Abstract
Current countermeasures for preventing hypertension emphasize only improvements to lifestyle. Recently, improving life environment has attracted attention, in parallel with publication of the WHO Housing and health guidelines. We quantitatively evaluated the relationship between housing thermal environment and blood pressure (BP) in a real-world setting. We conducted a nationwide, prospective intervention study—the Smart Wellness Housing survey—in Japan, as a non-randomized controlled trial. The intervention was the retrofitting of thermal insulation in houses. Participant recruitment was done by construction companies in all 47 prefectures of Japan. Measurements of home BP and indoor temperature at 1.0 m above the floor in the living room, changing room, and bedroom were taken for 2 weeks before and after the intervention each winter (November–March) of FY 2014–2019. As of July 2022, over 2500 households and 5000 participants were registered in the database. We found that (1) about 90% of Japanese lived in cold homes (minimum indoor temperature <18 °C), (2) indoor temperature was non-linearly associated with home BP, (3) morning systolic BP (SBP) was more sensitive than evening SBP to changes in indoor temperature, (4) SBP was influenced by indoor temperature change particularly in older participants and women, (5) unstable indoor temperature was associated with large BP variability, and (6) insulation retrofitting intervention significantly reduced home BP, especially in hypertensive patients. We proposed that the BP reduction effect of the life-environment is comparable to that achievable by lifestyle.
Similar content being viewed by others
Introduction
Excess winter mortality (EWM), which refers to the marked increase in mortality rate in winter, is a global problem in public health [1, 2]. Paradoxically, however, studies in Europe [3,4,5], the USA [6, 7], and Asia [8, 9] have reported higher EWM in areas with milder winter climates. One possible explanation for this is that houses in these areas are less adequately prepared for winter conditions. More than half of EWM is caused by cardiovascular disease (CVD) [10], a phenomenon which is partially attributable to cold-induced hypertension.
Hypertension is called a “silent killer” as it has almost no subjective symptoms [11]. Indeed, many hypertensive patients are unaware of their hypertension [12]. Reliance on antihypertensive drugs alone might be an inadequate, high-risk strategy—a likely better strategy would involve shifting the BP of the total population in the desirable direction. However, existing population strategies exclusively emphasize improvements to lifestyle, focusing on habits such as physical activity, diet, smoking and alcohol consumption; improving the housing thermal environment has been neglected.
In 2018, the WHO issued the Housing and health guidelines, which focused on “low indoor temperatures and insulation” [13]. Based on a systematic review of evidence the guidelines recommend a minimum indoor temperature of 18 °C, stating that low indoor temperature can lead to vasoconstriction—a known risk factor of hypertension—and that retrofitting insulation into existing housing can alleviate the negative effects of low indoor temperature on health. The guidelines call for research to establish the appropriateness of 18 °C as a general target for a minimum indoor temperature or whether this target should vary in different populations. The guidelines also emphasize the desirability of further evidence on the effects of living in a thermally insulated home on health outcomes.
Consistent with the above background, we started a nationwide, prospective intervention trial, the “Smart Wellness Housing (SWH) survey” in Japan, to quantitatively evaluate the health effects of indoor temperature and insulation retrofitting of houses.
Study design of the Smart Wellness Housing survey
The SWH survey was designed with two validation patterns, prepared from short- and long-term viewpoints (Fig. 1). The survey started in winter 2014, and collected all data used in the “before and after insulation study” described below. Construction companies recruited participants throughout all 47 prefectures of Japan, and more than 2500 households and 5000 participants were registered in the SWH survey database as of July 2022.
-
(1)
Before and after insulation study [University Hospital Medical Information
Network Clinical Trials Registry (UMIN-CTR) Trial No. UMIN000030601]
This study was a non-randomized controlled trial with groups categorized according to participants’ choice of whether or not to conduct insulation retrofitting. This intervention included a range of treatments, including heat-insulation work on the outer walls, floor and/or roof; replacing single-glazed with double-glazed windows; and replacing window frames. Thermal insulation performance level after retrofitting was set to meet the S standards (approximately equivalent to a long-life newly built, high-quality house) or A standards (lower than S standards but expected to provide consistently improved performance) of the ‘Act on the Promotion of Dissemination of Long-Lasting Quality Housing’ in Japan [14]. This study investigated short-term changes in indoor environment and participants’ health pre- and post-insulation retrofitting.
