Abstract
Novel lipid-based carriers, composed of cationic derivatives of polyisoprenoid alcohols (amino-prenols, APrens) and 1,2-dioleoyl-sn-glycero-3-phosphatidylethanolamine (DOPE), were designed. The carriers, which were previously shown to be nontoxic to living organisms, were now tested if suitable for administration of candesartan, an antihypertensive drug. Spontaneously hypertensive rats (SHR) received injections of candesartan (0.1 mg/kg body weight per day; s.c.) in freshly prepared carriers for two weeks. The rats’ arterial pressure was measured by telemetry. Urine and blood collection were performed in metabolic cages. In a separate group of SHR, the pharmacokinetics of the new formulation was evaluated after a single subcutaneous injection. The antihypertensive activity of candesartan administered in DOPE dispersions containing APrens was distinctly greater than that of candesartan dispersions composed of DOPE only or administered in the classic solvent (sodium carbonate). The pharmacokinetic parameters clearly demonstrated that candesartan in APren carriers reached the bloodstream more rapidly and in much greater concentration (almost throughout the whole observation) than the same drug administered in dispersions of DOPE only or in solvent. Serum creatinine (PCr) decreased significantly only in the group receiving candesartan in carriers with APrens (from 0.80 ± 0.04 to 0.66 ± 0.09 mg/dl; p < 0.05), whereas in the other groups PCr remained at the same level after treatment. Moreover, the new derivatives increased the loading capacity of the carriers, which is a valuable feature for any drug delivery system. Taken together, our findings led us to conclude that APrens are potentially valuable components of lipid-based drug carriers.
Similar content being viewed by others
Introduction
The term “polyisoprenoid alcohols” describes numerous naturally occurring hydrophobic polymers found in almost all living organisms [1]. These linear compounds are constructed of 5 to >150 isoprene units with a hydroxyl group (–OH) on the α-terminus and a hydrogen atom on ω-terminus [2]. Polyisoprenoid alcohols are commonly divided into dolichols (with a hydrogenated α-bond) and α-unsaturated polyprenols. The biological role of polyisoprenoid alcohols is a subject of extensive study, and they are postulated to serve as structural components that modulate the properties of cellular membranes [2]. Biophysical studies have shown that polyisoprenoids act as membrane modulators by increasing their fluidity and permeability [3, 4].
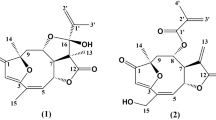
The latest research has demonstrated that semi-synthetic, cationic derivatives of polyisoprenoid alcohols (called amino-prenols, or APrens) possess lipofecting properties because they facilitate the transfer of genetic material into the cells [5]. To generate this cationic polyisoprenoid derivatives, we replaced the hydroxyl group on the α-terminus of polyisoprenoid alcohols with a quaternary ammonium group. This generated specific properties whereby these cationic lipids can influence biological membranes more easily and effectively, which gave rise to the idea of using APrens as components of lipid drug carriers.
The adverse effects of many currently used drugs, necessity to apply a combination of various drugs, and their insufficient bioavailability constitute major medical problems that physicians and patients are forced to address [6,7,8]. The pharmacological properties of common drugs can be augmented by using drug delivery systems (DDSs). Providing faster target access, delaying the rapid metabolism of the drug and/or slowing excretion through the kidneys can lead to a decrease in the therapeutic dose needed; thereby, adverse effects can be minimized or even eliminated [7].
Novel carriers composed of APrens and 1,2-dioleoyl-glycero-3-phosphatidyl ethanolamine (DOPE) were designed and proved not to be toxic for living organisms [9, 10]. The primary objective of this study was to evaluate the properties of APrens as components of drug carriers. As a model drug, we have chosen candesartan, an antihypertensive drug. Candesartan is a lipophilic drug belonging to the sartan family, which includes a large group of antagonists of the angiotensin II (ANG II) AT1 receptor. Candesartan is usually administered orally as a prodrug, candesartan cilexetil [11]. Candesartan cilexetil is absorbed in the intestinal wall and completely metabolized by esterases to the active form of candesartan. It shows relatively low bioavailability (~40%) after oral administration due to incomplete absorption [11]. We wanted to examine the hypotensive effectiveness of candesartan encapsulated in newly designed lipid-based carriers composed of APrens after subcutaneous administration to spontaneously hypertensive rats (SHR). In addition, we wanted to investigate whether changing the route of administration (from oral to subcutaneous) would improve its antihypertensive effectiveness and whether the required potency could be achieved with small doses of the drug.
Changes in arterial pressure were evaluated by telemetry in conscious, unrestrained rats. Once a week, rats were observed in metabolic cages and blood sampling was performed. Pharmacokinetic parameters were evaluated in a separate group of rats after a single subcutaneous injection.
Methods
Preparation of heptaprenyltrimethylammonium iodide (APren-7)
An amino-prenol containing seven isoprene units (APren-7) was selected for this study. First, a corresponding polyisoprenoid alcohol was extracted from birch wood, and then it was chemically modified following a procedure described previously [5]. A stock solution of APren-7 in ethanol was stored at −20 °C until used.
Preparation of aqueous dispersions of lipids for injection
Lipid suspensions were prepared using a lipid film hydration protocol. Briefly, to obtain candesartan-containing dispersions composed of DOPE and APren-7 (C+LP), we mixed 50 µl of a solution of DOPE (Sigma-Aldrich, Poznan, Poland) in chloroform (90 mg/ml) with 25 µl of a solution of APren-7 in ethanol (9 mg/ml, molar ratio DOPE:APren-7 = 10:1) and 50 µl of a solution of candesartan in ethanol (1 mg/ml; Santa Cruz Biotechnology, Santa Cruz, USA). This solution was dried with a stream of nitrogen gas to form a thin film on the bottom of the glass tube and further dried under reduced pressure overnight. Then 450 µl of water (82 °C) was added to hydrate the film. The tube was vortexed for 2 min and heated in a water bath (82 °C) for 10 min; this cycle was repeated twice, after which the tube was vortexed for 6 min. The suspension formed was extruded seven times through a 100 nm polycarbonate membrane (LiposoFast extruder, Avestin Europe GmbH, Mannheim, Germany). An appropriate volume of freshly prepared lipid suspension, containing an adequate amount of candesartan (see below), was used for each animal.
