Abstract
Over 15 million patients with epilepsy worldwide do not respond to drugs. Successful surgical treatment requires complete removal or disconnection of the seizure onset zone (SOZ), brain region(s) where seizures originate. Unfortunately, surgical success rates vary between 30 and 70% because no clinically validated biological marker of the SOZ exists. We develop and retrospectively validate a new electroencephalogram (EEG) marker—neural fragility—in a retrospective analysis of 91 patients by using neural fragility of the annotated SOZ as a metric to predict surgical outcomes. Fragility predicts 43 out of 47 surgical failures, with an overall prediction accuracy of 76% compared with the accuracy of clinicians at 48% (successful outcomes). In failed outcomes, we identify fragile regions that were untreated. When compared to 20 EEG features proposed as SOZ markers, fragility outperformed in predictive power and interpretability, which suggests neural fragility as an EEG biomarker of the SOZ.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
We also released the raw iEEG data for patients from NIH, UMH, UMMC, and JHH in the OpenNeuro repository in the form of BIDS-iEEG (https://openneuro.org/datasets/ds003029). Due to restrictions on data sharing from CClinic, we were unable to release the raw iEEG data that we received from this site. Dataset from CClinic is available upon request from authors at the CClinic. Source data are provided with this paper.
Code availability
All main figures of the paper can be reproduced using https://doi.org/10.34747/eagk-r33477. We include a jupyter notebook written in Python to help reproduce figures. An example of neural fragility being run on patient 01 can be shared upon request due to licensing restrictions.
The neural fragility algorithm has been implemented in a FDA 510k approved software medical device (current 510k number: K201910). More information will be available at www.neurologicsolutions.co. Otherwise, please contact corresponding authors for more information regarding a clinical demonstration.
Change history
21 March 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41593-022-01047-z
References
Berg, A. T. Identification of pharmacoresistant epilepsy. Neurologic Clinics 27, 1003–1013 (2009).
Epilepsy: A Public Health Imperative (World Health Organization, 2019).
Jobst, B. C. Consensus over individualism: validation of the ILAE definition for drug resistant epilepsy. Epilepsy Curr. 15, 172–173 (2015).
Begley, C. E. & Durgin, T. L. The direct cost of epilepsy in the United States: a systematic review of estimates. Epilepsia 56, 1376–1387 (2015).
Jehi, L. The epileptogenic zone: concept and definition. Epilepsy Curr. 18, 12–16 (2018).
Penfield, W. Epileptogenic lesions. Acta Neurol. Psychiatr. Belg. 56, 75–88 (1956).
Jobst, B. C., Darcey, T. M., Thadani, V. M. & Roberts, D. W. Brain stimulation for the treatment of epilepsy: brain stimulation in epilepsy. Epilepsia 51, 88–92 (2010).
Scharfman, H. E. The neurobiology of epilepsy. Curr. Neurol. Neurosci. Rep. 7, 348–354 (2007).
Gliske, S. V. et al. Universal automated high frequency oscillation detector for real-time, long term EEG. Clin. Neurophysiol. 127, 1057–1066 (2016).
Shah, P. et al. Local structural connectivity directs seizure spread in focal epilepsy. Preprint at bioRxiv https://doi.org/10.1101/406793 (2018).
Li, A. et al. Using network analysis to localize the epileptogenic zone from invasive EEG recordings in intractable focal epilepsy. Netw. Neurosci. 2, 218–240 (2018).
Burns, S. P. et al. Network dynamics of the brain and influence of the epileptic seizure onset zone. Proc. Natl Acad. Sci. USA 111, E5321–E5330 (2014).
Yaffe, R. B. et al. Physiology of functional and effective networks in epilepsy. Clin. Neurophysiol. 126, 227–236 (2015).
Khambhati, A. N., Davis, K. A., Lucas, T. H., Litt, B. & Bassett, D. S. Virtual cortical resection reveals push–pull network control preceding seizure evolution. Neuron 91, 1170–1182 (2016).
Bassett, D. S. & Sporns, O. Network neuroscience. Nat. Neurosci. 20, 353–364 (2017).