-
(2)
Long-term cohort study (UMIN-CTR Trial No. UMIN000042196)
This cohort study aims to evaluate long-term health effects in relation to differences in thermal insulation level. It is being conducted by a follow-up survey of households for more than 5 years after the completion of insulation retrofitting. Houses with no insulation retrofitting were randomly selected and included as a control group.
Participants measured the indoor thermal environment and their home blood pressure (HBP), and kept a diary for 2 weeks, mainly during winter (November–March). They also responded to a questionnaire during the same period. Indoor temperature and relative humidity at 1.0 m above the floor were monitored in the living room, changing room, and bedroom at 10-min intervals by automated monitoring sensors supplied by the investigators and installed by the participants. HBP was also measured twice in the morning and twice in the evening, in accordance with the Japanese guideline [15]. Health checkup data [e.g., blood lipids, blood glucose, and electrocardiogram (ECG)] were also collected whenever possible.
Indoor temperature in Japan and high-risk residents
Japan stretches across several climate zones from north to south. The climate is mostly temperate, but becomes subarctic mainly in Hokkaido. According to data from the Ministry of Land, Infrastructure, Transport and Tourism, 30% of the ~50 million houses in Japan are without insulation, and in 2018, only 11% were sufficiently insulated to meet the country’s highest thermal insulation standards [16]. Furthermore, in contrast to the continuous heating of entire buildings typical in Europe and the USA, intermittent heating of the living room only is the general practice in Japan. Therefore, there is concern that indoor temperatures in Japan may be lower than in European and American countries.
We reported the actual status of houses throughout Japan before insulation retrofitting [17]. Cross-sectional analyses involving 2190 houses revealed average temperatures when participants were at home in the living room and changing room of 16.8 °C and 13.0 °C, respectively, and 12.8 °C when participants slept in the bedroom. Minimum temperatures in the living room, changing room, and bedroom were 12.6 °C, 10.4 °C, and 11.2 °C, respectively. Minimum temperatures were below the 18 °C recommended in the WHO guidelines in over 90% of households. A comparison of average living room temperatures across prefectures is shown in Fig. 2. The highest temperature (19.8 °C) was in Hokkaido, where the climate is severe and houses have higher thermal insulation criteria than in other areas. In contrast, the lowest average living room temperature (13.1 °C) was in Kagawa, with a mild climate. The maximum difference between prefectures was 6.7 °C.
Average living room temperature at home in each prefecture from ref. [17] †Excluding prefectures with data from 5 participating households or less (displayed in white)
We also examined characteristics common to residents of cold houses. Lower household income was a risk factor for living in cold houses, likely because it may force residents to use heating sparingly or to live in houses with poor insulation. Single-person household was also a risk factor. Furthermore, lower room temperature was associated with the use of a kotatsu (traditional Japanese heating device which does not heat an entire room) and wearing of multiple layers of clothes. These results will aid in identifying “high-risk” residents in greater need of active housing intervention.
Separately to our study, Saeki et al. reported that mean living room/bedroom temperature was 16.1/12.6 °C in the cold season (October–April) in the Kansai region [18], and Uchiyama et al. found that mean temperature in the living room in 602 houses throughout Japan was 17 °C during winter (January–March) [19], which was almost the same as our result. Elsewhere, French et al. collected indoor temperatures of 397 houses in New Zealand during the winter season and reported mean living room daytime temperatures and nighttime bedroom temperatures of 15.8 °C and 13.6 °C, respectively [20], similar to Japan. In contrast, a study which reviewed indoor temperatures in UK homes reported average winter living room temperatures of 18–21 °C [21], while the average winter living room temperature in New York apartments was 23.3 °C [22], indicating more comfortable conditions in Europe and the USA than Japan. However, even in European and American countries, fuel (or energy) poverty, defined as an energy cost of maintaining an adequate indoor temperature of more than 10% of household income, is a prevalent problem [23, 24]. Thus, we note that living in cold homes is an issue not only in Japan, but also in some other countries.
Indoor temperature and blood pressure
As described above, we established that many Japanese people live in cold homes. In view of the concern that low indoor temperatures causes high blood pressure, we analyzed the association between HBP and indoor winter temperature using a multilevel model [25]. Cross-sectional analyses based on ~33,000 data points derived from 2900 residents revealed that HBP had a significant inverse association with indoor temperature: HBP was higher at low indoor temperatures. Of note, systolic blood pressure (SBP) was significantly more sensitive to changes in indoor temperature in the morning (8.2 mmHg increase/10 °C decrease) than in the evening (6.5 mmHg increase/10 °C decrease) in residents aged 57 years (mean age of participants in this survey). Because CVD-related crises occur frequently in the morning [26,27,28,29] and morning HBP strongly predicts cardiovascular events [30,31,32,33,34,35], this finding strengthens the importance of morning indoor temperature management in reducing the danger from CVDs.
