Abstract
Considerable changes have occurred in the management of differentiated thyroid cancer (DTC) during the past four decades, based on improved knowledge of the biology of DTC and on advances in therapy, including surgery, the use of radioactive iodine (radioiodine), thyroid hormone treatment and availability of recombinant human TSH. Improved diagnostic tools are available, including determining serum levels of thyroglobulin, neck ultrasonography, imaging (CT, MRI, SPECT–CT and PET–CT), and prognostic classifications have been improved. Patients with low-risk DTC, in whom the risk of thyroid cancer death is <1% and most recurrences can be cured, currently represent the majority of patients. By contrast, patients with high-risk DTC represent 5–10% of all patients. Most thyroid cancer-related deaths occur in this group of patients and recurrences are frequent. Patients with high-risk DTC require more aggressive treatment and follow-up than patients with low-risk DTC. Finally, the strategy for treating patients with intermediate-risk DTC is frequently defined on a case-by-case basis. Prospective trials are needed in well-selected patients with DTC to demonstrate the extent to which treatment and follow-up can be limited without increasing the risk of recurrence and thyroid cancer-related death.
Key points
-
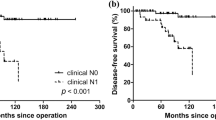
Prognostic classifications currently distinguish the risk of differentiated thyroid cancer (DTC)-related death from the risk of recurrence.
-
The majority of patients with DTC have low-risk disease; postoperative administration of radioiodine is indicated in selected patients and thyroid hormone treatment maintains serum levels of TSH within the normal range.
-
Follow-up is based on determination of serum levels of thyroglobulin and neck ultrasonography.
-
Fluorodeoxyglucose PET–CT is useful for the detection of neoplastic foci in patients with high-risk DTC and in those with detectable serum levels of thyroglobulin that increases over time during follow-up.
-
Patients with distant metastases are first treated with radioiodine, and with focal treatment modalities as necessary; patients with progression might benefit from systemic targeted therapies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Mazzaferri, E. L., Young, R. L., Oertel, J. E., Kemmerer, W. T. & Page, C. P. Papillary thyroid carcinoma: the impact of therapy in 576 patients. Medicine 56, 171–196 (1977).
Mazzaferri, E. L. & Jhiang, S. M. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am. J. Med. 97, 418–428 (1994).
Hay, I. D. et al. Papillary thyroid carcinoma (PTC) in children and adults: comparison of initial presentation and long-term postoperative outcome in 4432 patients consecutively treated at the Mayo clinic during eight decades (1936–2015). World J. Surg. 42, 329–342 (2018).
Schlumberger, M. et al. Follow-up of low-risk patients with differentiated thyroid carcinoma: a European perspective. Eur. J. Endocrinol. 50, 105–112 (2004).
Cady, B. Papillary carcinoma of the thyroid gland: treatment based on risk group definition. Surg. Oncol. Clin. N. Am. 7, 633–644 (1998).
Tubiana, M. et al. Long-term results and prognostic factors in patients with differentiated thyroid carcinoma. Cancer 55, 794–804 (1985).
Davies, L. & Welch, H. G. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA 295, 2164–2167 (2006).
Vaccarella, S. et al. Worldwide thyroid cancer epidemic? The increasing impact of overdiagnosis. N. Engl. J. Med. 375, 614–617 (2016).
Haugen, B. R. et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: American Thyroid Association Management Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26, 1–133 (2016).
Filetti, S. et al. Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 30, 1856–1883 (2019).
Lloyd, R. V., Osamura, R. Y., Kloppel, G. & Rosai, J. (eds) WHO Classification of Tumours of Endocrine Organs. 4th ed. (IARC, 2017).
Nikiforov, Y. E. et al. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: a paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol. 2, 1023–1029 (2016).
Fagin, J. A. & Wells, S. A. Jr. Biologic and clinical perspectives on thyroid cancer. N. Engl. J. Med. 375, 1054–1067 (2016).
Cancer Genome Atlas Research Network. Integrated genomic characterization of papillary thyroid carcinoma. Cell 159, 676–690 (2014).
Yoo, S. K. et al. Comprehensive analysis of the transcriptional and mutational landscape of follicular and papillary thyroid cancers. PLoS Genet. 12, e1006239 (2016).