Li, A., Inati, S., Zaghloul, K. & Sarma, S. Fragility in epileptic networks: the epileptogenic zone. in Proc. American Control Conference (IEEE, 2017); https://ieeexplore.ieee.org/abstract/document/7963378
Li, A. et al. Linear time-varying model characterizes invasive EEG signals generated from complex epileptic networks. in Proc. Annual International Conference of the IEEE Engineering in Medicine and Biology Society 2802–2805 (IEEE, 2017); https://pubmed.ncbi.nlm.nih.gov/29060480/
Sritharan, D. & Sarma, S. V. Fragility in dynamic networks: application to neural networks in the epileptic cortex. Neural Comput. 26, 2294–2327 (2014).
Jette, N., Reid, A. Y. & Wiebe, S. Surgical management of epilepsy. CMAJ 186, 997–1004 (2014).
Engel, J. et al. Early surgical therapy for drug-resistant temporal lobe epilepsy: a randomized trial. JAMA 307, 922–930 (2012).
Sheikh, S., Nair, D., Gross, R. & Gonzalez Martinez, J. Tracking a changing paradigm and the modern face of epilepsy surgery: a comprehensive and critical review on the hunt for the optimal extent of resection in mesial temporal lobe epilepsy. Epilepsia 60, 1768–1793 (2019).
Crino, P. B. et al. Increased expression of the neuronal glutamate transporter (EAAT3/EAAC1) in hippocampal and neocortical epilepsy. Epilepsia 43, 211–218 (2002).
González-Martínez, J. A., Ying, Z., Prayson, R., Bingaman, W. & Najm, I. Glutamate clearance mechanisms in resected cortical dysplasia: Laboratory investigation. J. Neurosurg. 114, 1195–1202 (2011).
Noebels, J. L. The biology of epilepsy genes. Annu. Rev. Neurosci. 26, 599–625 (2003).
Bradford, H. F. Glutamate, GABA and epilepsy. Prog. Neurobiol. 47, 477–511 (1995).
Traub, R. D. et al. A possible role for gap junctions in generation of very fast EEG oscillations preceding the onset of, and perhaps initiating, seizures. Epilepsia 42, 153–170 (2001).
DeFelipe, J. Chandelier cells and epilepsy. Brain 122, 1807–1822 (1999).
Jin, X., Prince, D. A. & Huguenard, J. R. Enhanced excitatory synaptic connectivity in layer V pyramidal neurons of chronically injured epileptogenic neocortex in rats. J. Neurosci. 26, 4891–4900 (2006).
Bulacio, J. C., Chauvel, P. & McGonigal, A. Stereoelectroencephalography: interpretation. J. Clin. Neurophysiol. 33, 503–210 (2016).
Couronné, R., Probst, P. & Boulesteix, A. L. Random forest versus logistic regression: a large-scale benchmark experiment. BMC Bioinformatics 19, 270 (2018).
Sheikh, S. et al. (Re)defining success in epilepsy surgery: the importance of relative seizure reduction in patient-reported quality of life. Epilepsia 60, 2078–2085 (2019).
Vakharia, V. N. et al. Getting the best outcomes from epilepsy surgery. Ann. Neurol. 83, 676–690 (2018).
Varatharajah, Y. et al. Integrating artificial intelligence with real-time intracranial EEG monitoring to automate interictal identification of seizure onset zones in focal epilepsy. J. Neural Eng. 15, 046035 (2018).
Laxer, K. D. et al. The consequences of refractory epilepsy and its treatment. Epilepsy Behav. 37, 59–70 (2014).
McIntosh, A. M. et al. Long-term seizure outcome and risk factors for recurrence after extratemporal epilepsy surgery. Epilepsia 53, 970–978 (2012).
Yardi, R. et al. Long-term outcomes of reoperations in epilepsy surgery. Epilepsia 61, 465–478 (2020).
Jeppesen, J., Beniczky, S., Johansen, P., Sidenius, P. & Fuglsang-Frederiksen, A. Detection of epileptic seizures with a modified heart rate variability algorithm based on Lorenz plot. Seizure 24, 1–7 (2015).