We found a nonlinear cubic relationship between morning SBP and indoor temperature, illustrated in Fig. 3. The relationship between HSBP and indoor temperature was weaker at low and high temperature ranges. This might be a consequence of thermoregulatory behaviors such as adding or removing clothes at low and high temperatures, and of limitations in thermophysiological reactions including vasoconstriction and vasodilatation. However, this evidence also highlights the importance of indoor temperature even if not extremely low, because SBP changes steeply at the middle temperature range. A previous systematic review and meta-analysis [36] did not determine optimum home temperature because it considered the temperature–BP relationship as a linear function. Therefore, we propose that the nonlinear temperature–BP relationship revealed in our study can contribute towards establishing optimum home temperature recommendations
Relationship between indoor ambient temperature and morning systolic blood pressure from ref. [25] †Average values for male/female participants in the Smart Wellness Housing survey were inputted into the multilevel model in ref. [25]: vegetable consumption = regularly, exercise = rarely, current smoking status = nonsmoker, alcohol consumption = every day/none, antihypertensive drug use = none. JSH indicates Japanese Society of Hypertension; and HSBP, home systolic blood pressure
We also found that SBP in older residents as well as women was particularly susceptible to indoor temperature change. Possible causes here are vascular endothelial dysfunction and diminished physiological adaptability (e.g., vasodilatation) to indoor temperature variations in older residents. Additionally, older residents and women have decreased muscle mass compared with younger residents and men, which translates to reduced metabolic heat production and increased vulnerability to cold. For these reasons, recommendations concerning optimum home temperature should be tailored according to population group, a topic identified as requiring future research in the WHO Housing and health guidelines.
Recently, Tai et al. [37] examined the relationship between ambulatory BP and skin temperature among 584 older adults, showing that the mediation effect of skin temperature and importance of distal skin temperature. This evidence promotes an understanding of the underlying thermophysiological mechanism and provides a clue of controlling BP.
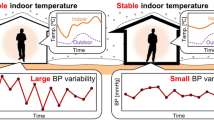
Indoor temperature instability and blood pressure variability
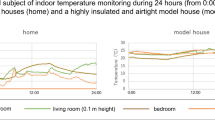
In addition to BP level, BP variability requires due consideration when evaluating the risk of cardiovascular events. We hypothesized that a stable home thermal environment helps to reduce BP variability, and evaluated the indoor temperature–BP relationship from another perspective [38]. Over a 2-week period we used the morning-evening (ME) difference as an index of diurnal variability, and the standard deviation (SD), coefficient of variation (CV), variability independent of the mean (VIM) as well as average real variability (ARV) as indices of day-by-day variability. The mean ME difference in indoor/outdoor temperature (overnight decrease) was 3.2/1.5 °C, and the mean indoor/outdoor temperature SD was 1.6/2.5 °C. As shown in Fig. 4, compared to participants living in houses with an overnight indoor temperature decrease (ME difference in indoor temperature) of less than 1 °C, the ME difference in SBP was more than double in participants living in houses with an ME difference in indoor temperature ≥4 °C. Concerning day-by-day variability, compared to participants whose houses had an indoor temperature SD < 1 °C, the SD of SBP was larger in participants whose houses had an SD ≥ 4 °C. Linear regression analyses adjusted for confounders showed a strong correlation between the ME difference in indoor temperature and the ME difference in SBP. The indoor temperature SD also showed an association with the SBP SD. Trends for CV, VIM, and ARV were similar to BP SD. By contrast, instability in outdoor temperature showed an association with neither diurnal nor day-by-day HBP variability. Of interest, Nakagami et al. [39] evaluated the effect of houses on BP level and variability by comparing 24-h BP at home and at a highly insulated model house. They found that residents who usually lived in a cold house had lower BP and smaller BP variability when in the model house, where indoor temperature was high and stable. Given that Narita et al. [40] showed that day-by-day HBP variability is more strongly associated with future CVD events in winter than in other seasons, these findings show that winter residents should keep the indoor temperature not only warm but stable to reduce BP level and variability.
