Abstract
Blood pressure (BP) measured in the clinic is subject to the white coat effect and does not always indicate the ‘usual’ BP. Ambulatory BP is the current gold standard, but remains inconvenient for routine use. Interest in automated BP, where the healthcare professional is absent from the examination room during BP measurement, is growing, as this reduces the white coat effect and yields BP values that are close to ambulatory readings. The aim of this study was to investigate how well automated office BP (AOBP), measured using the Omron HEM-907 device, compares with observed office BP (OOBP, healthcare professional remains in the examination room) and awake ambulatory BP (AABP) measurements. OOBP, AOBP and AABP were measured in 108 participants, with OOBP and AOBP measurements repeated 1 week later, following a standardised protocol. Average BP readings for visit one were 134 ± 18/77 ± 11 for OOBP, 131 ± 16/75 ± 11 for AOBP, and 133 ± 15/82 ± 12 for AABP. On both visits, automated readings were significantly lower than observed readings for both systolic and diastolic BP (P < 0.001 for both). Automated readings were also significantly lower than ambulatory readings, with a mean difference in systolic/diastolic BP of − 2 ± 11/− 7 ± 10 (P < 0.001 for both), with high correlations between the two modalities (r = 0.75 and r = 0.64, for systolic and diastolic BP, respectively, P < 0.001 for both). AOBP measured by the Omron HEM-907 is not associated with a white coat effect, unlike observed readings, and provides reproducible results and good correlations with ambulatory readings. Automated BP measured using the Omron HEM-907 is, therefore, a useful alternative to observed office readings.
Similar content being viewed by others
Introduction
Clinic (office) blood pressure (BP) has traditionally been measured manually by healthcare professionals. However, observed BP measurements have the well-known limitation of the white coat effect, where values recorded in the clinic are higher than at home [1], meaning that ‘usual’ BP is not always indicated by clinic-based readings. Twenty-four hour ambulatory BP monitoring (ABPM) is now the gold standard in BP measurement and is a valuable indicator of cardiovascular risk [2]. Indeed, ABPM, which provides a more reliable measure of ‘usual’ BP than clinic-based readings, has superior prognostic value compared with clinic BP [3] and is recommended by current guidelines as part of the routine assessment for diagnosing and managing hypertension [4,5,6]. However, ABPM can cause disruption to daily activities and relies on patient compliance. Thus, ABPM remains impractical for repeated or regular BP monitoring. Clearly, the ideal sphygmomanometer for recording BP routinely would combine the practicality of manual measurements with the prognostic value and lack of white coat effect associated with ambulatory readings.
Automated office BP (AOBP) is gaining recognition as an alternative way of measuring BP in the clinic. Sphygmomanometers that measure AOBP allow multiple BP readings to be recorded with the patient at rest and the operator absent from the examination room [7]. This is thought to minimise the white coat effect, and thus yield BP values that are closer to usual BP than observed office readings [8]. In addition, evidence suggests that AOBP is a good indicator of target organ damage, producing a similar correlation with left ventricular mass as ambulatory readings [9]. More recently, AOBP has been used in major hypertension trials such as the Systolic Blood Pressure Intervention Trial (SPRINT) [10], although recent data confirm that both attended and unattended BP readings were included in the analyses [11], and AOBP was recently included in the Canadian Hypertension Education Program guidelines as the preferred method of measuring in-office BP [5].
Several devices that can record AOBP have been validated for accuracy against mercury sphygmomanometry, including BpTru (BpTru Medical Devices, Coquitlam, BC, Canada) [12], Omron HEM-907 (Omron Healthcare, Kyoto, Japan) [13] and Microlife WatchBP (Microlife AG, Widnau, Switzerland) [14]. AOBP readings taken by both BpTru and Microlife WatchBP devices correlate well with ABPM [15, 16] and the Omron HEM-907 records similar BP readings to BpTru [17]. A recent sub-study from SPRINT compared ambulatory BP and clinic-based readings [18]. However, ambulatory and clinic readings may have been taken up to 3 weeks apart, and it is not clear whether the clinic readings were attended (observer present) or not. Therefore, the aim of our study was to evaluate the Omron HEM-907 device further, by comparing, directly, automated BP with observed office and ambulatory BP readings.