Chung, J. et al. Statistical connectomics. Preprint at OSF https://doi.org/10.31219/osf.io/ek4n3 (2020).
Fedele, T. et al. Resection of high frequency oscillations predicts seizure outcome in the individual patient. Sci. Rep. 7, 13836 (2017).
Haegelen, C. et al. High-frequency oscillations, extent of surgical resection, and surgical outcome in drug-resistant focal epilepsy. Epilepsia 54, 848–857 (2013).
Cuello-Oderiz, C. et al. Value of ictal and interictal epileptiform discharges and high frequency oscillations for delineating the epileptogenic zone in patients with focal cortical dysplasia. Clin. Neurophysiol. 129, 1311–1319 (2018).
Höller, Y. et al. High-frequency oscillations in epilepsy and surgical outcome. A meta-analysis. Front. Hum. Neurosci. 9, 574 (2015).
Spring, A. M. et al. Interrater reliability of visually evaluated high frequency oscillations. Clin. Neurophysiol. 128, 433–441 (2017).
Höller, P., Trinka, E. & Höller, Y. Electroencephalogram: mission impossible without computational intelligence. Comput. Intell. Neurosci. 2018, 1638097 (2018).
Gloss, D., Nevitt, S. J. & Staba, R. The role of high-frequency oscillations in epilepsy surgery planning. Cochrane Database Syst. Rev. 10, CD010235 (2017).
Chang, W. C. et al. Loss of neuronal network resilience precedes seizures and determines the ictogenic nature of interictal synaptic perturbations. Nat. Neurosci. 21, 1742–1752 (2018).
Kramer, M. A. & Cash, S. S. Epilepsy as a disorder of cortical network organization. Neuroscientist 18, 360–372 (2012).
Meador, K. J., Kapur, R., Loring, D. W., Kanner, A. M. & Morrell, M. J. Quality of life and mood in patients with medically intractable epilepsy treated with targeted responsive neurostimulation. Epilepsy Behav. 45, 242–247 (2015).
Loring, D. W., Kapur, R., Meador, K. J. & Morrell, M. J. Differential neuropsychological outcomes following targeted responsive neurostimulation for partial-onset epilepsy. Epilepsia 56, 1836–1844 (2015).
D’Andrea Meira, I. et al. Ketogenic diet and epilepsy: what we know so far. Front. Neurosci. 13, 5 (2019).
Hawasli, A. H., Bandt, S. K., Hogan, R. E., Werner, N. & Leuthardt, E. C. Laser ablation as treatment strategy for medically refractory dominant insular epilepsy: therapeutic and functional considerations. Stereotact. Funct. Neurosurg. 92, 397–404 (2014).
Gonzalez-Martinez, J. & Lachhwani, D. Stereoelectroencephalography in children with cortical dysplasia: technique and results. Childs Nerv. Syst. 30, 1853–1857 (2014).
See, S. J. et al. Surgical outcomes in patients with extratemporal epilepsy and subtle or normal magnetic resonance imaging findings. Neurosurgery 73, 68–76 (2013).
Kemp, B., Värri, A., Rosa, A. C., Nielsen, K. D. & Gade, J. A simple format for exchange of digitized polygraphic recordings. Electroencephalogr. Clin. Neurophysiol. 82, 391–393 (1992).
Holdgraf, C. et al. iEEG-BIDS, extending the Brain Imaging Data Structure specification to human intracranial electrophysiology. Sci. Data 6, 102 (2019).
Gorgolewski, K. J. et al. The brain imaging data structure, a format for organizing and describing outputs of neuroimaging experiments. Sci. Data 3, 160044 (2016).
Gramfort, A. et al. MEG and EEG data analysis with MNE-Python. Front. Neurosci. 7, 267 (2013).
Gramfort, A. et al. MNE software for processing MEG and EEG data. NeuroImage 86, 446–460 (2014).