Relationship between blood pressure variability and indoor temperature instability re-edited from ref. [37] †A: morning-evening (ME) difference in systolic blood pressure (SBP) and ME difference in indoor temperature. B: standard deviation (SD) of SBP and SD of indoor temperature. The plot shows the average of each group, and the error bar shows the 95% confidence interval. SD was calculated from a 2-week measurement. ME average was used as a representing value of each day when calculating SD
BP also shows long-term fluctuations [41, 42]; these include seasonal variation, which has been associated with cardiovascular events [43]. Several recent papers have summarized evidence on seasonal BP variation [44, 45], one of which recommended optimizing environmental factors such as room temperature and housing conditions to avoid excessive seasonal BP change [45]. We plan to analyze the association between indoor temperature and seasonal BP variation in a future paper using BP data collected from optional surveys in summer.
Interventions to retrofit houses with insulation and heating
In the previous sections, we analyzed baseline data before insulation retrofitting. In this section, we present a longitudinal analysis of pre- and post-intervention data to clarify changes in HBP following insulation retrofitting by comparing HBP in the retrofitting and non-retrofitting groups [46]. Morning indoor temperature rose by 1.5 °C after insulation retrofitting, in spite of a slight decrease in outdoor temperature. Retrofitting insulation significantly reduced all four HBP indices (SBP and DBP in the morning and evening), for example morning SBP by 3.1 mmHg. Furthermore, we found a dose–response relationship between increased indoor temperature and decreased HBP, confirming that simple improvements in the thermal environment indoors can be effective. Another finding, shown in Fig. 5, was of greater heterogeneity in the effects of retrofitting insulation on morning SBP in self-reported hypertensive patients compared to normotensive occupants (–7.7 vs –2.2 mmHg). This indicates that the effects of insulation retrofitting were especially valuable in subgroups having a high risk of CVD.
Change in morning home systolic blood pressure (HSBP) following insulation retrofitting by subgroup from ref. [45] †Each value shows the regression coefficient of multiple linear regression model adjusted for confounders. Blue bars indicate subgroups at high risk of cardiovascular diseases and red bars indicate subgroups at low risk of cardiovascular diseases
A study of heating intervention and BP was conducted in Japan by Saeki et al. [47], in which physicians provided instructions to the participants on how to use their heating. This intervention on heating usage significantly decreased SBP and DBP by 4.4 and 2.3 mmHg, respectively, and the author recommended further research into the combination of insulation retrofitting and heating. A second intervention study combining insulation retrofitting and heating was conducted in Scotland by Lloyd et al. [48]. They examined improvements in BP produced by home renovation which included introduction of insulation material and central heating systems. The intervention significantly decreased SBP and DBP by 22 and 20 mmHg, respectively. Allowing that the sample size of this study was small, the combined effect of insulation retrofitting and heating appeared to greatly influence BP.
Messages from the Smart Wellness Housing survey
We reviewed the effects of indoor temperature and insulation retrofitting on BP, focusing mainly on the national Smart Wellness Housing survey. In summary, we found: (1) about 90% of Japanese lived in cold homes (minimum indoor temperature <18 °C); (2) indoor temperature was nonlinearly associated with BP; (3) morning SBP was more sensitive to changes in indoor temperature than evening SBP; (4) SBP in older residents and women was particularly susceptible to indoor temperature change; (5) unstable indoor temperature was associated with large BP variability; and (6) insulation retrofitting intervention significantly reduced BP, especially in hypertensive patients.
A systematic review [49] showed significant quantitative effects of lifestyle improvements including diet, aerobic exercise, alcohol and sodium restriction, as well as fish oil supplements on BP, namely mean reductions in SBP of 5.0, 4.6, 3.8, 3.6, and 2.3 mmHg, respectively. As described above, our study showed a significant morning SBP reduction of 3.1 mmHg following the insulation retrofitting of houses. Saeki et al. also showed SBP reduction effects of 4.4 mmHg by heating. Although evidence from housing environment interventions is scarce, we expect that the life-environment can exert a BP reduction effect comparable to that associated with lifestyle changes. At present, hypertension and CVDs are widely regarded as lifestyle diseases. However, we consider these diseases to be not only lifestyle diseases but also life-environment diseases, based on the SWH survey and previous research which proposed housing as one of the factors determining BP [50]. Our suggestion from this review is shown in Fig. 6. Although the present Japanese health policy [Health Japan 21 (the Second Term)] includes lifestyle factors only, such as diet, exercise, and alcohol consumption [51], “housing” should be included to further decrease BP and the number of deaths due to CVDs.