Control suspensions containing candesartan in aqueous dispersions with DOPE only (C+L) were prepared using 55 µl of a solution of DOPE in chloroform (99 mg/ml) and 50 µl of a solution of candesartan in ethanol (1 mg/ml), and the rest of the preparation was conducted, as described above.
To ensure that each rat received the correct dose of candesartan (0.1 mg/kg), we verified the amount of the drug in the prepared lipid suspensions each time with HPLC/UV using a previously described method [12] with modifications (4.6 × 250 mm2 Cosmosil 5C18-AR-II (0.5 μm) column; isocratic elution with methanol, pH 6.5; external standards were used). Experiments were performed using a Waters dual-pump apparatus and a Waters Photodiode Array Detector (spectrum range: 200–440 nm).
Solution of candesartan in solvent and control solution
A solution of candesartan (0.03 mg/ml) in 0.1 N sodium carbonate (Na2CO3) and phosphate-buffered saline (PBS) mixed at a ratio of 1:24 was prepared (C+S); solvent alone (S) was administered (0.1 N Na2CO3 and PBS mixed at a ratio of 1:24) as a control.
Experimental animals
The experimental procedures were approved by the IV Ethical Committee (Warsaw). Male spontaneously hypertensive rats (SHR) bred at the Animal House of Mossakowski Medical Research Centre, Polish Academy of Sciences, weighing 301 ± 3 g (age: 11–13 weeks; n = 32) at the start of the experiments, were fed ad libitum a standard diet (STD, 0.25% Na w/w, SSNIFF GmbH, Soest, Germany) and had free access to drinking water during the whole experiment. An additional group of SHR (weighing 295 ± 6 g, age 11–13 weeks; n = 9) were used in the pharmacokinetic study.
Experimental protocols and measurements
A week before the beginning of the proper experiment telemetry transmitters (Data Sciences International, St. Paul, USA) were implanted into each rat for blood pressure measurements. The procedure was conducted under short-term anesthesia (pentobarbital sodium salt; 50 mg/kg i.p.). After 7 days of recovery, the rats were randomly divided into four groups and received (daily for two weeks) subcutaneous injections of freshly prepared solutions of candesartan (0.1 mg/kg in volume of 1 ml) in three different carriers – C+LP (candesartan in dispersions made of DOPE and APren-7), C+L (candesartan in dispersions made of DOPE only), or C+S (candesartan in solvent) – or a control solution, S (solvent) (n = 8 for each group). To eliminate the impact of circadian rhythms on blood pressure changes [13], we always performed the injections at the same time of day, between 1100 hours and 1200 hours.
Chronic experiment
Twice a week, systolic blood pressure (SBP) was measured by telemetry for 5 h after the injection. At one-week intervals (days 0, 7, and 14), rats were placed in metabolic cages (Tecniplast S.p.A., Buguggiate, Italy) for 24 h to measure food and water intake, urine volume, and the weight of feces. The osmolality (Uosm) and the concentrations of sodium (UNa), potassium (UK), and albumin in the urine were measured to calculate the excretion rates. Also on days 0, 7, and 14, blood was sampled for measurement of plasma osmolality (Posm), plasma sodium (PNa), and plasma creatinine concentration (PCr). Body weight (BW) was also determined.
Acute experiment
After 2 weeks, a subset of the rats in each group were killed, and the organs were collected for histopathological and morphometric analysis. The kidneys were weighed and fixed with 4% PFA. Heart weight was also measured, after which the left ventricle was gently excised and weighed for left ventricle hypertrophy assessment.
The second subset of rats were anaesthetized with intraperitoneal sodium thiopental (100 mg/kg; Sandoz GmbH, Kundl, Austria), and after surgical preparations, cardiovascular, and renal function parameters were assessed in acute experiments. All the surgical procedures were performed, as previously described [9, 14, 15]. Briefly, a cannula was placed in the trachea to provide clear airways, and the rats’ body temperature was maintained at approximately 37 °C using a servo-controlled heating pad. For blood sampling and mean blood pressure (MBP) measurements, a catheter was placed in the femoral artery and connected to a Statham pressure transducer; the same catheter was also used for sampling aortic blood. The left kidney was exposed from a subcostal flank incision and placed in a plastic holder. For total renal blood flow (RBF) measurement, a cuff probe was placed on the renal artery, connected to a Transonic flowmeter (Type T106, Transonic System, Inc., Ithaca, USA). The blood perfusion of the renal cortex (CBF) and outer and inner medulla (OMBF, IMBF) were measured separately as laser-Doppler fluxes using a Periflux 4001 system (Perimed AB, Jarfalla, Sweden). For CBF, a PF 407 probe was placed on the kidney surface; for OMBF and IMBF, two needle probes (PF 402) were inserted into the kidney to depths of 3 and 5 mm, respectively. For timed urine collection, the ureter was cannulated. To compensate fluid losses, bovine albumin (3% in Ringer solution) was infused at 10 ml/kg/h via the femoral vein. After the surgical preparations, inulin (1.5% solution in saline; 10 ml/kg/h; inulin from dahlia tubers, Sigma-Aldrich, Poznan, Poland) was administered throughout the whole experiment to measure glomerular filtration rate (GFR).
Pharmacokinetic study
A separate group of animals was used to evaluate the pharmacokinetics of candesartan in novel carriers with APrens after a single subcutaneous injection. A few days before the actual experiment, rats were anesthetized (pentobarbital sodium, 50 mg/kg, Biowet, Pulawy, Poland) and the coronary artery was cannulated for blood sampling (Micro-Renathane MRE033, BIOSEB-In Vivo Research Instruments, USA/Canada). The catheters were filled with an anticoagulant solution of 4% Citra-LockTM (Dirinco AG, Bern, Switzerland), and the rats were injected with an analgesic (Metacam, subcutaneous, 0.4 mg/kg). After recovery, the rats received a single, subcutaneous injection of a freshly prepared solution of candesartan (0.1 mg/kg in a volume of 1 ml) in a dispersion made of DOPE and APren-7 (C + LP, n = 3), candesartan in a dispersion made of DOPE only (C+L, n = 3) or candesartan in solvent (C+S, n = 3). Arterial blood (300 µl) was collected through a heparinized syringe before each injection (blank sample for baseline value) and then at hourly intervals for 8 h. The blood samples were immediately centrifuged at 2800 × g for 10 min. The plasma (~150 µl) was removed and stored at −20 °C until analysis was performed.
