Abstract
There has been much interest in the role of oral nicotinamide supplementation in reducing the incidence of non-melanoma skin cancers. This article reviews the hypothesised mechanisms of action of nicotinamide, and the available literature outlining its role for this purpose. There have been five randomised controlled trials (RCT), one histopathological study and two case series exploring the effect of oral nicotinamide supplementation on UV-induced immunosuppression of the skin, and incidence of actinic keratoses and non-melanoma skin cancers (NMSC). The largest RCT received criticism of the statistical analyses used, but the critics still acknowledged a likely benefit of treatment with oral nicotinamide in reducing the incidence of NMSC. Nicotinamide has a favourable safety profile. Current evidence is not definitive that oral nicotinamide supplementation reduces the incidence of NMSC, but it constitutes a low-risk management option that may be particularly relevant for high-risk individuals, and should be discussed as an option for these patients.
摘要
人们对口服烟酰胺补充剂在降低非黑色素瘤皮肤癌发病率中的作用抱有极大兴趣。本文总结了烟酰胺现有的可能作用机制并对相关文献进行了概述。有5项随机对照试验(RCT)、1项组织病理学研究和2项病例系列研究探索了口服烟酰胺补充剂针对紫外线诱导的皮肤癌免疫抑制的疗效, 以及其对降低光化性角化病和非黑色素瘤皮肤癌(NMSC)发生率的作用。一项大型的RCT研究虽然由于其统计分析遭到质疑, 但质疑者仍然承认口服烟酰胺在降低NMSC发病率上可能有益处。烟酰胺具有可靠的安全性优势。目前的证据仍不能证明口服烟酰胺补充剂可降低NMSC的发生率, 但它是一种低风险的治疗选择, 适合于高危个体的治疗, 应进一步探讨其作为高危病人治疗选择的可行性。
Similar content being viewed by others
Introduction
Nicotinamide (also known as niacinamide), hereafter NAM, is an amide derivative of vitamin B3. Humans are unable to produce it endogenously, and must derive it from exogenous sources [1]. It is found in meat, fish, legumes, mushrooms, nuts and grains, and has an active role in protecting cells from ultraviolet (UV) radiation-induced damage [2,3,4]. UV exposure is a recognised risk factor in the development of non-melanoma skin cancer (NMSC) [2], which has sparked interest in the role of oral NAM supplementation for reducing the incidence of these malignancies. NMSC is the most common malignancy in the white population [5], and a frequent presentation to oculoplastic services [6]. In this article, we review the current literature on oral supplementation of NAM and NMSC incidence, and consider how the use of NAM may be applied to ophthalmology.
Methods
A literature search using PubMed and Medline was carried out with search terms ‘nicotinamide’, ‘vitamin B3’, ‘niacinamide’, ‘basal cell carcinoma’, ‘BCC’, ‘squamous cell carcinoma’, ‘SCC’, ‘skin cancer’ and ‘chemoprevention’. Articles not written in English or focusing on topical administration of NAM were excluded. Relevant articles and their bibliographies were reviewed to identify further pertinent sources.
Results
The literature search resulted in 291 unique articles. Article review identified five randomised controlled trials (RCT) (two exploring localised UV-induced immunosuppression, one, incidence rates of actinic keratosis, and two, rates of NMSC), one histopathological study and two case series. Figure 1 gives an overview of the article review process.
Nicotinamide and cellular pathways
UV-irradiation to skin causes DNA damage that instigates a cascade of cellular responses to repair [2, 7]. DNA repair is an energy-intensive process, and inadequate levels of adenosine triphosphate (ATP) may limit these efforts and ultimately result in cell death. UV-irradiation depletes nicotinamide adenine dinucleotide (NAD+), which is required for the generation of ATP. This is exacerbated by UV exposure related overactivation of poly-adenosine diphosphate ribose polymerase (PARP), which blocks glycolysis and further reduces available NAD+.
NAM is theorised to support DNA repair following UV exposure via dual mechanisms as it is a precursor of NAD+, and a direct inhibitor of PARP. NAM, therefore, increases available NAD+, and supports maintenance of adequate ATP levels to drive the highly energy-dependent DNA repair process. Other theories on NAM’s protective mechanism of action include the inhibition of sirtuin enzymatic pathways, which regulate cellular metabolism and are pro-inflammatory [8]. Sirtuin 1, which inhibits apoptosis, has been found to be over-expressed in biopsy samples of NMSC [9, 10]. NAM may offer further photoprotection due to its impact on the immune system, since it is recognised to modulate a variety of cytokines including IL-1ß, IL-6, IL-8, TNF and IFN-g, and may have downstream effects on calcium-based leukocyte signalling and CD38-related NAD + regulation [7, 11, 12]. However, PARP-deficient cells have been shown to have higher rates of cell death, meaning there may be a balance with the effect of NAM-inhibition, and an in-vitro study on irradiated mouse cells by Riklis et al. [11] showed a concentration-dependent effect on DNA repair.