Expanded hierarchical structure for prevention of cardiovascular diseases including housing based on the present Japanese health policy “Health Japan 21 (the second term)” †Decreases in systolic blood pressure (SBP) by lifestyle modifications (e.g., 2.3 mmHg decrease by diet) and prevention effects on cardiovascular diseases (e.g., the prevention of 9,300 deaths/year due to cerebrovascular disease by 4.0 mmHg decrease in SBP) were quantified mainly based on epidemiological evidence
The Smart Wellness Housing cohort survey
In today’s society, most people spend from 60% to 70% of their time at home [52,53,54]. It is therefore conceivable that our present findings on the short-term effect underestimate the effects of housing on BP, and so it is necessary to evaluate the long-term effect of housing on BP. We hypothesized that living in a cold home for more than 5 years had an adverse cumulative effect on cardiovascular health. We named this effect “cold debt”, with reference to sleep debt [55], which is a state of chronic sleep deprivation leading to physical and mental disorders.
In addition to the results presented in this review, the SWH survey revealed that the number of residents with high cholesterol was larger in colder homes [56]. A long-term risk of progression of arteriosclerosis is therefore present. We also found that a greater number of residents in colder homes had abnormal ECGs [57], which we assume to be a long-term consequence. In conclusion, as shown in Fig. 1, we started the Smart Wellness Housing cohort survey to clarify whether cold debt exists or not.
Conclusion
The present review organizing evidence on housing and BP control indicated that housing has great potential for the prevention of hypertension in winter and the mitigation of EWM due to CVDs. We recommend life-environment improvements as well as lifestyle modifications to gain the additional benefit of decreasing patients with hypertension and CVDs. At present, as a target of life-environment improvements, 18 °C is widely accepted in general. However, it should be personalized depending on characteristics of residents because our evidence showed that vulnerability to indoor temperature was significantly different in each population group (e.g., age, gender). As a means of life-environment improvements, thermal insulation retrofit of houses was effective for a reduction in BP. We believe that the combination of insulation retrofit and appropriate heating use further enhance the importance of life-environment improvements in BP control.
References
The Eurowinter Group. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet. 1997;349:1341–6. https://doi.org/10.1016/S0140-6736(96)12338-2
Wilkinson P, Landon M, Armstrong B, Stevenson S, Pattenden S, McKee M, et al. Cold comfort: the social and environmental determinants of excess winter deaths in England, 1986–96. London, United Kingdom: Policy Press. 2001. https://www.jrf.org.uk/report/cold-comfort-social-and-environmental-determinants-excess-winter-deaths-england-1986-1996 Accessed 23 Jun 2022.
Healy JD. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Commun Health. 2003;57:784–9. https://doi.org/10.1136/jech.57.10.784
Analitis A, Katsouyanni K, Biggeri A, Baccini M, Forsberg B, Bisanti L, et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol. 2008;168:1397–408. https://doi.org/10.1093/aje/kwn266
Fowler T, Southgate RJ, Waite T, Harrell R, Kovats S, Bone A, et al. Excess winter deaths in Europe: a multi-country descriptive analysis. Eur J Public Health. 2015;25:339–45. https://doi.org/10.1093/eurpub/cku073
Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–7. https://doi.org/10.1093/aje/155.1.80
Gonseth S, Nusslé S, Bovet P, Panese F, Wiemels JL. Excess winter deaths caused by cardiovascular diseases are associated with both mild winter temperature and socio-economic inequalities in the U.S. Int J Cardiol. 2015;187:642–4. https://doi.org/10.1016/j.ijcard.2015.03.412
Yang J, Yin P, Zhou M, Ou CQ, Guo Y, Gasparrini A, et al. Cardiovascular mortality risk attributable to ambient temperature in China. Heart. 2015;101:1966–72. https://doi.org/10.1136/heartjnl-2015-308062
Chung Y, Lim YH, Honda Y, Guo YL, Hashizume M, Bell ML, et al. Mortality related to extreme temperature for 15 cities in northeast Asia. Epidemiology. 2015;26:255–62. https://doi.org/10.1097/EDE.0000000000000229
World Health Organization Europe. Environmental burden of disease associated with inadequate housing. 2011. http://www.euro.who.int/__data/assets/pdf_file/0017/145511/e95004sum.pdf Accessed 23 Jun 2022.
World Health Organization. A global brief on hypertension: silent killer, global public health crisis. 2013. http://apps.who.int/iris/bitstream/10665/79059/1/WHO_DCO_WHD_2013.2_eng.pdf Accessed 7 Jul 2022.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–50. https://doi.org/10.1161/CIRCULATIONAHA.115.018912
World Health Organization. Housing and health guidelines. 2018. https://www.who.int/sustainable-development/publications/housing-health-guidelines/en/. Accessed 7 Jul 2022.