Ganly, I. et al. Integrated genomic analysis of Hürthle cell cancer reveals oncogenic drivers, recurrent mitochondrial mutations, and unique chromosomal landscapes. Cancer Cell 34, 256–270 (2018).
Landa, I. et al. Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J. Clin. Invest. 126, 1052–1066 (2016).
Xing, M. Genetic-guided risk assessment and management of thyroid cancer. Endocrinol. Metab. Clin. N. Am. 48, 109–124 (2019).
Tuttle, R. M. & Alzahrani, A. S. Risk stratification in differentiated thyroid cancer: from detection to final follow-up. J. Clin. Endocrinol. Metab. 104, 4087–4100 (2019).
Durante, C. et al. Long term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J. Clin. Endocrinol. Metab. 91, 2892–2899 (2006).
Liu, J. et al. The genetic duet of BRAF V600E and TERT promoter mutations robustly predicts loss of radioiodine avidity in recurrent papillary thyroid cancer. J. Nucl. Med. 61, 177–182 (2020).
Durante, C. et al. BRAF mutations in papillary thyroid carcinomas inhibit genes involved in iodine metabolism. J. Clin. Endocrinol. Metab. 92, 2840–2843 (2007).
Azouzi, N. et al. NADPH oxidase NOX4 is a critical mediator of BRAFV600E-induced down regulation of the sodium iodide symporter in papillary thyroid carcinomas. Antioxid. Redox. Signal. 26, 864–877 (2017).
Chakravarty, D. et al. Small-molecule MAPK inhibitors restore radioiodine incorporation in mouse thyroid cancers with conditional BRAF activation. J. Clin. Invest. 121, 4700–4711 (2011).
Brierley, J. D., Gospodarowicz, M. K. & Wittekind, C. TNM Classification of Malignant Tumours 8th ed. (Wiley, 2017).
Tuttle, R. M., Haugen, B. & Perrier, N. D. Updated American Joint Committee on Cancer/Tumor-Node-Metastasis Staging System for Differentiated and Anaplastic Thyroid Cancer (eighth edition): what changed and why? Thyroid 27, 751–756 (2017).
Tuttle, R. M. et al. Estimating risk of recurrence in differentiated thyroid cancer after total thyroidectomy and radioactive iodine remnant ablation: using response to therapy variables to modify the initial risk estimates predicted by the new American Thyroid Association staging system. Thyroid 20, 1341–1349 (2010).
Grani, G. et al. Real-world performance of the American Thyroid Association risk estimates in predicting 1-year differentiated thyroid cancer outcomes: a prospective multicenter study of 2000 patients. Thyroid https://doi.org/10.1089/thy.2020.0272 (2020).
Trimboli, P. et al. Patient age is an independent risk factor of relapse of differentiated thyroid carcinoma and improves the performance of the American Thyroid Association Stratification System. Thyroid 30, 713–719 (2020).
Momesso, D. P. et al. Dynamic risk stratification in patients with differentiated thyroid cancer treated without radioactive iodine. J. Clin. Endocrinol. Metab. 101, 2692–2700 (2016).
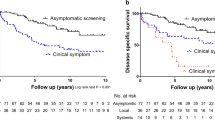
Miyauchi, A. & Ito, Y. Conservative surveillance management of low-risk papillary thyroid microcarcinoma. Endocrinol. Metab. Clin. N. Am. 48, 215–226 (2019).
Leboulleux, S., Tuttle, R. M., Pacini, F. & Schlumberger, M. Papillary thyroid microcarcinoma: time to shift from surgery to active surveillance? Lancet Diabetes Endocrinol. 4, 933–942 (2016).
Zhang, M., Luo, Y., Zhang, Y. & Tang, J. Efficacy and safety of ultrasound-guided radiofrequency ablation for treating low-risk papillary thyroid microcarcinoma: a prospective study. Thyroid 26, 1581–1587 (2016).
Lamartina, L. et al. Follow-up of differentiated thyroid cancer – what should (and what should not) be done. Nat. Rev. Endocrinol. 14, 538–551 (2018).
Wang, T. S. & Sosa, J. A. Thyroid surgery for differentiated thyroid cancer – recent advances and future directions. Nat. Rev. Endocrinol. 14, 670–683 (2018).