Methods
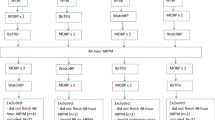
The study sample consisted of 108 participants who were recruited from hypertension clinics and a volunteer database held by the Vascular Research Clinic at Addenbrooke’s Hospital, Cambridge. Informed consent was given by all participants. Basic demographic data including age, sex, height, weight and current medications were recorded for each participant. After five minutes of seated rest in a quiet examination room, both OOBP and AOBP recordings were taken. The study operator was present during this period of rest. The order of OOBP and AOBP was randomised between participants, and there was no additional rest period between measurement modes. Following the office recordings, an ABPM was fitted to take daytime BP readings. Participants were followed up in the clinic exactly 1 week later, where OOBP and AOBP readings were repeated in the same order, after 5 minutes of seated rest.
Omron HEM-907 measurements
All office BP measurements were taken with the Omron HEM-907 device. Participants were seated comfortably and their non-dominant arm was used. Different cuff sizes were available, depending on arm circumference. For observed BP measurements, three single observed recordings separated by 1-minute intervals were made with the study operator present in the examination room. The first reading was discarded and the mean of the two remaining readings formed the OOBP. For automated measurements, three automated readings separated by two minute intervals were taken using the Omron HEM-907 device, whereas the study operator was out of the examination room. The average of these readings formed the AOBP.
Ambulatory monitoring
ABPM readings were recorded using the Mobil-O-Graph device (I.E.M., Stolberg, Germany) [19]. Six different Mobil-O-Graph devices were used, all of which were factory calibrated on a regular basis (at least once per year). The non-dominant arm was again used and different cuff sizes were available depending on arm circumference. The device was set to record BP at 30 min intervals during daytime hours and participants were instructed to wear the device for a minimum of 8 hours during the day and engage in routine daily activities. The mean AABP was then calculated.
Comparing Mobil-O-Graph and Omron HEM-907 devices
In order to compare, directly, the performance of the Omron HEM-907 and Mobil-O-Graph devices under standardised conditions, BP readings recorded by both devices were investigated in a further 30 volunteers. Age and sex were recorded for each participant. After 5 minutes of seated rest, BP was recorded in the non-dominant arm with both the Mobil-O-Graph and Omron HEM-907 devices, with the study operator present in the examination room. The same Mobil-O-Graph device was used for all recordings. The order in which the devices were used was randomised. Two recordings were made with each device and the average for each device was calculated.
Data analysis
Data were analysed using SPSS (Version 22) and are presented as means ± standard deviations. Paired-samples t tests were used for comparison of AOBP with both OOBP and AABP readings and Bland–Altman analyses were conducted to assess agreement between measurement modes [20]. Pearson correlation coefficients (r) were also calculated to examine continuous associations between AOBP, OOBP and AABP.
Results
Subject characteristics
Subject characteristics are presented in Table 1. There were 108 participants with an average age of 53 ± 21 years (range 20–85 years). Fifty-five participants (51%) were male and the average BMI was 26.7 ± 4.9 kg/m2. Fifty-six participants (52%) were hypertensive and 30 (28%) were taking antihypertensive medication. Two participants were lost to follow-up at the second visit. An average of 19 daytime ambulatory BP readings were recorded per participant.
Comparison of mean BP readings
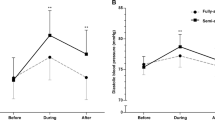
Average BP readings for each of the measurement modalities are shown in Table 2. On both visits AOBP was significantly lower than OOBP for both systolic BP (SBP) and diastolic BP (DBP), with a mean difference of −3 ± 7/−2 ± 4 mmHg for visit 1 and −4 ± 7/−3 ± 8 mmHg for visit 2 (P < 0.001 for all comparisons). AOBP was also significantly lower than AABP for both SBP and DBP, with a mean difference of −2 ± 11/−7 ± 10 mmHg (P = 0.02 and P < 0.001 for SBP and DBP, respectively). There was a high degree of correlation between AOBP and AABP (r = 0.75 and r = 0.64 for SBP and DBP, respectively, P < 0.001 for both) and between OOBP and AABP (r = − 0.66 for both SBP and DBP, P < 0.001 for both). There was no evidence of bias in the measurements modes as demonstrated by Bland–Altman plots for AOBP versus AABP (Fig. 1) and OOBP versus AABP (Fig. 2). Repeat readings for AOBP and OOBP were compared between visits 1 and 2. Mean differences were 1 ± 13/2 ± 8 mmHg for OOBP (P = 0.25 and P = 0.2 for SBP and DBP, respectively) and 2 ± 12/3 ± 10 mmHg for AOBP (P = 0.07 and P = 0.007 for SBP and DBP, respectively).