Building Research Institute. Assessment standards on the quality of housing, act on the promotion of renovation into long-lasting quality housing in fiscal 2019 (in Japanese). 2019. http://h31.choki-reform.com/doc/val_basis_koubo_h31.pdf. Accessed 7 Jul 2022.
Imai Y, Kario K, Shimada K, Kawano Y, Hasebe N, Matsuura H, et al. The Japanese Society of Hypertension Guidelines for self-monitoring of blood pressure at home (second edition). Hypertens Res. 2012;35:777–95. https://doi.org/10.1038/hr.2012.56
Housing Bureau, Ministry of Land, Infrastructure, Transport and Tourism. The first session of the committee on energy saving measures for houses and buildings for a decarbonized society (in Japanese). 2021. https://www.mlit.go.jp/jutakukentiku/house/content/001400905.pdf Accessed 7 Jul 2022.
Umishio W, Ikaga T, Fujino Y, Ando S, Kubo T, Nakajima Y, et al. Disparities of indoor temperature in winter: a cross-sectional analysis of the Nationwide Smart Wellness Housing Survey in Japan. Indoor Air. 2020;30:1317–28. https://doi.org/10.1111/ina.12708
Saeki K, Obayashi K, Iwamoto J, Tone N, Okamoto N, Tomioka K, et al. Stronger association of indoor temperature than outdoor temperature with blood pressure in colder months. J Hypertens. 2014;32:1582–9. https://doi.org/10.1097/HJH.0000000000000232
Uchiyama S, Tomizawa T, Tokoro A, Aoki M, Hishiki M, Yamada T, et al. Gaseous chemical compounds in indoor and outdoor air of 602 houses throughout Japan in winter and summer. Environ Res. 2015;137:364–72. https://doi.org/10.1016/j.envres.2014.12.005
French LJ, Camilleri MJ, Isaacs NP, Pollard AR. Temperatures and heating energy in New Zealand houses from a nationally representative study-HEEP. Energ Build. 2007;39:770–82. https://doi.org/10.1016/j.enbuild.2007.02.004
Vadodaria K, Loveday DL, Haines V. Measured winter and springtime indoor temperatures in UK homes over the period 1969–2010: a review and synthesis. Energy Pol. 2014;64:252–62. https://doi.org/10.1016/j.enpol.2013.07.062
Quinn A, Shaman J. Indoor temperature and humidity in New York City apartments during winter. Sci Total Environ. 2017;583:29–35. https://doi.org/10.1016/j.scitotenv.2016.12.183
Thomson H, Snell C, Bouzarovski S. Health, well-being and energy poverty in Europe: a comparative study of 32 European countries. Int J Environ Res Public Health. 2017;14:584. https://doi.org/10.3390/ijerph14060584
Mohr T. M. Fuel poverty in the US: evidence using the 2009 Residential Energy Consumption Survey. Energy Econ. 2018;74:360–9. https://doi.org/10.1016/j.eneco.2018.06.007
Umishio W, Ikaga T, Kario K, Fujino Y, Hoshi T, Ando S, et al. Cross-sectional analysis of the relationship between home blood pressure and indoor temperature in winter: a nationwide Smart Wellness Housing Survey in Japan. Hypertension. 2019;74:756–66. https://doi.org/10.1161/HYPERTENSIONAHA.119.12914
Muller JE, Tofler GH, Stone PH. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation. 1989;79:733–43. https://doi.org/10.1161/01.cir.79.4.733
Cohen MC, Rohtla KM, Lavery CE, Muller JE, Mittleman MA. Meta-analysis of the morning excess of acute myocardial infarction and sudden cardiac death. Am J Cardiol. 1997;79:1512–6. https://doi.org/10.1016/s0002-9149(97)00181-1
Elliott WJ. Circadian variation in the timing of stroke onset: a meta-analysis. Stroke. 1998;29:992–6. https://doi.org/10.1161/01.str.29.5.992
Omama S, Yoshida Y, Ogawa A, Onoda T, Okayama A. Differences in circadian variation of cerebral infarction, intracerebral haemorrhage and subarachnoid haemorrhage by situation at onset. J Neurol Neurosurg Psychiatry. 2006;77:1345–9. https://doi.org/10.1136/jnnp.2006.090373
Kario K, Saito I, Kushiro T, Teramukai S, Ishikawa Y, Mori Y, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational study. Hypertension. 2014;64:989–96. https://doi.org/10.1161/HYPERTENSIONAHA.114.04262
Kario K, Thijs L, Staessen JA. Blood pressure measurement and treatment decisions. Circ Res. 2019;124:990–1008. https://doi.org/10.1161/CIRCRESAHA.118.313219