Clinical applications – effect on cell senescence
Senescent cells are thought to be induced by oxidative stress, and increase in number with age. Senescent fibroblasts in skin are thought to contribute to the development of NMSC [1]. Mahajan et al. [1] undertook a series of experiments to evaluate the effect of both creatine and NAM on the number of senescent cells produced by treating dermal human neonatal fibroblasts with hydrogen peroxide (H2O2) for 2 h. Some cells were pre-treated for 24 h with creatinine, NAM, or both. Some were treated 2 h following the exposure to H2O2, some were treated with water and some not treated at all, to act as controls. Cells were incubated for 72 h post-H2O2 treatment with some cells removed at 24, 48 and 72 h for analysis. Pre-treatment for 2 days with either creatine or NAM resulted in reduced markers associated with senescent cells, with no additional improvements noted when they were combined. Similarly, pre-treatment with either creatine or NAM attenuated the impact of H2O2 on senescent-cell-induced changes in cytokine expression. As before, effects were similar for separate and combined use of creatine and NAM. However, treatment after exposure to H2O2 failed to achieve this effect. Furthermore, pre-treatment with creatine, NAM or both was shown to reduce the H2O2-induced increases in intracellular reactive oxygen species. This study lends support to the use of NAM as prophylaxis to reduce the incidence of NMSC, but not as a treatment option for NMSC. However, this is an in-vitro study relying on topical treatment, and further studies would be required in-vivo to elucidate the effect of oral supplementation on fibroblast senescence.
Clinical applications – effect on UV-induced immunosuppresion
In 2009, Yiasemides et al. [2] undertook a double blinded, randomised, controlled, crossover trial to evaluate the impact of oral NAM on UV-induced immunosuppression. It is recognised that UV radiation equivalent to daily ambient sun exposure is adequate to suppress delayed hypersensitivity responses to recall antigens. The authors applied this knowledge and evaluated the impact of oral NAM in healthy, Mantoux-positive volunteers. Volunteers took either NAM tablets or visually-matched placebo for 1 week. From day 3, three areas of the lower back received irradiation from a solar simulator with UV designed to replicate natural sunlight. Each area was irradiated with a different dose of radiation (1, 2 and 4 J/cm2) once daily for 3 consecutive days, after which they underwent Mantoux testing, alongside an adjacent, untreated area. The results of the Mantoux testing were evaluated 72 h later. Following a 4-week washout period, the process was repeated on the other side of the lower back, with volunteers switching from treatment to placebo, or vice versa. Of note, two different doses of NAM were used – one group took 500 mg NAM once daily (low dose group, n = 31), and the other took 500 mg 3 times a day (high dose group, n = 30). All volunteers had their minimal erythema dose – the minimum UV exposure required to generate a barely perceptible erythema 24 h later – established by testing on the upper back at the beginning of each arm of the study. The researchers also measured erythrocyte NAD+ levels in five fasted volunteers - 30, 60 and 90 min after consumption of a 500 mg NAM tablet. Oral NAM did not affect minimal erythema thresholds in either the low or high dose groups; neither did oral NAM affect hypersensitivity reactions on unirradiated sites. Immunosuppression was noted in a dose-dependent manner in both placebo and treatment groups; in those receiving NAM supplements, there was significantly less immunosuppression noted (p < 0.001), with similar responses in the high and low dose groups. Sub-analysis to identify risk factors for immunosuppression did not identify links with age or gender but did find an inverse relationship with minimal erythema dose, suggesting volunteers with paler complexion experienced greater immunosuppression than those with darker complexions. Blood levels of NAD+ peaked at 30% of baseline 1 h after NAM tablet ingestion, returning to baseline by 90 min, which the authors hypothesise meant the NAM was rapidly absorbed by tissues, though they highlight that it is not yet known how that correlates with NAD+ levels in skin. There were no reported adverse effects. The authors concluded that low dose oral NAM supplementation confers protection against photoimmunosuppression without any effect on tendency to sunburn and may offer inexpensive and well-tolerated protection against skin cancer.
Thanos et al. [13] used very similar methodology to explore the effect of both oral (and topical) NAM prior to photodynamic therapy (PDT) on local immunosuppression. Drawing on healthy, Mantoux-positive volunteers, they undertook a double-blind, placebo-controlled crossover study using high and low irradiance rates of PDT. PDT was found to induce local immunosuppression with high irradiance PDT having a larger effect (up to 50% suppression) than low irradiance PDT (up to 22%). Oral NAM reduced the observed immunosuppression by up to 69%.
Clinical applications – actinic keratoses and non-melanoma skin cancer
Surjana et al. [14] undertook a randomised, placebo-controlled, double blinded study into the number of actinic keratoses (AK) present in patients receiving oral NAM 500 mg either once or twice daily for a 4-month period. Participants were examined at baseline, 2 months and 4 months, with relative reductions in numbers of AK of up to 48% noted (35% in the twice daily group at both 2 and 4 months, 15 and 29% in the once daily group, all reaching statistical significance). Given the recognised link between number of AK and development of NMSC [15], the authors also noted the incidence of new biopsy-proven diagnoses of cutaneous malignancies. Prior histopathological diagnoses of cutaneous malignancies prior to enrolment occurred in 81% and 79% of participants in placebo and treatment groups. During the 4-month trial, 20 new NMSCs developed in 11 patients in the placebo group, and four developed in two patients in the treatment group with an odds ratio of developing a new NMSC in the NAM group of 0.14 (p = 0.019).