Appelhoff, S. et al. MNE-BIDS: MNE-Python + BIDS = easy dataset interaction. Zenodo https://doi.org/10.5281/zenodo.3891836 (2020).
Van Der Walt, S., Colbert, S. C. & Varoquaux, G. The NumPy array: a structure for efficient numerical computation. Comput. Sci. Eng. 13, 22–30 (2011).
Virtanen, P. et al. SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat. Methods 17, 261–272 (2020).
Hunter, J. D. Matplotlib: a 2D graphics environment. Comput. Sci. Eng. 9, 99–104 (2007).
Waskom, M. seaborn: statistical data visualization. J. Open Source Softw. https://doi.org/10.21105/joss.03021 (2021).
Allen, M., Poggiali, D., Whitaker, K., Marshall, T. R. & Kievit, R. A. Raincloud plots: a multi-platform tool for robust data visualization [version 1; peer review: 2 approved]. Wellcome Open Res. 4, 63 (2019).
Ho, J., Tumkaya, T., Aryal, S., Choi, H. & Claridge-Chang, A. Moving beyond P values: data analysis with estimation graphics. Nat. Methods 16, 565–566 (2019).
Vallat, R. Pingouin: statistics in Python. J. Open Source Softw. 3, 1026 (2018).
Raschka, S. MLxtend: providing machine learning and data science utilities and extensions to Python’s scientific computing stack. J. Open Source Softw. 3, 638 (2018).
Pedregosa, F. et al. Scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011).
Mezić, I. Spectral properties of dynamical systems, model reduction and decompositions. Nonlinear Dyn. 41, 309–325 (2005).
Schmid, P. Dynamic mode decomposition of numerical and experimental data. J. Fluid Mech. 656, 5–28 (2010).
Breiman, L. Random forests. Mach. Learn. 45, 5–32 (2001).
Perry, R. et al. Manifold forests: closing the gap on neural networks. Preprint at https://arxiv.org/abs/1909.11799 (2019).
& Tomita, T. M. et al. Sparse projection oblique randomer forests. J. Mach. Learn. Res. 21, 1–39 (2020).
Skocik, M., Collins, J., Callahan-Flintoft, C., Bowman, H. & Wyble, B. I tried a bunch of things: the dangers of unexpected overfitting in classification. Preprint at bioRxiv https://doi.org/10.1101/078816 (2016).
Alyakin, A., Qin, Y. & Priebe, C. E. LqRT: Robust hypothesis testing of location parameters using Lq-Likelihood-Ratio-Type test in Python. Preprint at https://arxiv.org/abs/1911.11922 (2019).
Qin, Y. & Priebe, C. E. Robust hypothesis testing via Lq-likelihood. Statistica Sinica 27, 1793–1813 (2017).
Li, A. et al. Neural fragility as an EEG marker of the seizure onset zone. Figshare https://doi.org/10.34747/eagk-r334 (2021).
Acknowledgements
A.L. is supported by NIH T32 EB003383, the NSF GRFP (DGE-1746891), the Arcs Chapter Scholarship, the Whitaker Fellowship and the Chateaubriand Fellowship. S.V.S. is supported by NIH R21 NS103113, the Coulter Foundation, the Maryland Innovation Initiative, a US NSF Career Award 1055560 and the Burroughs Wellcome Fund CASI Award 1007274. E.J. is supported by NIA K23 AG063899. I.C. was partially supported by NIH R25NS108937-02. K.A.Z. and S.I. are supported by the Intramural Research Program of the National Institute of Neurological Disorders and Stroke. S.C. is supported by 1UL1TR003098-01 and the UMB Institute for Clinical and Translational Research. J. Hopp is supported by NINDS 1 UO1 NS08803401—Established Status Epilepticus Treatment Trial (ESETT), MII TA Grant 20180828 TEDCO—EpiWatch: A Mobile Health Application for Epilepsy Management and U10 NS058932-01 NIH NINDS—‘Neurological Emergencies Treatment Trials (NETT) Network Clinical/Site Hub’. Computational resources were also provided by the Maryland Advanced Research Computing Center (MARCC). The authors would like to thank C. Priebe for useful discussions on statistical analyses, J. Vogelstein for introducing A.L. to the concepts of structured RFs, S. Kim and R. J. Smith for very helpful reviews of the manuscript and M. Breault for help in creating brain figures.