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–5. https://doi.org/10.1097/00004872-199816070-00010
Kario K, Saito I, Kushiro T, Teramukai S, Tomono Y, Okuda Y, et al. Morning home blood pressure is a strong predictor of coronary artery disease: the HONEST study. J Am Coll Cardiol. 2016;67:1519–27. https://doi.org/10.1016/j.jacc.2016.01.037
Kario K, Iwashita M, Okuda Y, Sugiyama M, Saito I, Kushiro T, et al. Morning home blood pressure and cardiovascular events in Japanese hypertensive patients. Hypertension. 2018;72:854–61. https://doi.org/10.1161/HYPERTENSIONAHA.118.11388
Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: the Japan Morning Surge-Home Blood Pressure Study. Hypertension. 2016;68:54–61. https://doi.org/10.1161/HYPERTENSIONAHA.116.07201
Wang Q, Li C, Guo Y, Barnett AG, Tong S, Phung D, et al. Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci Total Environ. 2017;575:276–86. https://doi.org/10.1016/j.scitotenv.2016.10.019
Tai Y, Obayashi K, Yamagami Y, Saeki K. Inverse association of skin temperature with ambulatory blood pressure and the mediation of skin temperature in blood pressure responses to ambient temperature. Hypertension. 2022;79:1845–55. https://doi.org/10.1161/HYPERTENSIONAHA.122.19190
Umishio W, Ikaga T, Kario K, Fujino Y, Suzuki M, Ando S, et al. Impact of indoor temperature instability on diurnal and day-by-day variability of home blood pressure in winter: a nationwide Smart Wellness Housing survey in Japan. Hypertens Res. 2021;44:1406–16. https://doi.org/10.1038/s41440-021-00699-x
Nakagami H, Akiyama H, Otsuka H, Iwamae A, Yamada H. Blood pressure fluctuations and the indoor environment in a highly insulated and airtight model house during the cold winter season. Hypertens Res. 2022;45:1217–9. https://doi.org/10.1038/s41440-022-00928-x
Narita K, Hoshide S, Kario K. Seasonal variation in day-by-day home blood pressure variability and effect on cardiovascular disease incidence. Hypertension 2022. https://doi.org/10.1161/HYPERTENSIONAHA.122.19494.
Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–55. https://doi.org/10.1038/nrcardio.2013.1
Kario K. Evidence and perspectives on the 24-hour management of hypertension: hemodynamic biomarker-initiated ‘anticipation medicine’ for zero cardiovascular event. Prog Cardiovasc Dis. 2016;59:262–81. https://doi.org/10.1016/j.pcad.2016.04.001
Hanazawa T, Asayama K, Watabe D, Tanabe A, Satoh M, Inoue R, et al. Association between amplitude of seasonal variation in self-measured home blood pressure and cardiovascular outcomes: HOMED-BP (Hypertension Objective Treatment Based on Measurement By Electrical Devices of Blood Pressure) study. J Am Heart Assoc. 2018;7:e008509. https://doi.org/10.1161/JAHA.117.008509
Stergiou GS, Palatini P, Modesti PA, Asayama K, Asmar R, Bilo G, et al. Seasonal variation in blood pressure: evidence, consensus and recommendations for clinical practice. Consensus statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens. 2020;38:1235–43. https://doi.org/10.1097/HJH.0000000000002341
Narita K, Hoshide S, Kario K. Seasonal variation in blood pressure: current evidence and recommendations for hypertension management. Hypertens Res. 2021;44:1363–72. https://doi.org/10.1038/s41440-021-00732-z
Umishio W, Ikaga T, Kario K, Fujino Y, Hoshi T, Ando S, et al. Intervention study of the effect of insulation retrofitting on home blood pressure in winter: a nationwide Smart Wellness Housing survey. J Hypertens. 2020;38:2510–8. https://doi.org/10.1097/HJH.0000000000002535
Saeki K, Obayashi K, Kurumatani N. Short-term effects of instruction in home heating on indoor temperature and blood pressure in elderly people: a randomized controlled trial. J Hypertens. 2015;33:2338–43. https://doi.org/10.1097/HJH.0000000000000729
Lloyd EL, McCormack C, McKeever M, Syme M. The effect of improving the thermal quality of cold housing on blood pressure and general health: a research note. J Epidemiol Commun Health 2008;62:793–7. https://doi.org/10.1136/jech.2007.067835
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33. https://doi.org/10.1097/01.hjh.0000199800.72563.26