Analytical procedures
The freezing point depression method (Osmomat® 030 M, Gonotec, Berlin, Germany) was used to measure plasma and urine osmolality. Sodium and potassium concentrations were determined by flame photometry (PFP7/C, Jenway Ltd, Stone, UK). The gravimetric method was used for urine volume measurement. Commercially available ELISA kits were used to assess urinary albumin (Immunology Consultants Laboratory, Inc., Portland, USA) and plasma creatinine (Sunred Biological Technology, Shanghai, China) concentrations.
Glomerular filtration rate (GFR)
GFR was calculated on the basis of inulin clearance. Plasma and urine inulin levels were determined using a modified method described previously [16]. Samples (100 µl aliquots) of plasma (diluted 1:3 with PBS) and urine (diluted 1:100 with PBS) were added to glass tubes, followed by the addition of 100 µl of a solution of glucose oxidase (100 U/ml; Sigma-Aldrich, Poznan, Poland) and catalase (1000 U/ml; Sigma-Aldrich, Poznan, Poland) prepared in pH 7 buffer. The tubes were briefly vortexed and incubated for 1 h at 37 °C in a laboratory incubator. Then, 150 µl of 50 mM indole-3-acetic acid (Sigma-Aldrich, Poznan, Poland) and 3 ml of hydrochloric acid (12.1 N) were added to each glass tube and incubated in a water bath for 20 min at 60 °C. After the samples were allowed to cool at room temperature for 30 min, an aliquot (200 µl) of each sample was transferred to a 96-well microplate and read spectrophotometrically at 490 nm (FLUOstar Omega, BMG LABTECH GmbH, Ortenberg, Germany). A linear calibration curve was constructed for each microplate using seven standard concentrations (0.0625 to 2 mg/ml) of inulin in PBS.
Renal morphology
Paraffin-embedded renal slices were stained with hematoxylin-eosin for histopathological analysis. The degree of damage to fifty randomly selected glomeruli per section was assessed under a light microscope. A semi-quantitative scoring method was used: grade 0—normal glomeruli; grade 1—sclerotic area up to 25%; grade 2—sclerotic area 25 to 50%; grade 3—sclerotic area 50 to 75%; grade 4—sclerotic area 75 to 100%. The glomerulosclerosis index (GSI) was calculated using the following formula:
where nx is the number of glomeruli in each grade of glomerulosclerosis [17].
To compare the tissue loss between groups, we carefully evaluated each renal slice in a two-step analysis. Renal slices that macroscopically exhibited the most extensive tissue loss were marked as “Significant tissue loss”. Afterwards, each renal slice was assessed under a microscope and marked as either “Lack of changes” or “Minor changes”. Investigators were blinded to the group assignments for the duration of macroscopic and microscopic analysis to promote the objectivity of the assessment.
Concentration of candesartan in plasma
Plasma samples collected in the pharmacokinetic study were used to measure candesartan concentration by high-performance liquid chromatography-electrospray ionization mass spectrometry (LC-MS). An LC-MS system (Shimadzu, Kyoto, Japan) consisting of a Jupiter 4 µm Proteo 90 Å column (250 × 4.6 mm2, 4 µm; Phenomenex, Torrance, USA), a binary Prominence pump (LC-20AD), an auto-sampler (SIL-20ACHT), a solvent degasser (DGU-20A3R), a column oven (CTO-20AC), a UV-Vis detector (SPD-20A), a controller (CBM-20A), and a liquid chromatograph mass spectrometer (LCMS-2020) was used for the study. The following HPLC- and LC-MS-grade solvents were used: acetonitrile (ACN), formic acid (FA), methanol (all from Sigma-Aldrich, Poznan, Poland), and deionized water from a Simplicity water purification system (MERCK, Poland).
Sample preparation
An aliquot of 150 µl of each plasma sample was added to 300 µl of ACN containing 1% of FA for protein precipitation. Then, the samples were vortexed and centrifuged (2800 × g, 4 min). The supernatants were collected, and another 200 µl of ACN with 1% of FA was added; the samples were then vortexed and centrifuged again. The combined supernatant was loaded into a HybridSPE-Phospholipid Ultra cartridge (Sigma-Aldrich, Poznan, Poland) in order to remove phospholipids and debris from the samples. A vacuum was applied, and the collected filtrate (450 µl) was evaporated under a nitrogen stream with SPE 24 position vacuum manifold system (Phenomenex, Torrance, USA) until dry, then reconstituted in 70 µl of methanol. Next, the samples were injected (10 µl) into the LC-MS system.
Chromatographic conditions
The mobile phases were as follows: A, deionized water with 0.05% FA; B, methanol with 0.05% FA. The total flow rate was set at 1.2 ml/min. A linear gradient from 30% to 100% of B over 20 min (the total length of one analysis was 45 min) was applied. Analysis was performed at 35 °C. The mass spectrometry data were analyzed using selected ion monitoring (SIM) mode in mass spectrometry.
Data analysis
A semi-quantitative method was used to estimate the concentration of candesartan in each sample. Blank rat plasma was spiked with a known amount of candesartan (0.75 µg) and processed along with all other samples. The area under the peak for the spiked plasma was used as a standard to calculate the concentration of the drug. Standard non-compartmental methods were used to evaluate the pharmacokinetic parameters. The peak serum concentration (Cmax) and the time to reach it (Tmax) were evaluated by visual examination of the data.
Statistics
Data are presented as the means ± SEM. The significance of changes was evaluated by repeated-measures multivariate analysis of variance (ANOVA), followed by a post hoc Duncan’s multiple range test (STATISTICA, version 10.0, StatSoft, Inc.). For some measured parameters, one-way ANOVA was used. The level of statistical significance was set at p < 0.05.
Results
Capacity and stability of aqueous DOPE dispersions
The amount of candesartan in 25 µl of lipid suspension for C+LP was 1.58 ± 0.06 µg, whereas the amount for the C+L group was 0.58 ± 0.08 µg (n = 11; p < 0.05 C+LP vs C+L, one-way ANOVA, followed by a post hoc Duncan’s multiple range test). The threefold increase in the ratio of candesartan to lipid components for C+LP indicates that APren-7 significantly improved the loading capacity of the designed carriers.
