Abstract
Background/objectives
Tablet-based perimetry could be used to test for glaucomatous visual field defects in settings without easy access to perimeters, although few studies have assessed diagnostic accuracy of tablet-based tests. The goal of this study was to determine the diagnostic accuracy of iPad perimetry using the visualFields Easy application.
Subjects/methods
This was a prospective, cross-sectional study of patients undergoing their first Humphrey Field Analyser (HFA) visual field test at a glaucoma clinic in India. Participants underwent 24-2 SITA Standard HFA testing and iPad-based perimetry with the visualFields Easy application. Reference standards for both visual field loss and suspected glaucoma were determined by ophthalmologist review of HFA results and optic disc photographs. Receiver operating characteristic curves were constructed to assess diagnostic accuracy at various test thresholds.
Results
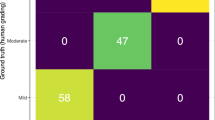
203 eyes from 115 participants were included, with 82 eyes classified as moderate or worse glaucoma. iPad perimetry had an area under the receiver operating characteristic (AUROC) curve of 0.64 (95% CI 0.57 to 0.71) for detection of any visual field defect relative to HFA and an AUROC of 0.68 (0.59 to 0.76) for detection of moderate or worse glaucoma relative to ophthalmologist examination. At a set specificity of 90%, the sensitivity of iPad perimetry for detection of moderate or worse glaucoma was 35% (22–48%).
Conclusions
iPad perimetry using the visualFields Easy application had inadequate diagnostic accuracy to be used as a screening tool for glaucoma in this South Indian population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Broadway DC. Visual field testing for glaucoma—a practical guide. Community Eye Health. 2012;25:66–70.
Wu Z, Medeiros FA. Recent developments in visual field testing for glaucoma. Curr Opin Ophthalmol. 2018;29:141–6.
John D, Parikh R. Cost-effectiveness of community screening for glaucoma in rural India: a decision analytical model. Public Health. 2018;155:142–51.
Jones PR, Lindfield D, Crabb DP. Using an open-source tablet perimeter (Eyecatcher) as a rapid triage measure for glaucoma clinic waiting areas. Br J Ophthalmol. 2021;105:681–6.
Anderson AJ, Johnson CA. Frequency-doubling technology perimetry. Ophthalmol Clin North Am. 2003;16:213–25.
Ong EL, Zheng Y, Aung T, Tan L, Cheng CY, Wong TY, et al. Performance of the Moorfields motion displacement test for identifying eyes with glaucoma. Ophthalmology. 2014;121:88–92.
Schulz AM, Graham EC, You Y, Klistorner A, Graham SL. Performance of iPad-based threshold perimetry in glaucoma and controls. Clin Exp Ophthalmol. 2018;46:346–55.
Kong YXG, He M, Crowston JG, Vingrys AJ. A Comparison of perimetric results from a tablet perimeter and Humphrey Field Analyzer in glaucoma patients. Transl Vis Sci Technol. 2016;5:2.
Johnson CA, Thapa S, George Kong YX, Robin AL. Performance of an iPad application to detect moderate and advanced visual field loss in Nepal. Am J Ophthalmol. 2017;182:147–54.
Ichhpujani P, Thakur S, Sahi RK, Kumar S. Validating tablet perimetry against standard Humphrey Visual Field Analyzer for glaucoma screening in Indian population. Indian J Ophthalmol. 2021;69:87–91.
Santos AS, Morabe ES. “VisualFields Easy”: an iPad Application as a simple tool for detecting visual field defects. Philipp J Ophthalmol. 2016;41:5.
Keltner JL, Johnson CA, Cello KE, Edwards MA, Bandermann SE, Kass MA, et al. Classification of visual field abnormalities in the Ocular Hypertension Treatment Study. Arch Ophthalmol. 2003;121:643–50.
Mills RP, Budenz DL, Lee PP, Noecker RJ, Walt JG, Siegartel LR, et al. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am J Ophthalmol. 2006;141:24–30.
Kumar RS, Ramgopal B, Rackenchath MV, A V SD, Mannil SS, Nagaraj S, et al. Comparison of structural, functional, tonometric, and visual acuity testing for glaucoma: a prospective diagnostic accuracy study. Ophthalmol Glaucoma. 2022;5:345–52.
Dabasia PL, Fidalgo BR, Edgar DF, Garway-Heath DF, Lawrenson JG. Diagnostic accuracy of technologies for glaucoma case-finding in a community setting. Ophthalmology. 2015;122:2407–15.
Acknowledgements
The authors thank Phani Kishore for logistical and technological support during the study.
Funding
This work was supported by the Fortisure Foundation, the National Institutes of Health (grant UG1EY028097), Research to Prevent Blindness (Medical Student Eye Research Fellowship), and That Man May See.
Author information
Authors and Affiliations
Contributions
QRR performed statistical analysis, created figures and tables, and wrote the first draft of the paper. RSK designed the study, collected data, was responsible for implementation of the study and interpreted the results. BR, MVR, SDA, SSM, and SN collected data. CAM, DMW, and KSO helped implement the study. JTO interpreted the results. RLS procured funding, conceived of the study, designed the study, collected data, and interpreted the results. JDK designed and helped implement the study, collected data, and interpreted the results. All co-authors interpreted and critically edited the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41433_2022_2223_MOESM1_ESM.docx
Supplemental Figure 1. Correlation between visualFields Easy and Humphrey Field Analyser (HFA) among eyes with reliable visualFields Easy results.
41433_2022_2223_MOESM2_ESM.docx
Supplemental Figure 2. Receiver operating characteristic (ROC) curves for detection of visual field defects among eyes with reliable visualFields Easy results.
41433_2022_2223_MOESM3_ESM.docx
Supplemental Figure 3. Receiver operating characteristic (ROC) curves for detection of eye-level glaucoma among eyes with reliable visualFields Easy results.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Richardson, Q.R., Kumar, R.S., Ramgopal, B. et al. Diagnostic accuracy of an iPad application for detection of visual field defects. Eye 37, 1690–1695 (2023). https://doi.org/10.1038/s41433-022-02223-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02223-y