Russell, M. D., Kamani, D. & Randolph, G. W. Modern surgery for advanced thyroid cancer: a tailored approach. Gland Surg. 9, S105–S119 (2020).
Fundakowski, C. E. et al. Surgical management of the recurrent laryngeal nerve in thyroidectomy: American Head and Neck Society consensus statement. Head Neck 40, 663–675 (2018).
Hartl, D. M. et al. Current concepts in the management of unilateral recurrent laryngeal nerve paralysis after thyroid surgery. J. Clin. Endocrinol. Metab. 9, 3084–3088 (2005).
Hauch, A., Al-Qurayshi, Z., Randolph, G. & Kandil, E. Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann. Surg. Oncol. 21, 3844–3852 (2014).
Adam, M. A. et al. Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Ann. Surg. 260, 601–605 (2014).
Garsi, J. P. et al. Therapeutic administration of 131I for differentiated thyroid cancer, radiation dose to ovaries and outcome of pregnancies. J. Nucl. Med. 49, 845–852 (2008).
Bourcigaux, N. et al. Impact on testicular function of a single ablative activity of 3.7 GBq radioactive iodine for differentiated thyroid carcinoma. Hum. Reprod. 33, 1408–1416 (2018).
Pacini, F. et al. Testicular function in patients with differentiated thyroid carcinoma treated with radioiodine. J. Nucl. Med. 35, 1418–1422 (1994).
Rubino, C. et al. Second primary malignancies in thyroid cancer patients. Br. J. Cancer 89, 1638–1644 (2003).
Verburg, F. A. et al. Errare humanum est, sed in errare perseverare diabolicum: methodological errors in the assessment of the relationship between I-131 therapy and possible increases in the incidence of malignancies. Eur. J. Nucl. Med. Mol. Imaging 47, 519–522 (2020).
Boucai, L. et al. Radioactive iodine-related clonal hematopoiesis in thyroid cancer is common and associated with decreased survival. J. Clin. Endocrinol. Metab. 103, 4216–4223 (2018).
Singer, M. C. et al. Salivary and lacrimal dysfunction after radioactive iodine for differentiated thyroid cancer: American Head and Neck Society Endocrine Surgery Section and Salivary Gland Section joint multidisciplinary clinical consensus statement of otolaryngology, ophthalmology, nuclear medicine and endocrinology. Head Neck 42, 3446–3459 (2020).
Lamartina, L., Durante, C., Filetti, S. & Cooper, D. S. Low-risk differentiated thyroid cancer and radioiodine remnant ablation: a systematic review of the literature. J. Clin. Endocrinol. Metab. 100, 1748–1761 (2015).
Sawka, A. M. et al. An updated systematic review and commentary examining the effectiveness of radioactive iodine remnant ablation in well-differentiated thyroid cancer. Endocrinol. Metab. Clin. N. Am. 37, 457–480 (2008).
Sacks, W., Fung, C. H., Chang, J. T., Waxman, A. & Braunstein, G. D. The effectiveness of radioactive iodine for treatment of low-risk thyroid cancer: a systematic analysis of the peer-reviewed literature from 1966 to April 2008. Thyroid 20, 1235–1245 (2010).
Jonklaas, J. et al. Outcomes of patients with differentiated thyroid carcinoma following initial therapy. Thyroid 16, 1229–1242 (2006).
Schvartz, C. et al. Impact on overall survival of radioactive iodine in low-risk differentiated thyroid cancer patients. J. Clin. Endocrinol. Metab. 97, 1526–1535 (2012).
Nixon, I. J. et al. The results of selective use of radioactive iodine on survival and on recurrence in the management of papillary thyroid cancer, based on Memorial Sloan-Kettering Cancer Center risk group stratification. Thyroid 23, 683–694 (2013).
Verburg, F. A. et al. Differentiated thyroid cancer patients potentially benefitting from postoperative I-131 therapy: a review of the literature of the past decade. Eur. J. Nucl. Med. Mol. Imaging 47, 78–83 (2020).
Tuttle, R. M. et al. Controversies, consensus, and collaboration in the use of 131I therapy in differentiated thyroid cancer: a joint statement from the American Thyroid Association, the European Association of Nuclear Medicine, the Society of Nuclear Medicine and Molecular Imaging, and the European Thyroid Association. Thyroid 29, 461–470 (2019).