Moreover, the amount of candesartan measured (only in a few samples) after two weeks of storage at +4 °C was not changed in dispersions composed of DOPE and APren-7 (C+LP), while it was slightly decreased (by 15%) in control dispersions composed of DOPE only (C+L). The formation of precipitate occurred only in the C+L group, which might suggest that APrens prevented this phenomenon.
Animal studies
Systolic blood pressure (SBP; Fig. 1)
For all groups receiving candesartan (C+LP, C+L, C+S), a statistically significant reduction in SBP was observed in comparison to a baseline value obtained on day 0 (for each group) and to a control group (SBP decrease after two weeks of treatment for C+LP: from 143 ± 4 to 110 ± 5; C+L: from 148 ± 4 to 126 ± 4; C+S: from 141 ± 6 to 117 ± 5; S: from 160 ± 3 to 154 ± 5 mmHg). Figure 1a shows the magnitude of SBP reduction (ΔSBP), assessed as the difference between SBP value on the following days and the baseline value on day 0 (the statistical significance of the within-group differences from day 0 has been omitted for clarity). After three days of treatment, ∆SBP was significantly lower in all candesartan-receiving groups than in the control (S) group (Fig. 1a). A greater decrease in SBP caused by candesartan administered in newly designed carriers with APren-7 (C+LP) was observed on day 6 of the experiment (NS). For this group, a progressive decrease in SBP until the end of the experiment was recorded, whereas, in the other groups receiving candesartan (C+L and C+S), ΔSBP remained stable or was even lower. At the end of the treatment, a significantly greater ΔSBP was observed in the C+LP group than in C+L or C+ S (Fig. 1a, b). Moreover, no ΔSBP difference was seen between the C+L and C+S groups.
a Decrease in systolic blood pressure (ΔSBP); b ΔSBP measured on the 13th day in spontaneously hypertensive rats (SHR) receiving for two weeks daily subcutaneous injections of the following, freshly prepared solutions: C+LP – candesartan in dispersions made of DOPE and APren-7 (0.1 mg/kg); C+L – candesartan in dispersions made of DOPE only (0.1 mg/kg;); C + S – candesartan in solvent (0.1 mg/kg); S – solvent (n = 8 for each group); * significantly different for C+LP compared with C+L, C+S and S; # significantly different for S compared with C+LP, C+L, C+S, p < 0.05 (repeated-measures multivariate analysis of variance [ANOVA], followed by a post hoc Duncan’s multiple range test)
Changes in body weight, excretory and plasma parameters (Table 1 and Table 2)
As expected, some parameters such as BW and diuresis increased significantly with age in each group (Table 1). Additionally, an increasing tendency was observed in parameters such as food and water intake (NS except in the S group, Table 1). After two weeks, diuresis was distinctly greater in the S group than in the C+L group or the C+S group, and the water intake in S group was significantly higher than in C+LP.
Table 2 shows the two-week profiles of total solute (UosmV), sodium (UNaV), potassium (UKV), and urinary albumin (UAE) excretion and of plasma osmolality (Posm), sodium (PNa), and potassium (PK) concentration. UosmV increased significantly in all groups except C+L (only a trend-level tendency was observed in this group). Sodium excretion increased in the S group. The baseline UAE value was significantly higher in C+S than in the C+L group or the control group (S). After two weeks, UAE in the C+S group significantly decreased, and UAE was similar in all groups. Over two weeks, plasma sodium concentrations decreased in the C+LP group.
Plasma creatinine (PCr, Fig. 2)
Figure 2 depicts changes in plasma creatinine over the course of two weeks. In the group receiving candesartan in the new carriers with APren-7 (C+LP), plasma creatinine decreased progressively (statistically significant after 14 days). At the end of the experiment, PCr was significantly lower in this group than in the C+S or S group and close to the set level of statistical significance in comparison to C+L group (p = 0.07).
Creatinine concentration in plasma (PCr) measured on days 0, 7, and 14 in SHR receiving for two weeks daily subcutaneous injections of freshly prepared solutions: C + LP, C + L, C + S and S (denotations as in Fig. 1; n = 8 for each group); *significantly different for C + LP compared with the value obtained on day 0; # significantly different for C + LP compared with C + S and S on the corresponding day of treatment, p < 0.05 (repeated-measures multivariate analysis of variance [ANOVA], followed by a post hoc Duncan’s multiple range test)
Renal and cardiovascular function parameters measured in acute experiments (Table 3)
The parameters measured in the acute experiments are shown in Table 3. The lowest MBP was observed in the C + LP group, but there were no significant differences between groups, probably owing to the small size of the groups (only a portion of each group was subjected to the acute experiment). Other parameters were consistent with the physiological values for SHR and did not differ between groups.
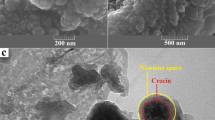
Histopathology, morphology and morphometry (Fig. 3)
Morphological analysis of renal slices stained with hematoxylin-eosin revealed significant histopathological changes. In some kidneys, the usual three-zoned structure (cortex, outer medulla, and inner medulla) was not seen, and significant tissue atrophy was observed. This might suggest a progressive tubulointerstitial inflammatory process leading to nephrosclerosis, which is common in SHR [18]. Macroscopic images of all analyzed kidneys are depicted in Fig. 3a. (Fig. 3 in color and enlarged color images of selected slices from each group are available in Supplementary Figures S1 and S3). Microscopic and macroscopic analysis revealed that the proportion of kidney tissue loss was lowest in the C+LP group, which received candesartan in novel carriers with APren-7, but the difference did not show statistical significance. Overall, five out of eight kidneys (62.5%) harvested from the C+LP group did not exhibit any damage. In the other groups, renal nephrosclerosis seemed more pronounced, but statistical analysis did not confirm the significance of this difference, probably owing to the small size of the groups. The observations are summarized in detail in Fig. 3.b. In the kidneys in which pathological changes had apparently not yet developed or within the remaining intact tissue areas, morphologic features typical of SHR were observed, especially in the cortex (data available in Supplementary Information, Figure S2). In addition, the glomerulosclerotic index (GSI) did not differ between groups (C+LP: 0.26 ± 0.03; C+L: 0.38 ± 0.06; C+S: 0.27 ± 0.05; S: 0.32 ± 0.05 arb. unit; NS). Morphometric analysis did not reveal any significant differences between groups (data available in Supplementary Table S1).