Chen et al. [16]. undertook a phase III controlled trial of 386 ‘high-risk’ participants randomised to 12 months of oral NAM (500 mg twice daily) or placebo, known as the ONTRAC study, and outlined a 23% reduction in the development of NMSCs at 12 months (p = 0.02). ‘High risk’ was defined as having had at least two NMSCs (basal cell carcinoma - BCC, squamous cell carcinoma – SCC, and Bowen’s disease) in the previous 5 years. The reduction appeared to be similar in the development of BCC (20%, p = 0.12) compared with SCC (30%, p = 0.05), with greatest effect seen among superficial BCC (although, as these are more common amongst immunosuppressed patients, their pathogenesis is likely to differ from the other subtypes). The effect was also greater amongst patients who had a higher number of NMSCs in the 5 years prior to the study. The incidence of AKs was also studied as a secondary endpoint and found to be 13% lower at 12 months. There were no differences found between the groups 6 months after NAM treatment was stopped, suggesting that the effect of treatment only persists whilst the patient is actively taking NAM.
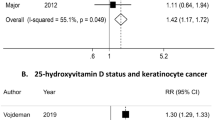
The findings of this RCT were discussed widely in the literature, which, in part, included criticism of its statistical analysis [17,18,19,20]. Gilmore et al. [17] performed a retrospective Bayesian analysis based on Chen et al.’s reported findings, and demonstrated that there was insufficient evidence to make any positive statements regarding NAM’s efficacy. They suggested that the true reduction in NMSC incidence rate is likely to be in the region of 5%, which the authors did not believe to be sufficient to recommend its use, although improved study design and increased sample sizes would be required to prove this with a meaningful statistical significance.
A specific criticism of the ONTRAC study lies in the fact that their primary endpoint was a composite one - the occurrence of BCC, SCC and Bowen’s disease, all counted as one – with the power calculation based on the same [17]. Given that the effect of NAM on the pathogenesis of tumour development is likely to differ between these three clinical entities, it would be clinically useful to investigate its effect on their incidence rates separately, which would necessitate different power calculations and, subsequently, larger sample sizes.
Gilmore et al. [17], however, also acknowledge that there was no evidence to conclude that NAM does not provide any benefit. Furthermore, they agree that given the underlying pathophysiology, NAM is likely to have a preventative effect on NMSC, but warn that higher standards of evidence will be required to prove it.
Minocha et al. [21] analysed pathological specimens of tumours arising as part of the ONTRAC study, examining 70 tumours (BCC or SCC) from the placebo group, and 60 from the NAM group. They found statistically lower levels of CD68+ positive cells in the NAM group, without statistically lower levels of CD163, suggesting a specific reduction in M1 macrophages. CD68+ cells have previously been found in higher levels in SCC than normal skin and M1 macrophages produce pro-carcinogenic reactive oxygen species and inflammation [21, 22]. The authors suggest that NAM reduces M1 macrophage-associated tumorigenesis. Tumours that arose in sun-exposed areas were also assessed for markers of DNA damage. Although these tended to lower levels in the NAM group, these did not reach statistical significance. The authors postulate this may relate to diverse sampling with respect to time between sun exposure and tumour excision. They also highlight that these analyses were performed on lesions that arose despite treatment with NAM, and the effect on areas of skin that did not develop tumours was outside the scope of this research [21].
Chen et al. [23] also reported a double blinded, placebo-controlled study with stable, immunosuppressed post-renal transplant patients randomised to receive oral NAM 500 mg twice daily or placebo for 6 months. Such patients are at high risk of developing NMSC, especially SCCs, which have been reported as occurring with a frequency up to 250 fold that of immunocompetent individuals [9, 24]. Patients were examined at baseline, then every 2 months for 6 months. They also undertook blood and urine testing at regular intervals to establish safety of NAM supplementation in this patient group. The primary endpoint was rate of new NMSC, with secondary endpoints separating these into BCC, SCC and AK. Although trends towards lower rates of new lesions were noted in the treated group, and they report an outlier in the placebo group that may have affected analyses, none of the endpoints reached statistical significance. The authors note similar rates of reduction compared with their ONTRAC study in immunocompetent individuals and speculate that larger numbers would reach statistical significance. Unfortunately, the study struggled to recruit the intended numbers required by their power calculations and was stopped early with only 25% of the intended participants. Yélamos et al. [25] echo Gilmore et al. [17] concerns about evaluating all NMSC subtypes together and highlight the underpowering of both of Chen et al.’s studies. They also raise particular concerns regarding the increased number of more aggressive lesions such as morpheiform BCCs and poorly differentiated SCCs in the ONTRAC treated group. They advocated larger studies to explore this.
In response to Chen et al. [23] reported findings, Drago et al. [26] reported positive responses in post-renal transplant patients, later publishing a similar study which also included post-hepatic transplant patients [27]. Both studies constituted small case control studies comparing size and number of AKs at baseline and after 6 months with treatment groups given oral NAM. The renal-only study used a regime of 250 mg 3 times a day. Unfortunately, the second study reports conflicting regimes, with the abstract reporting 500 mg once daily and the main body of the text stating 250 mg three times daily. Blood monitoring established there was no effect on immunosuppressant drug levels throughout the treatment periods. In the treated group, five of 19 patients underwent biopsy of a lesion clinically consistent with AK at baseline, which confirmed the diagnosis. The treated groups in both studies showed at least partial regression of at least one lesion in 88% of individuals, with 44% and 42% respectively showing complete regression of at least one lesion. No new lesions developed, and none transformed to SCC, whereas both untreated groups showed enlargement of lesions, development of new lesions, or transformation to SCC. In the second study, using area of AK in cm2, they showed statistically significant differences between the treated and untreated groups (p = 0.01). Unfortunately, there does not appear to be any evidence of blinding of the researchers evaluating the lesions. The authors speculate that their results differ to those of Chen et al. [23] due to different levels of immunosuppression, or drug choice, and note that Chen et al. did not report this information, so they are unable to compare the cohorts in this respect. They advocate larger studies with longer follow-up periods to confirm their findings.