Durante, C. et al. Long-term surveillance of papillary thyroid cancer patients who do not undergo postoperative radioiodine remnant ablation: is there a role for serum thyroglobulin measurement? J. Clin. Endocrinol. Metab. 97, 2748–2753 (2012).
Cailleux, A. F., Baudin, E., Travagli, J. P., Ricard, M. & Schlumberger, M. Is diagnostic iodine-131 scanning useful after total thyroid ablation for differentiated thyroid cancer? J. Clin. Endocrinol. Metab. 85, 175–178 (2000).
Pacini, F. et al. Diagnostic 131-iodine whole-body scan may be avoided in thyroid cancer patients who have undetectable stimulated serum Tg levels after initial treatment. J. Clin. Endocrinol. Metab. 87, 1499–1501 (2002).
Pacini, F. et al. Post-surgical use of radioiodine (131I) in patients with papillary and follicular thyroid cancer and the issue of remnant ablation. A consensus report. Eur. J. Endocrinol. 153, 651–659 (2005).
Schlumberger, M. et al. Strategies of radioiodine ablation in low-risk thyroid cancer patients. N. Engl. J. Med. 366, 1663–1673 (2012).
Mallick, U. et al. Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N. Engl. J. Med. 366, 1674–1685 (2012).
Borget, I. et al. Quality of life and cost-effectiveness assessment of radioiodine ablation strategies in patients with thyroid cancer: results from the randomized phase III ESTIMABL trial. J. Clin. Oncol. 33, 2885–2892 (2015).
Schlumberger, M. et al. ESTIMABL1: favorable outcome after ablation in low risk thyroid cancer patients. Lancet Diabetes Endocrinol. 6, 618–626 (2018); author’s reply 686–687 (2018).
Dehbi, H. M. et al. Recurrence after low-dose radioiodine ablation and recombinant human thyroid-stimulating hormone for differentiated thyroid cancer (HiLo): long-term results of an open-label, non-inferiority randomised controlled trial. Lancet Diabetes Endocrinol. 7, 44–51 (2019).
Matrone, A. et al. Postoperative thyroglobulin and neck ultrasound in the risk restratification and decision to perform 131I ablation. J. Clin. Endocrinol. Metab. 102, 893–902 (2017).
Ahtiainen, V., Vaalavirta, L., Tenhunen, M., Joensuu, H. & Mäenpää, H. Randomised comparison of 1.1 GBq and 3.7 GBq radioiodine to ablate the thyroid in the treatment of low-risk thyroid cancer: a 13-year follow-up. Acta Oncol. 30, 1–8 (2020).
Tuttle, R. M. Distinguishing remnant ablation from adjuvant treatment in differentiated thyroid cancer. Lancet Diabetes Endocrinol. 7, 7–8 (2019).
Sugitani, I. & Fujimoto, Y. Does postoperative thyrotropin suppression therapy truly decrease recurrence in papillary thyroid carcinoma? A randomized controlled trial. J. Clin. Endocrinol. Metab. 95, 4576–4583 (2010).
Grani, G., Ramundo, V., Verrienti, A., Sponziello, M. & Durante, C. Thyroid hormone therapy in differentiated thyroid cancer. Endocrine 66, 43–50 (2019).
Durante, C. et al. Papillary thyroid cancer: time course of recurrences during postsurgery surveillance. J. Clin. Endocrinol. Metab. 98, 636–642 (2013).
Grani, G. et al. Thyroid cancer patients with no evidence of disease: the need for repeat neck ultrasound. J. Clin. Endocrinol. Metab. 104, 4981–4989 (2019).
Baudin, E. et al. Positive predictive value of serum thyroglobulin levels, measured during the first year of follow-up following thyroid hormone withdrawal, in thyroid cancer patients. J. Clin. Endocrinol. Metab. 88, 1107–1111 (2003).
Pacini, F. et al. Outcome of differentiated thyroid cancer with detectable serum Tg and negative diagnostic (131)I whole body scan: comparison of patients treated with high (131)I activities versus untreated patients. J. Clin. Endocrinol. Metab. 86, 4092–4097 (2001).
Vaisman, F. et al. Spontaneous remission in thyroid cancer patients after biochemical incomplete response to initial therapy. Clin. Endocrinol. 77, 132–138 (2012).