Author information
Authors and Affiliations
Contributions
A.L., J.G.-M. and S.V.S. conceived the project. A.L., I.C., D.B., J.J., A.O.C., A.M.K., J. Hopp, S.C., J. Haagensen, E.J., W.A., N.C., Z.F., J.B. and J.G.-M. collected and supervised human epilepsy recordings and processes related to IRB at their respective centers. I.C., D.B., J.J., A.O.C. and A.M.K. oversaw data from UMHC. J. Hopp, S.C. and J. Haagensen oversaw data from UMMC. E.J., W.A. and N.C. oversaw data from JHH. S.I. and K.A.Z. oversaw data from the NIH. Z.F., J.B. and J.G.-M. oversaw data from CClinic. A.L. organized the data from all centers, converted data to BIDS, conducted the analyses and generated the figures. A.L. and S.V.S. wrote the paper with input from the other authors. C.H. helped develop the structured RF and statistical analyses.
Corresponding author
Ethics declarations
Competing interests
The authors declare the following competing interests: A.L., S.V.S. and J.G.-M. have equity in a startup, Neurologic Solutions Co., related to epilepsy data analysis. W.A. is on the Board of Advisors of Longeviti Neuro Solutions and a Compensated Consultant at Globus Medical. J. Hopp reports the following disclosures: personal compensation: royalties from publishing (UpToDate, Inc.); honoraria from speaking engagements: J. Kiffin Penry Epilepsy Education Programs; expert witness consultation: Gerolamo McNulty Divis & Lewbart A Professional Corporation Attorneys At Law Goodell, Devries, Leech & Dann, LLP. All other authors declare no competing interests.
Additional information
Peer review information Nature Neuroscience thanks the anonymous reviewers for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Computational experiment setup for all candidate SOZ features and statistical analysis.
Computational experiment setup for all candidate SOZ features and statistical analysis - (a) Any candidate feature that can produce a spatiotemporal heatmap was computed from EEG data and then partitioned by the clinically annotated SOZ set and the complement, SOZC (that is non-SOZ electrodes) to compute a confidence statistic measuring the feature’s belief of the clinician’s hypothesis. Here FSOZ and FSOZC were the feature values within their respective sets. fθ is the function depending on the Random Forest model parameters, θ that maps the statistics of the FSOZ and FSOZC to a confidence statistic. An ideal feature would have high and low confidence for success and failed outcomes respectively. Each point on the final CS distribution comparisons represent one patient. (b) A more detailed schematic of how our proposed fragility and baseline features were computed from EEG data for a single snapshot of EEG data. See fragility methods section for description of x, A and Δ.
Extended Data Fig. 2 Entire fragility heatmap of seizures in successful and failed surgical outcomes.
Entire fragility heatmap of seizures in successful and failed surgical outcomes - Fragility heatmaps with electrodes on y-axis and time on x-axis with the dashed white-lines denoting seizure onset and offset. Shows a period of 30 seconds before seizure onset and 30 seconds after seizure offset. (a) Shows clinically annotated maps of the implanted ECoG/SEEG electrodes with red denoting SOZ contacts. (b) shows spatiotemporal fragility heatmaps for example of successful outcome (Patient_01), and failed outcome (Patient_26 and Patient_40). The color scale represents the amplitude of the normalized fragility metric, with closer to 1 denoting fragile regions and closer to 0 denoting relatively stable regions. The contacts in red and orange are part of the SOZ and RZ, respectively as defined in 4 section. Note that the red contacts are also part of the RZ. Within the seizures, estimating the linear systems are not as stable, which can be seen by fragility ‘everywhere’ in the map. Visualized with Turbo continuous colormap. Best seen if viewed in color.
Extended Data Fig. 3 Pooled fragility distribution analysis for all patients.