a Macroscopic images of renal slices stained with hematoxylin-eosin and b distribution of the kidneys (number of kidneys in each group) by extent of renal damage, harvested from SHR receiving for two weeks daily subcutaneous injections of freshly prepared solutions: C+LP, C+L, C+S and S (denotations as in Fig. 1)
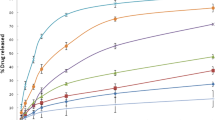
Pharmacokinetic study (Fig. 4)
The plasma concentration of candesartan after single subcutaneous injection into SHR is depicted in Fig. 4. The Cmax for the drug administered in lipid carriers with APren-7 (C+LP: 0.26 ± 0.05 ng/ml) was reached at 3 h (Tmax) after the injection. After 2 h of injection, the drug concentration was significantly higher in this group than in groups that received candesartan in other carriers (C+L and C+S), and this lasted almost until the end of the experiment. The peak concentration after administration of candesartan in dispersions made of DOPE only (C+L) was also reached after 3 h (Cmax for C+L: 0.13 ± 0.03 ng/ml), and the concentration curve was similar in shape to that of C+LP, but the values were much lower. In the C+S group, it was difficult to evaluate the peak concentration by visual examination of the data and to identify the Tmax. The drug concentration in the C+S group remained stable throughout nearly the whole experiment, ranging between 0.10 ± 0.02 and 0.11 ± 0.03 ng/ml, and reached a minimum at the end (0.08 ± 0.03 ng/ml).
The concentration of candesartan in plasma after single subcutaneous injection into SHR of freshly prepared solution: C+LP, C+L or C+S (0.11 m mg/kg, n = 3 for each group denotations as in Fig. 1); *significantly different for C + LP compared with C+L; # significantly different for C + LP compared with C+S; p < 0.05 (repeated-measures multivariate analysis of variance [ANOVA], followed by a post hoc Duncan’s multiple range test)
Discussion
We have tested novel carriers containing a cationic, semi-synthetic derivative of polyisoprenoid alcohol (APren-7) for subcutaneous administration of candesartan in SHR. Dispersions containing DOPE and APren-7 (C+LP) exhibited a significantly elevated loading capacity for candesartan in comparison to control carriers devoid of APren (C+L), which is a valuable property for any DDS. In addition, it seems that APren-7 prevents the leakage of the drug from the carriers. APren carriers containing candesartan have not yet been characterized in detail; however, the hydrophobic nature of the molecules of the drug suggests its incorporation into, or at least close association with, the lipid layer, where APren molecules are incorporated as well. The positive charge of the APren molecule might affect the APren-candesartan interactions and consequently influence the rate at which the drug is released from the carrier. This interaction is probably due to the formation of an electrostatic bond between the quaternary ammonium group of APren and the carboxylic group of candesartan, which should be dissociated and thus negatively charged under the applied experimental conditions (pH of ~6.5). This electrostatic interaction might lead to the formation of APren-candesartan clusters in the lipid layer, and this, in turn, would facilitate loading of the drug. Such electrostatic interactions do not occur in the lipid layer in the absence of APren. This speculation is validated by the increased content of candesartan recorded in dispersions supplemented with APren in comparison to the control (DOPE only).
On the other hand, the presence of the positively charged APrens in the lipid membrane should facilitate its interaction with the negatively charged phospholipids of the endothelial membrane system, followed by fusion of the membranes and release of the drug. Although tempting, these speculations require further experimental verification.
The antihypertensive effectiveness of candesartan given in the novel carriers was compared with the effectiveness of candesartan administered in control carriers made of DOPE only and in the solvent. Analysis of the magnitude of reduction of SBP indicated that the newly designed carriers with APrens augmented the therapeutic efficacy of candesartan. In the C+LP group, a progressive decline in SBP was observed until the end of the experiment, whereas in the groups receiving candesartan in control dispersions or in solvent, SBP remained unaltered or started to rise again after 6 days of treatment. Notably, in acute experiments, the lowest MBP was recorded for the C+LP group. These results suggest that APren-7 used as a component of the lipid drug carriers improved the bioavailability of candesartan. We performed additional experiments to evaluate the pharmacokinetics of the drug in the new formulation (after a single subcutaneous injection). The results clearly show that candesartan reaches the bloodstream more rapidly and in much greater concentration when administered in novel lipid carriers with APren-7. This derivative, owing to its ability to interact with biological membranes, can probably facilitate the penetration of the subcutaneous tissue and accelerate the entrance of the drug into the bloodstream, shortening the time it takes to reach the AT1 receptors. It seems that this facilitation is due to the modification of the physicochemical properties of dispersions by APren-7 per se, as the bioavailability of candesartan given in dispersions of DOPE only was much lower and close to the value for solvent alone.
Moreover, the antihypertensive efficacy of candesartan depends on the applied dosage [19]; therefore, we would like to emphasize that a significant and substantial decrease in blood pressure was achieved with a low dosage of the drug (0.1 mg/kg/day). When administered orally in the form of a prodrug (candesartan cilexetil), it is usually given in much higher doses [20, 21]. Skov et al [22]. administered candesartan cilexetil to SHR (in drinking water) at three different dosages, and only the highest (5 mg/kg/day), which was 50 times higher than the one used in our study, resulted in substantial inhibition of the development of hypertension. We are aware that the direct comparison of the effectiveness of drugs administered by different routes is not completely justified at this point, but the results we obtained are also promising in comparison to previous reports on subcutaneously administered candesartan. Nishimura et al. [23, 24]. treated SHR with candesartan at a 5-fold higher dosage (0.5 mg/kg/day dissolved in 0.1 N sodium carbonate via subcutaneously implanted mini-pumps, for 14 days) and observed only a slightly stronger antihypertensive effect than the one presented in the present work (Nishimura et al. found a 32% decrease in BP, whereas we observed a 23% decrease in SBP for the C+LP group). Moreover, the baseline values of BP in Nishimura’s work were much higher; therefore, the normalization of blood pressure was within the same range of values.