Ritter, A. et al. Detecting recurrence following lobectomy for thyroid cancer: role of thyroglobulin and thyroglobulin antibodies. J. Clin. Endocrinol. Metab. 105, 2145–2151 (2020).
Hartl, D. M. et al. Influence of prophylactic neck dissection on rate of retreatment for papillary thyroid carcinoma. World J. Surg. 37, 1951–1958 (2013).
Hartl, D. M. et al. Optimization of staging of the neck with prophylactic central and lateral neck dissection for papillary thyroid carcinoma. Ann. Surg. 255, 777–783 (2012).
Rosario, P. W., de Souza Furtado, M., Mourão, G. F. & Calsolari, M. R. Patients with papillary thyroid carcinoma at intermediate risk of recurrence according to American Thyroid Association criteria can be reclassified as low risk when the postoperative thyroglobulin is low. Thyroid 25, 1243–1248 (2015).
Nascimento, C. et al. Post-operative fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT): an important imaging modality in patients with aggressive histology of differentiated thyroid cancer. Thyroid 25, 437–444 (2015).
Beckham, T. H. et al. Intensity-modulated radiation therapy with or without concurrent chemotherapy in nonanaplastic thyroid cancer with unresectable or gross residual disease. Thyroid 28, 1180–1189 (2018).
Tuttle, R. M. & Sabra, M. M. ATA high-risk thyroid cancer patients demonstrating an excellent response to therapy within a few weeks of initial therapy have better than expected clinical outcomes. Endocr. Pract. 25, 287–289 (2019).
Schlumberger, M., Mancusi, F., Baudin, E. & Pacini, F. 131I therapy for elevated thyroglobulin levels. Thyroid 7, 273–276 (1997).
Leboulleux, S. et al. Post-radioiodine treatment whole body scan in the era of fluorodesoxyglucose positron emission tomography for differentiated thyroid carcinoma with elevated serum thyroglobulin levels. Thyroid 22, 832–838 (2012).
Shah, S. & Boucai, L. Effect of age on response to therapy and mortality in patients with thyroid cancer at high risk of recurrence. J. Clin. Endocrinol. Metab. 103, 689–697 (2018).
Travagli, J. P. et al. Combination of radioiodine (131I) and probe-guided surgery for persistent or recurrent thyroid carcinoma. J. Clin. Endocrinol. Metab. 83, 2675–2680 (1998).
Hartl, D. M. et al. Charcoal suspension tattoo localization for differentiated thyroid cancer recurrence. Ann. Surg. Oncol. 16, 2602–2608 (2009).
Lamartina, L. et al. Surgery for neck recurrence of differentiated thyroid cancer: outcomes and risk factors. J. Clin. Endocrinol. Metab. 102, 1020–1031 (2017).
Pacini, F. et al. Outcome of 309 patients with metastatic differentiated thyroid carcinoma treated with radioiodine. World J. Surg. 18, 600–604 (1994).
Hay, I. D., Lee, R. A., Davidge-Pitts, C., Reading, C. C. & Charboneau, J. W. Long-term outcome of ultrasound-guided percutaneous ethanol ablation of selected “recurrent” neck nodal metastases in 25 patients with TNM stages III or IVA papillary thyroid carcinoma previously treated by surgery and 131I therapy. Surgery 154, 1448–1454 (2013); discussion 1454–1455 (2013).
Kitamura, Y. et al. Immediate causes of death in thyroid carcinoma: clinicopathological analysis of 161 fatal cases. J. Clin. Endocrinol. Metab. 84, 4043–4049 (1999).
Hartl, D. M. et al. Surgery in the context of kinase inhibitor therapy for locally invasive thyroid cancer. Eur. J. Surg. Oncol. 46, 650–655 (2020).
Berdelou, A. et al. Treatment of refractory thyroid cancer. Endocr. Relat. Cancer 25, R209–R223 (2018).
Tuttle, R. M. et al. Novel concepts for initiating multitargeted kinase inhibitors in radioactive iodine refractory differentiated thyroid cancer. Best Pract. Res. Clin. Endocrinol. Metab. 31, 295–305 (2017).