The influence of randomising the order of observed and automated BP readings is presented in Table 3. Irrespective of the order of measurements, AOBP was lower than OOBP for both SBP and DBP, although the differences were not statistically significant when OOBP was measured first. Similar results were obtained at the repeat visit (data not shown). In addition, averaging all three OOBP readings rather than the second and third readings did not meaningfully influence the results (average of three OOBP readings: 134 ± 18 and 77 ± 12 mmHg for SBP and DBP, visit 1; 132 ± 17 and 75 ± 12 mmHg for SBP and DBP, visit 2).
Comparing Mobil-O-Graph with Omron HEM-907
Mobil-O-Graph and Omron HEM-907 readings were compared under standardised conditions in the clinic, in 30 volunteers. The average age was 58 ± 20 years (range 25—86 years) and there were 21 females (70%). Average values for SBP and DBP are shown in Table 4. The Mobil-O-Graph device recorded significantly lower SBP values (mean difference − 4 ± 9 mmHg, P = 0.016) but significantly higher DBP values (mean difference of 6 ± 6 mmHg, P < 0.001) compared with the Omron device. However, both SBP and DBP readings were highly correlated between devices (r = 0.92 and r = 0.86, respectively, P < 0.001 for both).
Discussion
The current study aimed to compare automated BP measured using the Omron HEM-907 device with both observed office and ambulatory measurements. Our main findings were that automated BP was significantly lower than observed BP, and that automated BP was also significantly lower than ambulatory BP, albeit with a high correlation between measurement modalities. These data suggest that automated measurement of BP with the Omron HEM-907 is not associated with a white coat effect in the clinic setting and provides a suitable and convenient alternative for assessing usual BP.
White coat effect
In the current study, the same device (Omron HEM-907) was used to record BP in both automated and manual BP modes, and the absence of a white coat effect with automated measurements was consistent between study visits. This suggests that any differences were more likely to result from the measurement modality, i.e., the presence or absence of an operator in the examination room, rather than any inherent variability in the device itself, although the use of different measurement intervals for observed (one minute) and automated (two minutes) readings may have introduced additional variability. We deliberately randomised the order in which observed or automated readings were taken, so as to reduce the influence of any potential ‘order effect’. The lower SBP seen with automated versus observed measurements in our study was smaller in magnitude than that reported with the BpTru device [21]. However, all participants in the study using BpTru were known hypertensives and the average SBP on manual measurement was higher than in our study (151 ± 10mHg [21]). Moreover, the study utilising the BpTru device measured automated BP following the manual measurement, which may have resulted in an order effect [22]. Nevertheless, the reduction in manual office DBP with BpTru [21] was similar to the difference between observed and automated measurements seen in our study.
Automated versus ambulatory BP
We observed that automated BP was also significantly lower than daytime ambulatory BP, for both SBP and DBP, although this difference was small. Although this is in agreement with a previously published finding using the BpTru device [21], it has been suggested that allowing a period of rest prior to automated measurements, as done in the current study, may result in BP values, which are lower than ambulatory values [22]. Our randomisation procedure also meant that in half of the participants, automated measurements followed observed measurements and, therefore, an even longer rest period. However, as demonstrated in Table 3, the ‘order effect’ was much greater for observed measurements and so is unlikely to explain the overall lower automated versus ambulatory BP values obtained in our study. The study participants were relatively young, with an average age of 53 ± 21 years, and it is possible that greater activity levels during the daytime ambulatory monitoring period may have contributed to the higher BP values yielded by ambulatory, compared with automated BP monitoring.
The difference between automated and ambulatory BP readings in this study could also result from inherent differences between the measurement devices (Omron HEM-907 and Mobil-O-Graph). Indeed, a simple head-to-head comparison between the devices, under carefully standardised conditions, showed that the Mobil-O-Graph yielded lower values of SBP (by ~ 4 mmHg), but higher values of DBP (by ~ 6 mmHg). Assuming consistency and applying this offset to our observed AABP values would yield mean AABP values of 137/76 mmHg. The differences between devices could relate to several factors but most likely involves the measurement algorithm employed by each device. Our data are not supported by previously published studies with the Mobil-O-Graph, which demonstrate reasonable equivalence with the Spacelabs 90207 ambulatory BP monitor, particularly for DBP [23, 24]. However, previous studies [13, 25, 26] and a recent review [27] highlight a tendency for the Omron 907 device to record lower values of DBP. Regardless of the source of the discrepancy between devices, our data suggest that we may have under-estimated the true difference between automated and ambulatory readings in our study, at least for SBP, and support the notion [22] that a period of rest is probably not required prior to undertaking automated BP readings.