The higher effectiveness of candesartan in the novel carriers is also supported by analysis of plasma creatinine (PCr), which is a routinely used marker for assessment of renal function [25, 26]. Specifically in the group that received candesartan in dispersions with APren-7, a progressive decrease in PCr was observed, which may indicate improvement of renal function as a result of the reduction in SBP. This might also suggest some renoprotective activity of APrens per se, since a progressive decrease in PCr occurred in the C+LP group only. This observation may be significant, considering the numerous reports indicating that other derivatives of polyisoprenoid alcohols exhibit similar properties. It has been demonstrated that polyisoprenoid epoxides stimulate the biosynthesis of coenzyme Q and inhibit cholesterol synthesis [27]. In addition, dolichols are suspected of being involved in the response to oxidative stress and in aging [28]. Obviously, we cannot draw explicit conclusions regarding the renoprotective properties of the APrens solely on the basis of a decrease in PCr. Nevertheless, this finding is definitely worthy of further exploration.
Another parameter measured in this study was urinary albumin excretion (UAE), which, in 2009, was added by the European Medicines Agency in cooperation with the Food and Drug Administration (EMEA/FDA) to the list of biomarkers for nephrotoxicity detection in preclinical drug studies [29, 30]. UAE did not show any significant changes after treatment with candesartan in the C+LP group. In the C+S group, a significant decrease in UAE was observed after treatment, but we are reluctant to ascribe it to greater hypotensive effectiveness. The significant decrease observed might be explained by the significantly higher baseline value of UAE, which may be due to the high interindividual variability of the SHR strain. After treatment, UAE values were at the same relatively low level in all groups; much higher values of UAE are considered a symptom of albuminuria in SHR [31].
The SHR strain is now considered the best model imitating the development of kidney disease in patients with hypertension [32, 33]. It has been shown that SHR exhibit elevated UAE due to the development of hypertension and kidney injury [34]. The reason for the absence of any influence of 2 weeks’ treatment on UAE in our study was probably the fact that the rats were just entering the established phase of hypertension; hence, progressing kidney damage was not yet reflected by increased excretion of albumin [18, 35]. However, histopathological analysis did reveal damage that had not yet manifested itself as increasing UAE. In some kidneys harvested from the animals at the end of the experiment, major structural changes were observed. Extensive nephrosclerosis is a common phenomenon occurring in SHR [36,37,38]. It has been demonstrated that the glomerular afferent arterioles of SHR are constricted, which can directly cause tissue ischemia and interstitial infiltration of cells involved in the inflammatory response, such as T-lymphocytes and macrophages. These cells can locally generate ANG II and reactive oxygen species, which can lead to tubulointerstitial nephritis [38]. On the basis of the histopathological analysis, which showed that the structural changes were least pronounced in the C+LP group, we can assume that pathological inflammation leading to extensive tissue loss was alleviated to the greatest extent in rats receiving candesartan administered in novel carriers with APren-7.
Evaluation of the vast majority of other parameters measured showed no significant differences between or within groups receiving candesartan or between them and the control group (S). We observed some within-group differences in certain parameters (diuresis, water intake, total solutes and sodium excretion). The abovementioned increments are due to the normal physiological growth of the animals. We also believe that some of the observed differences between groups (in water intake and diuresis) are a consequence of rather unfortunate randomization of the animals at the beginning of the experiment, which led to a slightly higher BW for animals in the control group. In this group, most of the values are somewhat higher than those in other groups. The majority of the significant between-group differences in those parameters are obliterated when expressed per 100 g body weight (data not shown). Also debatable is the decrease in plasma sodium concentration in the C+LP group. Again, probably owing to the substantial inter-individual variability of the SHR strain, the baseline value of PNa was slightly higher in this group than in other groups, but after two weeks there were no differences between groups; therefore, we believe that it is not related to the effectiveness of the administered therapy.
Conclusions and clinical implications
The experiments described herein are the first evaluation of novel derivatives of polyisoprenoid alcohols as components of drug carriers. In summary, candesartan, the drug selected for this study, showed greater antihypertensive activity when given in dispersions with APrens than when administered in control lipids without APren or in the classic solvent. Pharmacokinetic experiments confirmed that this functional improvement was a result of increased bioavailability of the drug caused by APren per se.
Further studies are necessary to confirm the properties of APrens and their potential use for the delivery of drugs targeting intracellular receptors. Nevertheless, we conclude that APrens may serve as a valuable component of lipid-based carriers for the delivery of drugs. Furthermore, APrens increased the loading capacity and probably improved the physicochemical parameters of new carriers, which is valuable for any drug delivery system. Also worth mentioning are obtained prerequisites that APrens per se exhibit renoprotective properties. Further research is necessary to test this hypothesis; nevertheless, considering other reports regarding similar properties, we take the position that this finding definitely merits further investigation.
In our opinion, the significant and substantial decrease in systolic blood pressure after subcutaneous administration of candesartan (in relatively small dosage and after only three days of treatment) calls for special attention.
We are aware that while oral drug administration is at present the most convenient route, the development of patch technology for transdermal drug delivery is very promising. The advantage over traditional routes is that it can ensure a stable drug concentration in the blood, owing to the constant rate of drug release from the patch [39]. Moreover, the common and serious problem of patients’ poor compliance with the dosing schedule is eliminated [40]. Furthermore, oral administration is often not possible owing to gastrointestinal disorders (persistent diarrhea or vomiting), impaired consciousness or swallowing problems. Importantly, by circumventing the gastrointestinal system, we eliminate the problem of incomplete absorption, as well as the first pass effect through the liver. Thus, the bioavailability of the drug increases. Subcutaneous or transdermal administration may also be an alternative to the intravenous route, especially in cases of vascular damage (e.g. of neoplastic or chemotherapeutic origin).
In addition to the present results, other studies have confirmed that APrens might also be used as components of innovative lipofecting mixtures for targeted gene therapy [41]. Overall, we conclude that APrens represent very valuable compounds with a wide range of potential applications.