Miyauchi, A. et al. Prognostic impact of serum thyroglobulin doubling-time under thyrotropin suppression in patients with papillary thyroid carcinoma who underwent total thyroidectomy. Thyroid 21, 707–716 (2011).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECISTguideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
Sabra, M. M., Sherman, E. J. & Tuttle, R. M. Tumor volume doubling time of pulmonary metastases predicts overall survival and can guide the initiation of multikinase inhibitor therapy in patients with metastatic, follicular cell-derived thyroid carcinoma. Cancer 123, 2955–2964 (2017).
Barat, M. et al. Thermal-ablation of vertebral metastases prevents adverse events in patients with differentiated thyroid carcinoma. Eur. J. Radiol. 119, 108650 (2019).
Quan, G. M., Pointillart, V., Palussière, J. & Bonichon, F. Multidisciplinary treatment and survival of patients with vertebral metastases from thyroid carcinoma. Thyroid 22, 125–130 (2012).
Farooki, A., Leung, V., Tala, H. & Tuttle, R. M. Skeletal-related events due to bone metastases from differentiated thyroid cancer. J. Clin. Endocrinol. Metab. 97, 2433–2439 (2012).
Maxon, H. R. et al. Relation between effective radiation dose and outcome of radioiodine therapy for thyroid cancer. N. Engl. J. Med. 309, 937–941 (1983).
Pötzi, C. et al. Comparison of iodine uptake in tumour and nontumour tissue under thyroid hormone deprivation and with recombinant human thyrotropin in thyroid cancer patients. Clin. Endocrinol. 65, 519–523 (2006).
Deandreis, D. et al. Comparison of empiric versus whole body/blood clearance dosimetry-based approach to radioactive iodine treatment in patients with metastases from differentiated thyroid cancer. J. Nucl. Med. 58, 717–722 (2017); correspondence 863–864 and 1531 (2017).
Sgouros, G. et al. Patient-specific dosimetry for 131I thyroid cancer therapy using 124I PET and 3-dimensional-internal dosimetry (3D-ID) software. J. Nucl. Med. 45, 1366–1372 (2004).
Plyku, D. et al. Recombinant human thyroid-stimulating hormone versus thyroid hormone withdrawal in 124I PET/CT-based dosimetry for 131I therapy of metastatic differentiated thyroid cancer. J. Nucl. Med. 58, 1146–1154 (2017).
Klubo-Gwiezdzinska, J. et al. Efficacy of dosimetric versus empiric prescribed activity of 131I for therapy of differentiated thyroid cancer. J. Clin. Endocrinol. Metab. 96, 3217–3225 (2011).
Robbins, R. J. et al. Real-time prognosis for metastatic thyroid carcinoma based on 2-[18F]fluoro-2-deoxy-D-glucose-positron emission tomography scanning. J. Clin. Endocrinol. Metab. 91, 498–505 (2006).
Schlumberger, M., Lacroix, L., Russo, D., Filetti, S. & Bidart, J. M. Defects in iodide metabolism in thyroid cancer and implications for the follow-up and treatment of patients. Nat. Rev. Endocrinol. 3, 260–269 (2007).
Schlumberger, M. et al. Definition and management of radioactive iodine-refractory differentiated thyroid cancer. Lancet Diabetes Endocrinol. 2, 356–358 (2014).
Brose, M. S. et al. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Lancet 384, 319–328 (2014); correspondence 228–229 (2015).
Schlumberger, M. et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N. Engl. J. Med. 372, 621–630 (2015); correspondence 1868 (2015).
Brose, M. S., Worden, F. P., Newbold, K. L., Guo, M. & Hurria, A. Effect of age on the efficacy and safety of lenvatinib in radioiodine-refractory differentiated thyroid cancer in the phase III SELECT trial. J. Clin. Oncol. 35, 2692–2699 (2017).
Berdelou, A. et al. Lenvatinib for the treatment of radio-iodine refractory thyroid cancer in real-life practice. Thyroid 28, 72–78 (2018).
Locati, L. D. et al. Real-world efficacy and safety of lenvatinib: data from a compassionate use in the treatment of radioactive iodine-refractory differentiated thyroid cancer patients in Italy. Eur. J. Cancer 118, 35–40 (2019).
Locati, L. D. et al. Treatment of advanced thyroid cancer with axitinib: phase 2 study with pharmacokinetic/pharmacodynamic and quality-of-life assessments. Cancer 120, 2694–2703 (2014).