Ferreira et al. [28] undertook a two-pronged study exploring the effects of the both oral NAM, and topical 5-Flurouracil (5FU) on skin field cancerisation. They recruited 36 patients with 3-10 AKs on a forearm. Patients were first randomised to receive 500 mg oral NAM twice daily, or placebo (blinded), then randomised again to use topical 5FU 3 times a day or SPF 30 sunscreen 3 times a day on their forearm for 120 days. Evaluations explored clearance of AKs, changes in forearm photoageing scales, and biopsy samples from areas clinically AK-free looking at epithelial dysplasia, using expression of both p53 and Ki67 markers. 5FU reduced the overall number of AKs compared with use of sunscreen, but did not reach statistical significance in clearance of AKs or in epithelial dysplasia markers. NAM was not shown to have any impact, except in reducing the expression of Ki67, which did reach statistical significance. However, patient numbers were small, three patients failed to complete the courses (not related to the use of NAM) and the side effect profile of NAM was favourable, and much less than that of 5FU. The authors speculate that a longer course of NAM might have demonstrated a clinical benefit not identified in this research.
Side effects and tolerability
Oral nicotinamide has been used for a variety of clinical indications, including: autoimmune blistering disorders such as bullous pemphigoid, acne, depression, and prevention of type 1 diabetes mellitus and degenerative neurological disorders [7, 29, 30].
Studies in rodents raised concerns regarding toxicity of NAM, with doses resulting in death of half of the population at 2.5 g/kg [30]. However, studies in humans have reported good tolerability at higher doses, with no adverse effects reported in children treated for 5 years with doses of 25–50 mg/kg/day, and reported practice of doses up to 3 g per day in adults [30].
Reported side effects include temporary headache, dizziness and vomiting in fasted individuals who consumed 6 g orally, resolving upon withdrawal [30, 31]. Reversible hepatotoxicity has been reported in doses of 9–10 g/day [32, 33].
Surjana et al. [14] reported good compliance (94–98% as determined by rates of returned tablets at the end of their trial) in patients taking 500 mg either once or twice daily, with one report of nausea. They also reported that blood tests (full blood count, creatinine and liver function) taken at 2 months did not show any clinically significant changes compared with baseline, though they do not elaborate on what changes, if any, were noted.
Caution should be taken in patients with hepatic disease, which delays clearance of plasma levels [33]. Due to differences in metabolic pathways, side effects reported by non-human studies may not be representative of effects in humans. Older studies may be difficult to interpret due to use of products contaminated by nicotinic acid, with its different side effect profile. Concerns raised regarding NAM-induced insulin resistance in rats appear unfounded in humans; a double-blind, randomised, placebo-controlled trial found no difference in incidence of diabetes in individuals with diabetic relatives who had islet-cell antibodies and received 1.2 g/m2 oral NAM for 5 years [33, 34]. A 7-year study offering 1.2 g/m2 oral NAM to children found to have islet-cell antibodies compared incidence of diabetes in the treated group compared with those who declined treatment and found that rates of diabetes were 41% of that in the untreated group, suggesting a possible protective effect, though this methodology is less robust than that of a RCT [35].
Oral NAM has been associated with an overall lowering of phosphate levels [9, 36]. Whilst this could theoretically be problematic in patients on long-term supplementation, this has not been reported in the studies where patients have taken nicotinamide for years [34, 35]. Furthermore, it is theorised this may be of clinical benefit in patients with end-stage renal disease, or post-renal transplant patients, in whom hyperphosphataemia is correlated with cardiovascular morbidity and graft rejection [9]. Unfortunately, one study found it was equally effective but less well-tolerated than sevelamer in haemodialysis patients, with 45% of patients in the NAM arm failing to complete the course: half of these due to side effects [36]. Doses were titrated between 0.5 and 2 g per day, and it may be that these doses were too high for this population.
Some interest has been shown regarding the use of NAM in patients with Parkinson’s disease. A trial by Green [37] comparing excretion of NAM metabolic products after oral administration of 50 mg NAM in individuals with motor neurone disease or Parkinson’s disease against control identified abnormal excretion rates in patients with Parkinson’s disease. The authors speculated that this may be due to an underlying enzymatic dysfunction of hydroxylation resulting in a build-up of neurotoxic derivatives, though this study is not designed to confirm a causative effect [37]. Zhao et al. [38] summarise the current evidence, which is inconclusive. There is evidence to suggest an optimal therapeutic window with respect to neuroprotection from NAM, with excessive levels being potentially neurotoxic. However, Alisky [39] reports a case of a patient receiving oral nicotinic acid (also known as niacin, a precursor to NAM) whose Parkinsonian symptoms of bradykinesia and rigidity improved with increasing doses of nicotinic acid, but relapsed upon nicotinic acid withdrawal due to side effects of nightmares and skin rash. Concurrent research during the ONTRAC study failed to identify any neurocognitive effect of oral NAM supplementation, though they highlight that other more vulnerable populations may be more likely to demonstrate a change [40]. It seems prudent to avoid oral supplementation in patients with Parkinson’s disease until further research can elucidate this issue.
NAM crosses the placenta, with higher levels in foetuses than mothers. No formal studies have evaluated the safety of oral nicotinamide supplementation in pregnancy or breastfeeding, but no concerns appear to have been raised in the literature [33].