References
Surmacz L, Swiezewska E. Polyisoprenoids—secondary metabolites or physiologically important superlipids? Biochem Biophys Res Commun. 2011;407:627–32. https://doi.org/10.1016/j.bbrc.2011.03.059
Swiezewska E, Danikiewicz W. Polyisoprenoids: structure, biosynthesis and function. Prog Lipid Res. 2005;44:235–58. https://doi.org/10.1016/j.plipres.2005.05.002
Valtersson C, van Duyn G, Verkleij AJ, Chojnacki T, de Kruijff B, Dallner G. The influence of dolichol, dolichol esters, and dolichyl phosphate on phospholipid polymorphism and fluidity in model membranes. J Biol Chem. 1985;260:2742–51.
Hartley MD, Imperiali B. At the membrane frontier: a prospectus on the remarkable evolutionary conservation of polyprenols and polyprenyl-phosphates. Arch Biochem Biophys. 2012;517:83–97. https://doi.org/10.1016/j.abb.2011.10.018
Madeja Z, Rak M, Wybieralska E, Rózański I, Masnyk M, Chmielewski M, Łysek R, Chojnacki T, Jankowski W, Ciepichal E, Swiezewska E, Tekle M, Dallner G. New cationic polyprenyl derivative proposed as a lipofecting agent. Acta Biochim Pol. 2007;54:873–6.
Pirmohamed M, Breckenridge AM, Kitteringham NR, Park BK. Adverse drug reactions. BMJ Br Med J. 1998;316:1295–8.
Allen TM, Cullis PR. Drug delivery systems: entering the mainstream. Science. 2004;303:1818–22. https://doi.org/10.1126/science.1095833
Shimamoto K, Kimoto M, Matsuda Y, Asano K, Kajikawa M. Long-term safety and efficacy of high-dose controlled-release nifedipine (80 mg per day) in Japanese patients with essential hypertension. Hypertens Res. 2015;38:695–700. https://doi.org/10.1038/hr.2015.54
Gawrys O, Olszynski KH, Gawarecka K, Swiezewska E, Chojnacki T, Masnyk M, Chmielewski M, Kompanowska-Jezierska E. Cationic derivative of polyprenol, a potential component of liposomal drug carriers, does not alter renal function in rats. Eur J Lipid Sci Technol. 2014;116:659–62. https://doi.org/10.1002/ejlt.201300489
Gawrys O, Polkowska M, Roszkowska-Chojecka M, Gawarecka K, Chojnacki T, Swiezewska E, Masnyk M, Chmielewski M, Rafałowska J, Kompanowska-Jezierska E. Effects of liposomes with polyisoprenoids, potential drug carriers, on the cardiovascular and excretory system in rats. Pharmacol Rep. 2014;66:273–8. https://doi.org/10.1016/j.pharep.2013.09.009
Gleiter CH, Mörike KE. Clinical pharmacokinetics of candesartan. Clin Pharmacokinet. 2002;41:7–17. https://doi.org/10.2165/00003088-200241010-00002
Puranik MP, Wadher SJ, Kosarkar AL, Yeole PG. Method development and validation of candesartan cilexetil by RP-HPLC. Int J Res Pharm Biomed Sci. 2012;3:1227–30.
Hermida RC, Ayala DE, Smolensky MH, Fernández JR, Mojón A, Portaluppi F. Chronotherapy with conventional blood pressure medications improves management of hypertension and reduces cardiovascular and stroke risks. Hypertens Res. 2016;39:277–92. https://doi.org/10.1038/hr.2015.142
Kuczeriszka M, Olszyński KH, Gąsiorowska A, Sadowski J, Kompanowska-Jezierska E. Interaction of nitric oxide and the cytochrome P-450 system on blood pressure and renal function in the rat: dependence on sodium intake. Acta Physiol. 2011;201:493–502. https://doi.org/10.1111/j.1748-1716.2010.02222.x
Badzyńska B, Sadowski J. Renal hemodynamic responses to intrarenal infusion of acetylcholine: comparison with effects of PGE2 and NO donor. Kidney Int. 2006;69:1774–9. https://doi.org/10.1038/sj.ki.5000338
Nolin TD, Colaizzi IV, Palevsky PM, Matzke GR, Frye RF. Rapid microtiter plate assay for determination of inulin in human plasma and dialysate. J Pharm Biomed Anal. 2002;28:209–15. https://doi.org/10.1016/S0731-7085(01)00643-4
Maric C, Sandberg K, Hinojosa-Laborde C. Glomerulosclerosis and tubulointerstitial fibrosis are attenuated with 17beta-estradiol in the aging Dahl salt sensitive rat. J Am Soc Nephrol. 2004;15:1546–56. https://doi.org/10.1097/01.ASN.0000128219.65330.EA
Zhou XJ, Vaziri ND, Zhang J, Wang HW, Wang XQ. Association of renal injury with nitric oxide deficiency in aged SHR: prevention by hypertension control with AT1 blockade. Kidney Int. 2002;62:914–21. https://doi.org/10.1046/j.1523-1755.2002.00516.x
Neutel JM, Weir MR, Moser M, Harris S, Edwards D, Michelson EL, Wang R, Investigators AS. The effects of candesartan cilexetil in isolated systolic hypertension: a clinical experience trial. J Clin Hypertens. 2000;2:181–6.