Cabanillas, M. E. et al. Cabozantinib as salvage therapy for patients with tyrosine kinase inhibitor-refractory differentiated thyroid cancer: results of a multicenter phase II International Thyroid Oncology Group trial. J. Clin. Oncol. 35, 3315–3321 (2017).
Bible, K. C. et al. Efficacy of pazopanib in progressive, radioiodine-refractory, metastatic differentiated thyroid cancers: results of a phase 2 consortium study. Lancet Oncol. 11, 962–972 (2010).
Lamartina, L. et al. Anti-angiogenic tyrosine kinase inhibitors: occurrence and risk factors of hemoptysis in refractory thyroid cancer. J. Clin. Endocrinol. Metab. 101, 2733–2741 (2016).
Wirth, L. J. et al. Efficacy of selpercatinib in RET-altered thyroid cancers. N. Engl. J. Med. 383, 825–835 (2020).
Hu, M. et al. Clinical activity of selective RET inhibitor, BLU-667, in advanced RET-altered thyroid cancers: updated results from the phase 1 ARROW study [abstract]. Thyroid 28 (Suppl. 1), A170 (2018).
Drilon, A., Hu, Z. I., Lai, G. G. Y. & Tan, D. S. W. Targeting RET-driven cancers: lessons from evolving preclinical and clinical landscapes. Nat. Rev. Clin. Oncol. 15, 151–167 (2018).
Shah, M. H. et al. Results of randomized phase II trial of dabrafenib versus dabrafenib plus trametinib in BRAF-mutated papillary thyroid carcinoma [abstract]. J. Clin. Oncol. 35 (Suppl. 15), 6022 (2017).
Ho, A. L. et al. Selumetinib-enhanced radioiodine uptake in advanced thyroid cancer. N. Engl. J. Med. 368, 623–632 (2013).
Rothenberg, S. M., McFadden, D. G., Palmer, E. L., Daniels, G. H. & Wirth, L. J. Redifferentiation of iodine-refractory BRAF V600E-mutant metastatic papillary thyroid cancer with dabrafenib. Clin. Cancer Res. 21, 1028–1035 (2015).
Leboulleux, S. et al. Redifferentiation of a BRAF-K601E mutated poorly differentiated thyroid cancer patient with dabrafenib and trametinib treatment. Thyroid 29, 735–742 (2019).
Mehnert, J. M. et al. Pembrolizumab for advanced papillary or follicular thyroid cancer: preliminary results from the phase 1b KEYNOTE-028 study [abstract]. J. Clin. Oncol. 34 (Suppl. 15), 6091 (2016).
Lorch, J. H. et al. A phase II study of nivolumab (N) plus ipilimumab (I) in radioidine refractory differentiated thyroid cancer (RAIR DTC) with exploratory cohorts in anaplastic (ATC) and medullary thyroid cancer (MTC) [abstract]. J. Clin. Oncol. 38 (Suppl. 15), 6513 (2020).
Haugen, B. et al. Lenvatinib plus pembrolizumab combination therapy in patients with radioiodine-refractory (RAIR), progressive differentiated thyroid cancer (DTC): results of a multicenter phase II international thyroid oncology group trial [absdtract]. J. Clin. Oncol. 38 (Suppl. 15), 6512 (2020).
Burman, B. et al. Radioiodine (RAI) in combination with durvalumab for recurrent/metastatic thyroid cancers? [abstract]. J. Clin. Oncol. 38 (Suppl. 15), 6587 (2020).
Van Herle, A. J., Uller, R. P., Matthews, N. I. & Brown, J. Radioimmunoassay for measurement of thyroglobulin in human serum. J. Clin. Invest. 52, 1320–1327 (1973).
Schlumberger, M. et al. Circulating thyroglobulin and thyroid hormones in patients with metastases of differentiated thyroid carcinoma: relationship to serum thyrotropin levels. J. Clin. Endocrinol. Metab. 51, 513–519 (1980).
Haugen, B. R. et al. A comparison of recombinant human thyrotropin and thyroid hormone withdrawal for the detection of thyroid remnant or cancer. J. Clin. Endocrinol. Metab. 84, 3877–3885 (1999).