Zhao [41] analysed the data reported in Chen et al. [16] phase III trial in immunocompetent individuals, and identified statistically significantly higher rates of mucocutaneous infections within the group receiving oral nicotinamide, though the original authors believe this falls within the realms of chance, highlighting that non-mucocutaneous infection rates were higher in the placebo group and that nicotinamide has been found to reduce skin infections in mouse models [8].
Future areas of research
Gollins et al. [42] recently undertook a survey of dermatologists and clinicians working in transplant units across the UK, as well as a survey of solid organ transplant recipients. They aimed to assess current practices regarding systemic chemoprevention drug use and establish feasibility for a UK-based RCT studying the use of oral NAM to reduce the incidence of SCC in these high-risk patients. Of all clinician respondents, 73% had initiated systemic chemoprevention, 60% using acitretin as their first line treatment option. NAM has been used by 24%. Feasibility for the study appeared good, with 82% of clinicians expressing a willingness to recruit patients, and 72% of patient respondents indicating a willingness to participate.
Perceptions of Nicotinamide in NMSC prevention
Fania et al. [43] recently undertook a survey amongst Italian dermatologists exploring perceptions of the use of systemic photoprotective agents in reducing the risk of NMSC, which included NAM. 85.2% believe that systemic photoprotection plays a role in reducing the risk of NSMC. Of those who had prescribed just one of the treatment options enquired about, most reported prescribing NAM (31.5%). The majority of prescriptions were given for short-term use: 56.1% covering the 2–3 month summer period.
A 2021 survey of Mohs surgeons in the United States by Desai et al. [44] examined prescribing habits and perceptions over the safe use long-term of oral NAM. Of 160 respondents, 76.9% recommend nicotinamide for the prevention of NMSC – 70% consider oral NAM in patients who develop at least two NMSCs over 2 years, and 44.4% frequently or always recommend oral NAM to organ transplant recipients to prevent SCC. Clinicians practising for more than 10 years, and those expressing uncertainty or concern regarding the long-term use of oral NAM were less likely to have recommended its use in the previous year. Unfortunately, the number of respondents represented only 11.3% of invited clinicians, and those that responded may represent a biased sample of those with particularly strong views regarding this use of oral NAM. However, with 20% of respondents recommending oral NAM to at least 100 patients in the previous year, the number of patients affected is considerable, and the authors recommend further studies into safety profiling and cost-effectiveness of oral NAM in this context.
The National Comprehensive Cancer Network, consisting of 31 cancer centres in the USA, incorporated the use of NAM as a preventative management option for SCC in their 2017 guidelines, particularly referencing its better side effect profile than oral retinoids: an alternative systemic chemopreventative treatment option [45]. A 2021 meta-analysis by Tee et al. [46] reported no difference between oral retinoids and NAM for prevention of AK and NMSC, prompting Hoegler et al. [47] to recommend NAM as first line treatment for prevention of NMSC. They highlight the logistical barriers of using oral retinoids such as prescription requirement, dose titration, monitoring blood tests, and teratogenicity that are not encountered when prescribing NAM.
However, consensus-based guidelines on invasive cutaneous SCC were updated for the European Dermatology Forum and published in 2020, which acknowledged the evidence regarding nicotinamide in this role, but did not recommend its routine use [48]. A consensus paper of Italian dermatology opinions on management of AK, also published in 2020, perceived nicotinamide favourably for reducing the incidence of SCCs [49]. Furthermore, Cosio et al. [50] propose that nicotinamide be incorporated into a multi-drug approach alongside hedgehog inhibitors, arsenic trioxide, itraconazole, and all-trans retinoic acid for locally advanced or treatment-resistant BCC. They recommend the combination due to different, but synergistic, mechanisms of action on cellular metabolism, citing the potential for reduced drug-resistance, and lower required dosages of each drug, thereby minimising side effect profiles.
Nicotinamide versus nicotinic acid
NAM contains an amide group, which differentiates it from nicotinic acid (also known as niacin), which is an acidic variant of vitamin B3 [51]. Nicotinic acid is a precursor to NAM and is converted into NAM in vivo [52, 53]. Administered orally, it has been used as a treatment for hyperlipidaemia [3]. However, it has a vasodilatory effect that results in flushing, headache and hypotension and limited its clinical application [51, 52]. Although nicotinic acid may have similar effects on cellular pathways regarding maintenance of NAD+ levels [30], its side effect profile is significant and the two should not be confused or used interchangeably [51, 54, 55]. The difference must be specifically highlighted to patients if recommending NAM to prevent confusion and unintended side effects.
Topical or oral nicotinamide
This review focuses on oral administration of NAM. Topical NAM is also available, and has evidence supporting its anti-ageing and anti-inflammatory properties [54]. It is commercially available in facial serums, and there is some interest in use of topical NAM for treatment of localised photoimmunosuppression, as there has been for oral NAM [13, 56].