BP measurements from three different sphygmomanometers have now been compared against ambulatory BP [15, 16, 18], with our study being the first to compare readings between the Omron HEM-907 and ambulatory BP in a well-controlled setting, where both observed and automated readings were considered. In our study, automated BP measured with the Omron HEM-907 showed high correlations with ambulatory measurements for SBP and DBP, which compares favourably with results obtained with the Microlife WatchBP and BpTru devices (r = 0.819/0.801 [16] and r = 0.571/0.610[15], respectively). Although our sample size was considerably lower than the BpTru and SPRINT ABPM studies (n = 108 versus n = 481 and n = 897), it was similar to that used with Microlife WatchBP (n = 100). However, the ambulatory monitor used in each study has differed by manufacturer (A&D[15], Space Labs [16] and, in the current study, Mobil-O-Graph). For a more accurate comparison between the different measurement modalities, a single ambulatory device should be used. Ideally such a device would be able to measure BP in both ambulatory and automated modes so as to definitively test the hypothesis that automated and ambulatory measurement modes yield similar BP readings.
Limitations
Our study had a number of limitations. First, we included a relatively low number of hypertensive participants in comparison with other studies. However, we wanted to investigate the Omron HEM-907 device across a range of BP values, rather than just in the hypertensive range. In addition, the observed BP was the average of the second and third readings, with the first reading discarded, whereas automated BP was the average of all three readings. However, re-analysis of the data based on all three readings made no material difference to the results. Of note, observed readings were taken at 1-minute intervals, whereas automated readings were taken at 2-minute intervals, which may have introduced additional variability. Finally, we performed sequential readings of observed and automated BP during the same clinic visit, and allowed a rest period prior to the automated measurement. It has previously been suggested that allowing a rest period may result in automated BP values that are significantly lower than ambulatory values [22]. Therefore, we randomised the order of readings to reduce any potential order effects associated with sequential BP measurement. Performing automated or observed office BP readings in a randomised order before or after the ambulatory measurements would have provided an alternative approach.
Observed BP measurements in the clinic setting are subject to the white coat effect, yielding higher values than ambulatory readings, which are currently considered the gold standard for BP measurement. However, the utility of automated BP readings is becoming increasingly recognised. We have demonstrated that automated SBP and DBP readings measured with the Omron HEM-907 device were somewhat lower than observed BP measurements, an effect that was reproducible over two clinic visits. Moreover, automated BP readings correlated well with daytime ambulatory BP readings. Overall, our findings suggest that automated BP measured using the Omron HEM-907 provides a useful alternative to observed clinic measurements, which would likely be higher in routine office practice.
References
Kleinert HD, Harshfield GA, Pickering TG, Devereux RB, Sullivan PA, Marion RM, et al. What is the value of home blood pressure measurement in patients with mild hypertension? Hypertension. 1984;6:574–8.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–83.
Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–61.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219.
Leung AA, Nerenberg K, Daskalopoulou SS, McBrien K, Zarnke KB, Dasgupta K, et al. Hypertension Canada’s 2016 Canadian Hypertension Education Program Guidelines for Blood Pressure Measurement, Diagnosis, Assessment of Risk, Prevention, and Treatment of Hypertension. Can J Cardiol. 2016;32:569–88.
Hypertension in adults: diagnosis and management. Clinical Guideline CG127. 2011. Available from https://www.nice.org.uk/guidance/cg127.
Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension. 2010;55:195–200.
Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Conventional versus automated measurement of blood pressure in the office (CAMBO) trial. Fam Pract. 2012;29:376–82.
Andreadis EA, Agaliotis GD, Angelopoulos ET, Tsakanikas AP, Chaveles IA, Mousoulis GP. Automated office blood pressure and 24-h ambulatory measurements are equally associated with left ventricular mass index. Am J Hypertens. 2011;24:661–6.
