, 144–154 (2017).
Ma, N. S., Thompson, C. & Weston, S. Brief report: scurvy as a manifestation of food selectivity in children with autism. J Autism Dev Disord. 46, 1464–1470 (2016).
Ferguson, B. J. et al. Psychophysiological associations with gastrointestinal symptomatology in autism spectrum disorder. Autism Res. 10, 276–288 (2017).
Barnhill, K. et al. Growth status of children with autism spectrum disorder: a case-control study. J Hum Nutr Diet. 30, 59–65 (2016).
Broder-Fingert, S., Brazauskas, K., Lindgren, K., Iannuzzi, D. & Van Cleave, J. Prevalence of overweight and obesity in a large clinical sample of children with autism. Acad Pediatr. 14, 408–414 (2014).
Rimmer, J. H., Yamaki, K., Lowry, B. M., Wang, E. & Vogel, L. C. Obesity and obesity-related secondary conditions in adolescents with intellectual/developmental disabilities. J Intellect Disabil Res. 54, 787–794 (2010).
Shedlock, K. et al. Autism spectrum disorders and metabolic complications of obesity. J Pediatr. 178, 183–187 (2016).
Liu, X. et al. Correlation between nutrition and symptoms: nutritional survey of children with autism spectrum disorder in Chongqing, China. Nutrients. 8 (2016).
Healy, S., Haegele, J. A., Grenier, M. & Garcia, J. M. Physical activity, screen-time behavior, and obesity among 13-year olds in Ireland with and without autism spectrum disorder. J Autism Dev Disord. 47, 49–57 (2017).
Corvey, K., Menear, K. S., Preskitt, J., Goldfarb, S. & Menachemi, N. Obesity, physical activity and sedentary behaviors in children with an autism spectrum disorder. Matern Child Health J. 20, 466–476 (2016).
Castro, K. et al. Feeding behavior and dietary intake of male children and adolescents with autism spectrum disorder: a case-control study. Int J Dev Neurosci. 53, 68–74 (2016).
Bicer, A. H. & Alsaffar, A. A. Dietary intake and physical activity levels of male adolescents with autism spectrum disorder (ASD) and normal to high body mass index (BMI)-a case series study. Res Autism Spect Dis. 31, 1–10 (2016).
Mari-Bauset, S., Llopis-Gonzalez, A., Zazpe-Garcia, I., Mari-Sanchis, A. & Morales-Suarez-Varela, M. Nutritional status of children with autism spectrum disorders (ASDs): a case-control study. J Autism Dev Disord. 45, 203–212 (2015).
Hill, A. P., Zuckerman, K. E. & Fombonne, E. Obesity and autism. Pediatrics. 136, 1051–1061 (2015).
Croen, L. A. et al. The health status of adults on the autism spectrum. Autism. 19, 814–823 (2015).
Phillips, K. L. et al. Prevalence and impact of unhealthy weight in a national sample of US adolescents with autism and other learning and behavioral disabilities. Matern Child Health J. 18, 1964–1975 (2014).
Bandini, L. G. et al. Comparison of physical activity between children with autism spectrum disorders and typically developing children. Autism. 17, 44–54 (2013).
Meguid, N. et al. Dietary patterns of children with autism spectrum disorder: a study based in Egypt. Open Access Maced J Med Sci. 3, 262–267 (2015).
Bicer, A. H. & Alsaffar, A. A. Body mass index, dietary intake and feeding problems of Turkish children with autism spectrum disorder (ASD). Res Dev Disabil. 34, 3978–3987 (2013).
Accordino, R. E., Kidd, C., Politte, L. C., Henry, C. A. & McDougle, C. J. Psychopharmacological interventions in autism spectrum disorder. Expert Opin Pharmacother. 17, 937–952 (2016).
Yoon, Y., Wink, L. K., Pedapati, E. V., Horn, P. S. & Erickson, C. A. Weight gain effects of second-generation antipsychotic treatment in autism spectrum disorder. J Child Adolesc Psychopharmacol. 26, 822–827 (2016).
Wallace, G. L. et al. Real-world executive functions in adults with autism spectrum disorder: profiles of impairment and associations with adaptive functioning and co-morbid anxiety and depression. J Autism Dev Disord. 46, 1071–1083 (2016).
Levin, A. & Scher, A. Sleep problems in young children with autism spectrum disorders: a study of parenting stress, mothers’ sleep-related cognitions, and bedtime behaviors. CNS Neurosci Ther. 22, 921–927 (2016).
Shinawi, M. et al. 11p14.1 microdeletions associated with ADHD, autism, developmental delay, and obesity. Am JMed Genet A. 155A, 1272–1280 (2011).
Fernandez, B. A. et al. Phenotypic spectrum associated with de novo and inherited deletions and duplications at 16p11.2 in individuals ascertained for diagnosis of autism spectrum disorder. J Med Genet. 47, 195–203 (2010).
Acknowledgements
This work was supported by the National Science Foundation of China (No. 81330016, No. 81630038 to Dezhi Mu), a Grant from the State Commission of Science Technology of China (2012BAI04B04), a Grant from the Science and Technology Bureau of Sichuan Province (2014SZ0149), a Grant from the Major State Basic Research Development Program (2013CB967404), a Grant of clinical discipline program (neonatology) from the Ministry of Health of China (1311200003303), and a Grant from Ministry of Education of China (IRT0935).
Author information
Authors and Affiliations
Contributions
Z.Z. and L.Z. conceived and designed the experiments. Z.Z. and S.L. performed the experiments. F.Z., Y.W. and L.H. analyzed the data. J.H., R.Z. and Y.Q. contributed reagents/materials/analysis tools. Z.Z. wrote the manuscript. D.M. revised the manuscript and was the fund contributor.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zheng, Z., Zhang, L., Li, S. et al. Association among obesity, overweight and autism spectrum disorder: a systematic review and meta-analysis. Sci Rep 7, 11697 (2017). https://doi.org/10.1038/s41598-017-12003-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12003-4
This article is cited by
-
Promoting Physical Activity Through Telehealth, Peer Support, and Wearables: A Pilot Randomized Controlled Trial Among Adults with Autism Spectrum Disorder
Journal of Developmental and Physical Disabilities (2024)
-
Neophobia, sensory experience and child’s schemata contribute to food choices
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2024)
-
Differences in Mealtime Behaviors, Food Security, and Weight Concerns Between Neurotypical Youth and Youth with Autism Spectrum Disorder
Advances in Neurodevelopmental Disorders (2023)
-
High-Fat Diet Exacerbates Autistic-Like Restricted Repetitive Behaviors and Social Abnormalities in CC2D1A Conditional Knockout Mice
Molecular Neurobiology (2023)
-
Prevalence and factors associated with overweight, obesity, and hypertension in a large clinical sample of adults with autism spectrum disorder
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.