Nicotinamide and ophthalmology
NMSC is the most frequent periocular malignancy, and the current evidence supports the theory that oral NAM supplementation may reduce the number of NMSCs developing in a high-risk individual for as long as the individual remains on it. It is also relatively common for patients to have field changes such as diffuse AK that increase their risk of developing NMSC, with some evidence to suggest oral NAM can cause regression, which could theoretically reduce the patient’s longer term risk of developing NMSC, though this has yet to be substantiated. For patients in whom surgical intervention is deemed unsuitable, perhaps due to medical comorbidities, oral NAM may provide a low-risk option to reduce the rate of growth, but should not be used in preference to more established treatment options such as hedgehog inhibitors. In patients at high risk of developing future lesions, such as those with NMSC, with field change, and those who are immunosuppressed, NAM may have a preventative role, though immunosuppressed patients first require more investigation into how to safely manage the dosing to prevent unacceptable side effects. Further work is required to explore these avenues before oral NAM is likely to become integrated into routine practice. However, oral NAM supplementation should be discussed with patients considered at high risk of future lesions so they can make an informed decision as to whether they wish to take it. The potential for isolated use of topical NAM for this purpose, or whether it has additive effects when combined with oral NAM are not yet clear and fall outside the scope of this review. Furthermore, patients deemed to be at high risk for developing NMSC may have chronic sun exposure on large surface areas of their skin and are frequently older patients or those with multiple comorbidities for whom application of topical NAM to a large area is likely to be impractical or unreliable, and oral NAM probably represents the logistically easier option. In patients pursuing supplementation, we would recommend a dose of 500 mg twice daily on the basis of the ONTRAC study regime and ease of administration. If this is not tolerated, topical NAM could be trialled as an alternative.
There is also interest in NAM in other contexts within ophthalmology. It has been shown that there are lower serum levels of NAM in patients with glaucomatous optic neuropathy; some early human RCTs suggest that oral NAM offers neuroprotection, slowing deterioration and possibly enhancing inner retinal ganglion cell function in patients with glaucoma [57,58,59]. Similarly, in-vivo animal models and in-vitro studies using cell lines from human uveal melanomas show anti-angiogenic and anti-inflammatory properties of NAM and suggest it is a viable treatment option [60,61,62]. These areas still require further investigation to elucidate the potential benefits before it could be introduced to routine clinical practice.
Limitations
This is a retrospective review focusing on oral administration of NAM for the purpose of reducing incidence of NMSC. Studies thus far have generally relied on small numbers of patients, or analysis of different subtypes of NMSC as one entity, which has drawn criticism regarding the validity of the studies and questions regarding clinical applicability of the findings.
Conclusion
NAM is an amide form of vitamin B3 available in a variety of common foods, and cheaply available without the need for prescription in the UK. Administered orally, it has a very good side effect profile with minimal symptoms, usually gastrointestinal or headaches, that resolve upon cessation of the drug. It is thought to be safe for use in pregnancy. Smaller doses may be appropriate in patients with hepatic or renal dysfunction, and NAM should be avoided in patients with neurodegenerative disease until more information is available. Oral NAM supplementation does not affect risk of sunburn with UV exposure, but has been shown to reduce UV-induced immunosuppression. NAM is hypothesised to support DNA repair by repleting NAD+ stores required for this energy-dependent process, inhibiting PARP and its effects on glycolysis, and inhibiting sirtuin enzymes which are pro-inflammatory. NAM’s support of DNA repair is theorised to reduce tumorigenesis. Although there has been criticism of one study’s statistical analysis, there remains acknowledgement that NAM is likely to have some effect to reduce the incidence of NMSC. Furthermore, NAM may even support regression of AK, which are precursors to NMSC. However, the effect of NAM appears to disappear upon cessation of the drug. Further high-quality research would be beneficial to elucidate the degree of benefit that can be expected with use of oral NAM. However, until such data is available, NAM represents a cheap and well-tolerated treatment option for patients at high risk of developing future NMSC and clinicians should incorporate this into their discussions with such patients.
References
Mahajan AS, Arikatla VS, Thyagarajan A, Zhelay T, Sahu RP, Kemp MG, et al. Creatine and Nicotinamide Prevent Oxidant-Induced Senescence in Human Fibroblasts. Nutrients. 2021 Nov [cited 2022 Jan 10];13. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8622652/.
Yiasemides E, Sivapirabu G, Halliday GM, Park J, Damian DL. Oral nicotinamide protects against ultraviolet radiation-induced immunosuppression in humans. Carcinogenesis. 2009;30:101–5.
Chen AC, Damian DL. Nicotinamide and the skin: Nicotinamide and the skin. Australas J Dermatol. 2014;55:169–75.
Chen AC, Damian DL, Halliday GM. Oral and systemic photoprotection: Oral and systemic photoprotection. Photodermatol Photoimmunol Photomed. 2014;30:102–11.
Leiter U, Garbe C. Epidemiology of Melanoma and Nonmelanoma Skin Cancer—The Role of Sunlight. In: Reichrath J, editor. Sunlight, Vitamin D and Skin Cancer. New York, NY: Springer New York; 2008 [cited 2021 Oct 28]. 89–103. (Advances in Experimental Medicine and Biology; vol. 624). Available from: http://link.springer.com/10.1007/978-0-387-77574-6_8.
Rene C. Oculoplastic aspects of ocular oncology. Eye 2013;27:199–207.
Damian DL. Photoprotective effects of nicotinamide. Photochem Photobio Sci. 2010;9:578.
Chen AC, Martin A, Damian DL. Nicotinamide for skin-cancer chemoprevention. N. Engl J Med. 2016;374:789–90.
Bostom AG, Merhi B, Walker J, Robinson-Bostom L. More than skin deep? Potential nicotinamide treatment applications in chronic kidney transplant recipients. World J Transpl. 2016;6:658–64.