Pacini, F. et al. Radioiodine ablation of thyroid remnants after preparation with recombinant human thyrotropin in differentiated thyroid carcinoma: results of an international, randomized, controlled study. J. Clin. Endocrinol. Metab. 91, 926–932 (2006).
Schlumberger, M., Ricard, M., De Pouvourville, G. & Pacini, F. How the availability of recombinant human TSH has changed the management of patients who have thyroid cancer. Nat. Rev. Endocrinol. 3, 641–650 (2007).
Brassard, M. et al. Long-term follow-up of patients with papillary and follicular thyroid cancer: a prospective study on 715 patients. J. Clin. Endocrinol. Metab. 96, 1352–1359 (2011).
Netzel, B. C. et al. Thyroglobulin (Tg) testing revisited: Tg assays, TgAb assays, and correlation of results with clinical outcomes. J. Clin. Endocrinol. Metab. 100, 1074–1083 (2015).
Spencer, C. & Fatemi, S. Thyroglobulin antibody (TgAb) methods—strengths, pitfalls and clinical utility for monitoring TgAb-positive patients with differentiated thyroid cancer. Best. Pract. Res. Clin. Endocrinol. Metab. 27, 701–712 (2013).
Leboulleux, S. et al. Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J. Clin. Endocrinol. Metab. 92, 3590–3594 (2007).
Leenhardt, L. et al. European Thyroid Association guidelines for cervical ultrasound scan and ultrasound-guided techniques in the postoperative management of patients with thyroid cancer. Eur. Thyroid. J. 2, 147–159 (2013).
Pacini, F. et al. Detection of thyroglobulin in fine needle aspirates of nonthyroidal neck masses: a clue to the diagnosis of metastatic differentiated thyroid cancer. J. Clin. Endocrinol. Metab. 74, 1401–1404 (1992).
Leboulleux, S., Schroeder, P. R., Schlumberger, M. & Ladenson, P. W. The role of PET in follow-up of patients treated for differentiated epithelial thyroid cancers. Nat. Rev. Endocrinol. 3, 112–121 (2007).
Wu, D. et al. 124I positron emission tomography/computed tomography versus conventional radioiodine imaging in differentiated thyroid cancer: a review. Thyroid 29, 1523–1535 (2019).
Padovani, R. P. et al. One month is sufficient for urinary iodine to return to its baseline value after the use of water-soluble iodinated contrast agents in post-thyroidectomy patients requiring radioiodine therapy. Thyroid 22, 926–930 (2012).
Aide, N. et al. Clinical relevance of single-photon emission computed tomography/computed tomography of the neck and thorax in postablation (131)I scintigraphy for thyroid cancer. J. Clin. Endocrinol. Metab. 94, 2075–2084 (2009).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
M.S. and S.L. have received personal fees and research support from Bayer, Eisai, Exilixis-IPSEN and Sanofi-Genzyme. No financial support was received from these entities for writing this review.
Additional information
Peer review information
Nature Reviews Endocrinology thanks A. Shaha and F. Verburg for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Thyroid Cancer Genome Atlas (TCGA): https://www.cancer.gov/about-nci/organization/ccg/research/structural-genomics/tcga/studied-cancers/thyroid
Supplementary information
Rights and permissions
About this article
Cite this article
Schlumberger, M., Leboulleux, S. Current practice in patients with differentiated thyroid cancer. Nat Rev Endocrinol 17, 176–188 (2021). https://doi.org/10.1038/s41574-020-00448-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-020-00448-z
This article is cited by
-
Imprinted gene detection effectively improves the diagnostic accuracy for papillary thyroid carcinoma
BMC Cancer (2024)
-
Cytosolic Cadherin 4 promotes angiogenesis and metastasis in papillary thyroid cancer by suppressing the ubiquitination/degradation of β-catenin
Journal of Translational Medicine (2024)
-
Bioinformatics analysis for the identification of Sprouty-related EVH1 domain-containing protein 3 expression and its clinical significance in thyroid carcinoma
Scientific Reports (2024)
-
Successful localisation of recurrent thyroid cancer using preoperative patent blue dye injection
Journal of Endocrinological Investigation (2024)
-
DNMT1/DNMT3a-mediated promoter hypermethylation and transcription activation of ICAM5 augments thyroid carcinoma progression
Functional & Integrative Genomics (2024)