Pooled fragility distribution analysis for all patients - failed (a), no surgery (b) and successful surgery (c) datasets. Each SOZ (soz in blue bars) and SOZC (‘nsoz’ in orange bars) distribution per patient was bootstrap sampled (see 4 for more information on sampling) and then compared using the one-sided Mann-Whitney U test. The corresponding test yielded a statistic of 2776334 (PValue = 0.355) for the failed patient outcomes and a statistic of 36836739 (PValue = 3.326e-70) for the successful patient outcomes. The patients without resection were not included in the analysis comparing to outcome, but these patients can present as interesting case studies where the SOZ was hypothetically localizable, but perhaps was too close to eloquent areas.
Extended Data Fig. 4 Patient-specific SOZ vs SOZC neural fragility near seizure onset.
Patient-specific SOZ vs SOZC neural fragility near seizure onset - Red SOZ vs black SOZC signals for patients presented in Figure 4: Patient_01(a), Patient_26(b), Patient_40(c). For each patient, the ictal snapshots available are visualized around seizure onset with 5 seconds before onset until the first 20% of the seizure. Not necessarily all electrodes in the clinically annotated SOZ are part of the EZ when the patient had a successful outcome. Therefore, if neural fragility had value in contrasting true EZ electrodes from non-EZ electrodes, then any extra electrodes clinically annotated in the SOZ should have relative lower fragility. The lines represent mean +/- sem.
Extended Data Fig. 5 Pooled-patient per clinical center SOZ vs SOZC neural fragility.
Pooled-patient per clinical center SOZ vs SOZC neural fragility - Red SOZ vs black SOZC fragility signals for pooled patients within each of the five centers with successful (a) and failed outcomes (b) for NIH (n=14), JHH (n=4), CC (n=61), UMH (n=5), and UMMC (n=7) (top to bottom respectively). Note UMMC only had successful outcomes, so there was28 no curve for the failures. Seizure periods were resampled and normalized to 100 samples for averaging and viewing purposes. In JHH and UMH, there were only one and two patients in successful outcomes respectively. The lines represent mean +/- sem.
Extended Data Fig. 6 Comparison of classification models using different features.
Comparison of classification models using different features - (a) The ROC curve over 10 folds of cross-validation of the held-out test set obtained by applying a Random Forest model onto the spatiotemporal heatmaps to predict surgical outcome (see 4). Fragility and the top-3 baseline features in terms of AUC are visualized. The shaded area represents the standard deviation of the curve obtained by linear interpolation for visualization purposes. The AUC of fragility obtained a 0.88 +/- 0.064 over the 10 standard deviation with a relative improvement of 7.2% improvement in AUC compared to the next best feature representation (that is the beta frequency band). At the Youden point (stars), neural fragility obtains a balanced accuracy score of 0.76 +/- 0.06, and an improvement of 0.32 in TPR and 0.32 in FPR compared to the clinical operating point (red star). (b) The average PR curve showing that fragility is better then the top 3 features by at least an average precision of 0.04. (c) A paired estimation plot showing how the same test set of patients differed in AUC depending on whether it was using the fragility, or beta feature heatmap representation. The paired Cohen’s D effect size was computed at -0.975 (-1.97 to -0.29; 95% CI). The p-values associated with the difference between Neural Fragility and the Beta frequency band were 0.0204, 0.0273, and 0.0225 using the one-sided Wilcoxon rank-sum test, permutation test, and the paired student t-test respectively. (d) Calibration curve showing the fraction of actual successful surgical outcomes on the y-axis vs the average CS output on the x-axis. The curve measures how calibrated the predicted success probability values are to the true risk stratification of the patient population. The closer a curve is to the y = x line, then the more calibrated a model is. It is quantified by the Brier-loss (closer to 0 is better), which is shown in the legend, and is significantly lower then the next best feature (an improvement of 15%). The shaded region represents 95% confidence interval of two standard deviations.
Extended Data Fig. 7 Estimated feature importance (mean and stdev) of the associated fragility heatmap used estimated using permutation.