Minocha R, Damian DL, Halliday GM. Melanoma and nonmelanoma skin cancer chemoprevention: A role for nicotinamide? Photodermatol Photoimmunol Photomed. 2018;34:5–12.
Riklis E, Kol R, Marko R. Trends and developments in radioprotection: the effect of nicotinamide on DNA repair. Int J Radiat Biol. 1990;57:699–708.
Rissiek B, Guse AH, Adriouch S, Bruzzone S. Editorial: the versatile role of nicotinamide adenine dinucleotide in immunity. Front Immunol. 2021;12:810280.
Thanos SM, Halliday GM, Damian DL. Nicotinamide reduces photodynamic therapy-induced immunosuppression in humans: Nicotinamide reduces PDT immunosuppression in humans. Br J Dermatol. 2012;167:631–6.
Surjana D, Halliday GM, Martin AJ, Moloney FJ, Damian DL. Oral nicotinamide reduces actinic keratoses in phase II double-blinded randomized controlled trials. J Invest Dermatol. 2012;132:1497–500.
Green A, Battistutta D. Incidence and determinants of skin cancer in a high-risk australian population. Int J Cancer. 1990;46:356–61.
Chen AC, Martin AJ, Choy B, Fernández-Peñas P, Dalziell RA, McKenzie CA, et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. N. Engl J Med. 2015;373:1618–26.
Gilmore SJ. Nicotinamide and skin cancer chemoprevention: The jury is still out. Australas J Dermatol. 2018;59:6–9.
Gilmore SJ. Response to ‘Considering the chemopreventive potential of nicotinamide in Gilmore’s Bayesian analysis’. Australas J Dermatol. 2018;59:236–7.
Phelan PS. Chemopreventive potential of nicotinamide in Gilmore’s Bayesian analysis. Australas J Dermatol. 2018;59:236–236.
Bagcchi S. Nicotinamide yields impressive results in skin cancer. Lancet Oncol. 2015;16:e591.
Minocha R, Martin AJ, Chen AC, Scolyer RA, Lyons JG, McKenzie CA, et al. A reduction in inflammatory macrophages may contribute to skin cancer chemoprevention by nicotinamide. J Invest Dermatol. 2019;139:467–9.
Pettersen JS, Fuentes-Duculan J, Suárez-Fariñas M, Pierson KC, Pitts-Kiefer A, Fan L, et al. Tumor-associated macrophages in the cutaneous SCC microenvironment are heterogeneously activated. J Invest Dermatol. 2011;131:1322–30.
Chen AC, Martin AJ, Dalziell RA, McKenzie CA, Lowe PM, Eris JM, et al. A phase II randomized controlled trial of nicotinamide for skin cancer chemoprevention in renal transplant recipients. Br J Dermatol. 2016;175:1073–5.
Collins L, Asfour L, Stephany M, Lear JT, Stasko T. Management of non-melanoma skin cancer in transplant recipients. Clin Oncol. 2019;31:779–88.
Yélamos O, Halpern AC, Weinstock MA. Reply to ‘A phase II randomized controlled trial of nicotinamide for skin cancer chemoprevention in renal transplant recipients’. Br J Dermatol. 2017;176:551–2.
Drago F, Ciccarese G, Parodi A. Nicotinamide for skin-cancer chemoprevention. N. Engl J Med. 2016;374:789–90.
Drago F, Ciccarese G, Cogorno L, Calvi C, Marsano LA, Parodi A. Prevention of non-melanoma skin cancers with nicotinamide in transplant recipients: a case-control study. Eur J Dermatol. 2017;27:382–5.
Ferreira ER, Miola AC, Lima TRR, Schmitt JV, Abbade LPF, Miot HA. Efficacy of intermittent topical 5-fluorouracil 5% and oral nicotinamide in the skin field cancerization: a randomized clinical trial. Bras Dermatol. 2021;96:784–7.
Knip M, Douek IF, Moore WPT, Gillmor HA, McLean AEM, Bingley PJ, et al. Safety of high-dose nicotinamide: a review. Diabetologia. 2000;43:1337–45.
Hwang ES, Song SB. Possible adverse effects of high-dose nicotinamide: mechanisms and safety assessment. Biomolecules. 2020;10:687.
Horsman MR, Høyer M, Honess DJ, Dennis IF, Overgaard J. Nicotinamide pharmacokinetics in humans and mice: a comparative assessment and the implications for radiotherapy. Radiother Oncol J Eur Soc Ther Radio Oncol. 1993;27:131–9.
Elliott RB, Pilcher CC, Stewart A, Fergusson D, McGregor MA. The use of nicotinamide in the prevention of type 1 diabetes. Ann N. Y Acad Sci. 1993;696:333–41.
Rolfe HM. A review of nicotinamide: treatment of skin diseases and potential side effects. J Cosmet Dermatol. 2014;13:324–8.
Gale EA. European Nicotinamide Diabetes Intervention Trial (ENDIT): a randomised controlled trial of intervention before the onset of type 1 diabetes. Lancet. 2004;363:925–31.
Elliott RB, Pilcher CC, Fergusson DM, Stewart AW. A Population Based Strategy to Prevent Insulin-Dependent Diabetes Using Nicotinamide. J Pediatr Endocrinol Metab. 1996 Jan [cited 2021 Nov 13];9. Available from: https://www.degruyter.com/document/doi/10.1515/JPEM.1996.9.5.501/html.