Yano Y. Blood pressure management in an ecosystem context. Hypertens Res. 2020;43:989–94. https://doi.org/10.1038/s41440-020-0464-7
Yokoyama T. National health promotion measures in Japan: health Japan 21(the second term). J Natl Inst Public Health. 2020;69:14–24. https://doi.org/10.20683/jniph.69.1_14
Leech JA, Nelson WC, Burnett RT, Aaron S, Raizenne ME. It’s about time: a comparison of Canadian and American time-activity patterns. J Expo Anal Environ Epid. 2002;12:427–32. https://doi.org/10.1038/sj.jea.7500244
Brasche S, Bischof W. Daily time spent indoors in German homes-baseline data for the assessment of indoor exposure of German occupants. Int J Hyg Environ Heal. 2005;208:247–53. https://doi.org/10.1016/j.ijheh.2005.03.003
Schweizer C, Edwards RD, Bayer-Oglesby L, Gauderman WJ, Ilacqua V, Jantunen MJ, et al. Indoor time-microenvironment-activity patterns in seven regions of Europe. J Expo Sci Environ Epid 2007;17:170–81. https://doi.org/10.1038/sj.jes.7500490
Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. https://doi.org/10.1016/S0140-6736(99)01376-8
Umishio W, Ikaga T, Kario K, Fujino Y, Suzuki M, Hoshi T, et al. Association between indoor temperature in winter and serum cholesterol: a cross-sectional analysis of the Smart Wellness Housing Survey in Japan. J Atheroscler Thromb. 2022; https://doi.org/10.5551/jat.63494
Umishio W, Ikaga T, Kario K, Fujino Y, Suzuki M, Ando S, et al. Electrocardiogram abnormalities in residents in cold homes: a cross-sectional analysis of the nationwide Smart Wellness Housing survey in Japan. Environ Health Prev. 2021;26:104. https://doi.org/10.1186/s12199-021-01024-1
Acknowledgements
We gratefully acknowledge the assistance and participation of various construction companies, researchers, and research committee members in all 47 prefectures in Japan for their role in the SWH survey. Members of the research committee for promotion of SWH who participated in the study are listed in the online Data Supplement (Supplementary Table 1).
Funding
This study was partly supported by the Ministry of Land, Infrastructure, Transport and Tourism as part of the Model Project for Promotion of SWH and a JSPS KAKENHI [Grant Number JP17H06151; Principal Investigator, Prof. Toshiharu Ikaga]. Funding organizations had no role in the study design, data collection, management, analysis, or interpretation, nor in the preparation of the article or the decision to submit it for publication.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
TI has received research grants from Tokyo Gas Co., Ltd., Osaka Gas Co., Ltd., Panasonic Homes Co. Ltd., Fuyo Home Co. Ltd., Asahi Kasei Homes Corp., LIXIL Corp., Azbil Corp., Kajima Corp., Shimizu Corp., Nice Corp., Japan Gas Association and Japan Sustainable Building Consortium. KK has received a research grant from Omron Healthcare Co., Ltd. YF has reported grants and personal fees from Saibugas Co., Ltd. MS has received non-restrictive research funds from Taiyo Nippon Sanso Corp. TH has received honorarium from LIXIL Corp. The above grants/funds/honoraria were all received outside the submitted work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Umishio, W., Ikaga, T., Kario, K. et al. Role of housing in blood pressure control: a review of evidence from the Smart Wellness Housing survey in Japan. Hypertens Res 46, 9–18 (2023). https://doi.org/10.1038/s41440-022-01060-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01060-6
Keywords
This article is cited by
-
Salt and seasonal variation research in Asia
Hypertension Research (2024)
-
Topics 2023 in Hypertension Research leading to guidelines in Asia
Hypertension Research (2023)
-
Digital hypertension towards to the anticipation medicine
Hypertension Research (2023)
-
Effects of indoor temperature and its fluctuation on blood pressure and its variability
International Journal of Biometeorology (2023)
-
Home blood pressure-centered approach – from digital health to medical practice: HOPE Asia Network consensus statement 2023
Hypertension Research (2023)