Group SR, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Johnson KC, Whelton PK, Cushman WC, Cutler JA, Evans GW, Snyder JK, et al. Blood pressure measurement in SPRINT (Systolic Blood Pressure Intervention Trial). Hypertension. 2018;71:848–57.
Wright JM, Mattu GS, Perry TL Jr, Gelferc ME, Strange KD, Zorn A, et al. Validation of a new algorithm for the BPM-100 electronic oscillometric office blood pressure monitor. Blood Press Monit. 2001;6:161–5.
White WB, Anwar YA. Evaluation of the overall efficacy of the Omron office digital blood pressure HEM-907 monitor in adults. Blood Press Monit. 2001;6:107–10.
Stergiou GS, Tzamouranis D, Protogerou A, Nasothimiou E, Kapralos C. Validation of the Microlife Watch BP Office professional device for office blood pressure measurement according to the International protocol. Blood Press Monit. 2008;13:299–303.
Beckett L, Godwin M. The BpTRU automatic blood pressure monitor compared to 24 h ambulatory blood pressure monitoring in the assessment of blood pressure in patients with hypertension. BMC Cardiovasc Disord. 2005;5:18.
Myers MG, Valdivieso M. Evaluation of an automated sphygmomanometer for use in the office setting. Blood Press Monit. 2012;17:116–9.
Myers MG, Valdivieso M, Kiss A, Tobe SW. Comparison of two automated sphygmomanometers for use in the office setting. Blood Press Monit. 2009;14:45–7.
Drawz PE, Pajewski NM, Bates JT, Bello NA, Cushman WC, Dwyer JP, et al. Effect of intensive versus standard clinic-based hypertension management on ambulatory blood pressure: results from the SPRINT (Systolic Blood Pressure Intervention Trial) Ambulatory Blood Pressure Study. Hypertension. 2017;69:42–50.
Wei W, Tolle M, Zidek W, van der Giet M. Validation of the mobil-O-Graph: 24 h-blood pressure measurement device. Blood Press Monit. 2010;15:225–8.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Edwards C, Hiremath S, Gupta A, McCormick BB, Ruzicka M. BpTRUth: do automated blood pressure monitors outperform mercury? J Am Soc Hypertens. 2013;7:448–53.
Myers MG. Eliminating the human factor in office blood pressure measurement. J Clin Hypertens (Greenwich). 2014;16:83–6.
Kallem RR, Meyers KE, Sawinski DL, Townsend RR. A comparison of two ambulatory blood pressure monitors worn at the same time. J Clin Hypertens (Greenwich). 2013;15:321–5.
Sarafidis PA, Lazaridis AA, Imprialos KP, Georgianos PI, Avranas KA, Protogerou AD, et al. A comparison study of brachial blood pressure recorded with Spacelabs 90217A and Mobil-O-Graph NG devices under static and ambulatory conditions. J Hum Hypertens. 2016;30:742–9.
El Assaad MA, Topouchian JA, Darne BM, Asmar RG. Validation of the Omron HEM-907 device for blood pressure measurement. Blood Press Monit. 2002;7:237–41.
Omboni S, Riva I, Giglio A, Caldara G, Groppelli A, Parati G. Validation of the Omron M5-I, R5-I and HEM-907 automated blood pressure monitors in elderly individuals according to the International Protocol of the European Society of Hypertension. Blood Press Monit. 2007;12:233–42.
Myers MG. Automated Office Blood Pressure-Incorporating SPRINT Into Clinical Practice. Am J Hypertens. 2017;30:8–11.
Acknowledgements
This work was funded by the NIHR Cambridge Biomedical Research Centre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
D’Sa, L., Senaratne, N., Woodcock-Smith, J. et al. Evaluation of the Omron HEM-907 automated blood pressure device: comparison with office and ambulatory blood pressure readings. Hypertens Res 42, 52–58 (2019). https://doi.org/10.1038/s41440-018-0120-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0120-7
Key words
This article is cited by
-
Comparative accuracies of automated and manual office blood pressure measurements in a Chinese population
Hypertension Research (2022)
-
Comparison of blood pressure values—self-measured at home, measured at an unattended office, and measured at a conventional attended office
Hypertension Research (2019)
-
Automated Office-Based Blood Pressure Measurement: an Overview and Guidance for Implementation in Primary Care
Current Hypertension Reports (2019)