Wang Z, Niu Q, Peng X, Li M, Liu K, Liu Y, Liu J, Jin F, Li X, Wei Y. Candesartan cilexetil attenuated cardiac remodeling by improving expression and function of mitofusin 2 in SHR. Int J Cardiol. 2016;214:348–57. https://doi.org/10.1016/j.ijcard.2016.04.007
Choisy SC, Kim S-J, Hancox JC, Jones SA, James AF. Effects of candesartan, an angiotensin II receptor type I blocker, on atrial remodeling in spontaneously hypertensive rats. Physiol Rep. 2015;3:e12274. https://doi.org/10.14814/phy2.12274
Skov K, Mogensen S, Mulvany MJ. Persistent effect of treatment with candesartan cilexetil on blood pressure in spontaneously hypertensive rats. J Renin Angiotensin Aldosterone Syst. 2001;2:S91–4. https://doi.org/10.1177/14703203010020011601
Nishimura Y, Ito T, Saavedra JM. Angiotensin II AT(1) blockade normalizes cerebrovascular autoregulation and reduces cerebral ischemia in spontaneously hypertensive rats. Stroke. 2000;31:2478–86. https://doi.org/10.1161/01.STR.31.10.2478
Nishimura Y, Xu T, Jöhren O, Häuser W, Saavedra JM. The angiotensin AT1 receptor antagonist CV-11974 regulates cerebral blood flow and brain angiotensin AT1 receptor expression. Basic Res Cardiol. 1998;93:63–68. Suppl 2
Keppler A, Gretz N, Schmidt R, Kloetzer H-M, Groene H-J, Lelongt B, Meyer M, Sadick M, Pill J. Plasma creatinine determination in mice and rats: an enzymatic method compares favorably with a high-performance liquid chromatography assay. Kidney Int. 2007;71:74–8. https://doi.org/10.1038/sj.ki.5001988
Lopez-Giacoman S, Madero M. Biomarkers in chronic kidney disease, from kidney function to kidney damage. World J Nephrol. 2015;4:57–73. https://doi.org/10.5527/wjn.v4.i1.57
Bentinger M, Tekle M, Brismar K, Chojnacki T, Swiezewska E, Dallner G. Polyisoprenoid epoxides stimulate the biosynthesis of coenzyme Q and inhibit cholesterol synthesis. J Biol Chem. 2008;283:14645–53. https://doi.org/10.1074/jbc.M710202200
Bergamini E, Bizzarri R, Cavallini G, Cerbai B, Chiellini E, Donati a GoriZ, Manfrini a, Parentini I, Signori F, Tamburini I. Ageing and oxidative stress: a role for dolichol in the antioxidant machinery of cell membranes? J Alzheimers Dis. 2004;6:129–35.
Van Meer L, Moerland M, Cohen AF, Burggraaf J. Urinary kidney biomarkers for early detection of nephrotoxicity in clinical drug development. Br J Clin Pharmacol. 2014;77:947–57. https://doi.org/10.1111/bcp.12282
Boudonck KJ, Mitchell MW, Német L, Keresztes L, Nyska A, Shinar D, Rosenstock M. Discovery of metabolomics biomarkers for early detection of nephrotoxicity. Toxicol Pathol. 2009;37:280–92. https://doi.org/10.1177/0192623309332992
Garrett MR, Joe B, Yerga-Woolwine S. Genetic linkage of urinary albumin excretion in Dahl salt-sensitive rats: influence of dietary salt and confirmation using congenic strains. Physiol Genom. 2006;25:39–49. https://doi.org/10.1152/physiolgenomics.00150.2005
Feld LG, Cachero S, Van Liew JB., Zamlauski-Tucker M, Marianna Noble B Enalapril and renal injury in spontaneously hypertensive rats. Hypertension. 1990;16:544–54. https://doi.org/10.1161/01.HYP.16.5.544
Komatsu K, Frohlich ED, Ono H, Ono Y, Numabe A, Willis GW. Glomerular dynamics and morphology of aged spontaneously hypertensive rats. Eff angiotensin-Convert Enzym Inhib Hypertens. 1995;25:207–213.
Inoue BH, Arruda-Junior DF, Campos LC, Barreto ALT, Rodrigues MV, Krieger JE, Girardi ACC. Progression of microalbuminuria in SHR is associated with lower expression of critical components of the apical endocytic machinery in the renal proximal tubule. Am J Physiol Ren Physiol. 2013;305:F216–26. https://doi.org/10.1152/ajprenal.00255.2012
Reckelhoff JF, Zhang H, Granger JP. Decline in renal hemodynamic function in aging SHR: role of androgens. Hypertension. 1997;30:677–81. https://doi.org/10.1161/01.HYP.30.3.677
Skov K, Nyengaard JR, Korsgaard N, Mulvany MJ. Number and size of renal glomeruli in spontaneously hypertensive rats. J Hypertens. 1994;12:1373–6. http://www.ncbi.nlm.nih.gov/pubmed/7706696
Johnson RJ, Feig DI, Nakagawa T, Sanchez-Lozada LG, Rodriguez-Iturbe B. Pathogenesis of essential hypertension: historical paradigms and modern insights. J Hypertens. 2008;26:381–391. https://doi.org/10.1097/HJH.0b013e3282f29876
Rodríguez-Iturbe B, Quiroz Y, Nava M, Bonet L, Chávez M, Herrera-Acosta J, Johnson RJ, Pons HA. Reduction of renal immune cell infiltration results in blood pressure control in genetically hypertensive rats. Am J Physiol Ren Physiol. 2002;282:F191–201. https://doi.org/10.1152/ajprenal.0197.2001
Prausnitz MR, Langer R. Transdermal drug delivery. Nat Biotechnol. 2008;26:1261–8. https://doi.org/10.1007/978-3-642-00477-3_13
Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189–99. https://doi.org/10.1089/bar.2012.9960
Grecka E, Statkiewicz M, Gorska A, Biernacka M, Grygorowicz MA, Masnyk M, Chmielewski M, Gawarecka K, Chojnacki T, Swiezewska E, Malecki M. Prenyl ammonium salts—new carriers for gene delivery: a B16-F10 mouse melanoma model. PLoS ONE. 2016;11:e0153633 https://doi.org/10.1371/journal.pone.0153633
Acknowledgements
This work was supported by the Polish National Cohesion Strategy, Innovative Economy Grant No. UDA-POIG.01.03.01-14-036/09-00). OG has been supported by a scholarship from the European Social Fund, Human Capital Operational Programme. We like to express special thanks to Malgorzata Modrzewska-Lewczuk from the Scientific Documentation Unit of Mossakowski Medical Research Centre (PAS) for preparing macroscopic images of harvested kidneys.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Gawryś, O., Baranowska, I., Gawarecka, K. et al. Innovative lipid-based carriers containing cationic derivatives of polyisoprenoid alcohols augment the antihypertensive effectiveness of candesartan in spontaneously hypertensive rats. Hypertens Res 41, 234–245 (2018). https://doi.org/10.1038/s41440-018-0011-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0011-y
This article is cited by
-
The treatment with sGC stimulator improves survival of hypertensive rats in response to volume-overload induced by aorto-caval fistula
Naunyn-Schmiedeberg's Archives of Pharmacology (2023)
-
Polyprenol-Based Lipofecting Agents for In Vivo Delivery of Therapeutic DNA to Treat Hypertensive Rats
Biochemical Genetics (2021)