Estimated feature importance (mean and stdev) of the associated fragility heatmap used estimated using permutation - The metric of interest was the concordance statistic (that is AUC) of the ROC curve. The original feature map is transformed into a 20dimensional set of time-varying statistics of its SOZ and SOZC electrodes describing the quantiles of the spatiotemporal heatmap (10% - 100% quantiles). This time-varying summary allows these heatmaps to be pooled together across subjects when training a Random Forest classifier as described in Methods.
Extended Data Fig. 8 Neural fragility vs frequency power values.
Neural fragility vs frequency power values - Fragility versus frequency power in the delta, theta, alpha, beta, gamma and highgamma band for Patient_01, Patient_26, and Patient_40. For band definitions, refer to Methods - Baseline features - spectral features. Every point represents the spectral power and neural fragility value from a randomly chosen window and electrode from one of the patients. No significant correlation is seen or computed from the data. Each spectral feature and fragility are normalized as described in Methods.
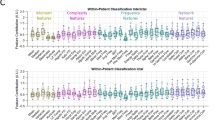
Extended Data Fig. 9 Interpretability ratio of feature heatmaps.
Interpretability ratio of feature heatmaps - a) Two heatmap examples of a seizure snapshot of Patient_01 (NIH treated, ECoG, CC1, Engel I, ILAE 1) with the beta frequency band (left) and the neural fragility heatmap (right). Both colormaps show the relative feature value normalized across channels over time. The black line denotes electrographic seizure onset. (b) A box plot of the interpretability ratio that is defined in Results Section 8.12 computed for every feature. The y-axis shows an effect size difference between the interpretability ratios of success and failed outcomes. The interpretability ratio for each patient’s heatmap is defined as the ratio between the feature values in the two electrode sets (SOZ/ SOZC). Neural fragility is significantly greater then the beta band (alpha Level=0.05).
Extended Data Fig. 10 Neural fragility correlation against non-epileptic clinical covariates.
Neural fragility correlation against non-epileptic clinical covariates - Fragility success probabilities (denoted as ‘Confidence Statistic’ in y-axes) split by clinical factors, such as handedness (a), gender (b), ethnicity (c) and age at surgery (d). Not all patients had data for each of these categories, so the subset of available data was used. Note the sample sizes vary across different groups shown. For ethnicity, we also had 1 Asian subject, but left it out because the permutation effect size estimation procedure does not work for 1 sample. Effect sizes were estimated using the permutation test and Mann Whitney U test described in Methods. The corresponding effect sizes and p-values were (0.1/0.99) for handedness, and (0.12/0.7) for gender. The pvalue was computed using the one-sided Mann-Whitney U test. The slope was negligibly close to 0 for surgery age linear fit. There was no relatively notable trend in the data related to ethnicity. The significant Cohen’s D effect size difference is primarily due to the low sample sizes in non-Caucasian ethnicities. The error bars represent 95% confidence interval specified by 2 standard deviations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–4.
Supplementary Table 1
Clinical metadata for each patient in the study.
Source data
Source Data Fig. 5
Box plot summary.
Source Data Fig. 6
Box plot summary.
Rights and permissions
About this article
Cite this article
Li, A., Huynh, C., Fitzgerald, Z. et al. Neural fragility as an EEG marker of the seizure onset zone. Nat Neurosci 24, 1465–1474 (2021). https://doi.org/10.1038/s41593-021-00901-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41593-021-00901-w
This article is cited by
-
Generalisability of epileptiform patterns across time and patients
Scientific Reports (2024)
-
High-performance prediction of epilepsy surgical outcomes based on the genetic neural networks and hybrid iEEG marker
Scientific Reports (2024)
-
Graph theoretical measures of fast ripple networks improve the accuracy of post-operative seizure outcome prediction
Scientific Reports (2023)
-
Epilepsy Detection with Multi-channel EEG Signals Utilizing AlexNet
Circuits, Systems, and Signal Processing (2023)
-
Graph-generative neural network for EEG-based epileptic seizure detection via discovery of dynamic brain functional connectivity
Scientific Reports (2022)