Lenglet A, Liabeuf S, El Esper N, Brisset S, Mansour J, Lemaire-Hurtel A-S, et al. Efficacy and safety of nicotinamide in haemodialysis patients: the NICOREN study. Nephrol Dial Transpl Publ Eur Dial Transpl Assoc - Eur Ren Assoc. 2017;32:870–9.
Green S. N-methylation of pyridines in Parkinson’s disease. Lancet. 1991;338:120–1.
Zhao X, Zhang M, Li C, Jiang X, Su Y, Zhang Y. Benefits of vitamins in the treatment of parkinson’s disease. Oxid Med Cell Longev. 2019;2019:9426867.
Alisky JM. Niacin improved rigidity and bradykinesia in a Parkinson’s disease patient but also caused unacceptable nightmares and skin rash—A case report. Nutr Neurosci. 2005;8:327–9.
Martin AJ, Dhillon HM, Vardy JL, Dalziell RA, Choy B, Fernández-Peñas P, et al. Neurocognitive function and quality of life outcomes in the ONTRAC study for skin cancer chemoprevention by nicotinamide. Geriatrics. 2019;4:31.
Zhao Y. Nicotinamide for skin-cancer chemoprevention. N. Engl J Med. 2016;374:789.
Gollins CE, Shah A, Sinha K, Khan S, Paul N, Meeajun B, et al. Feasibility of a trial to evaluate nicotinamide for chemoprevention of skin cancers in organ transplant recipients in the UK. Br J Dermatol. 2020;183:394–6.
Fania L, Sampogna F, Ricci F, Hyeraci M, Paradisi A, Palese E, et al. Systemic photoprotection in skin cancer prevention: knowledge among dermatologists. Biomolecules. 2021;11:332.
Desai S, Olbricht S, Ruiz ES, Hartman RI. Nicotinamide for keratinocyte carcinoma chemoprevention: a nationwide survey of mohs surgeons. Dermatol Surg. 2021 ;47:452–3.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Squamous Cell Cancer. National Comprehensive Cancer Network; 2017 [cited 2021 Dec 14]. Available from: https://oncolife.com.ua/doc/nccn/Squamous_Cell_Skin_Cancer.pdf.
Tee LY, Sultana R, Tam SYC, Oh CC. Chemoprevention of keratinocyte carcinoma and actinic keratosis in solid-organ transplant recipients: Systematic review and meta-analyses. J Am Acad Dermatol. 2021;84:528–30.
Hoegler KM, Khachemoune A. Is the first-line systemic chemoprevention of nonmelanoma skin cancer nicotinamide or acitretin? Int J Dermatol. 2021;60:749–50.
Stratigos AJ, Garbe C, Dessinioti C, Lebbe C, Bataille V, Bastholt L, et al. European interdisciplinary guideline on invasive squamous cell carcinoma of the skin: Part 1. epidemiology, diagnostics and prevention. Eur J Cancer. 2020;128:60–82.
Moscarella E, Di Brizzi EV, Casari A, De Giorgi V, Di Meo N, Fargnoli MC, et al. Italian expert consensus paper on the management of patients with actinic keratoses. Dermatol Ther. 2020 Nov [cited 2021 Oct 24];33. Available from: https://onlinelibrary.wiley.com/doi/10.1111/dth.13992.
Cosio T, Di Prete M, Campione E. Arsenic trioxide, itraconazole, all-trans retinoic acid and nicotinamide: a proof of concept for combined treatments with hedgehog inhibitors in advanced basal cell carcinoma. Biomedicines. 2020;8:156.
Huber R, Wong A. Nicotinamide: An Update and Review of Safety & Differences from Niacin. Skin Ther Lett. 2020 Dec [cited 2021 Oct 24];25. Available from: https://www.skintherapyletter.com/dermatology/nicotinamide-update-niacin/.
Kademian M, Bechtel M, Zirwas M. Case reports: new onset flushing due to unauthorized substitution of niacin for nicotinamide. J Drugs Dermatol. 2007;6:1220–1.
Hosseini B. Vitamin B3 – Not all forms are equivalent! J Pharm Pr Res. 2017;47:79–80.
Snaidr VA, Damian DL, Halliday GM. Nicotinamide for photoprotection and skin cancer chemoprevention: A review of efficacy and safety. Exp Dermatol. 2019;28:15–22.
Ratnarajah K, Zargham H, Jafarian F. Confusion among different forms of vitamin B3. J Cutan Med Surg. 2020;24:642–3.
Gensler HL. Prevention of photoimmunosuppression and photocarcinogenesis by topical nicotinamide. Nutr Cancer. 1997;29:157–62.
Hui F, Tang J, Williams PA, McGuinness MB, Hadoux X, Casson RJ, et al. Improvement in inner retinal function in glaucoma with nicotinamide (vitamin B3) supplementation: A crossover randomized clinical trial. Clin Exp Ophthalmol. 2020;48:903–14.
Tribble JR, Otmani A, Sun S, Ellis SA, Cimaglia G, Vohra R, et al. Nicotinamide provides neuroprotection in glaucoma by protecting against mitochondrial and metabolic dysfunction. Redox Biol. 2021;43:101988.
De Moraes CG, John SWM, Williams PA, Blumberg DM, Cioffi GA, Liebmann JM. Nicotinamide and pyruvate for neuroenhancement in open-angle glaucoma: a phase 2 randomized clinical trial. JAMA Ophthalmol. 2022;140:11–8.
Malesu R, Martin AJ, Lyons JG, Scolyer RA, Chen AC, McKenzie CA, et al. Nicotinamide for skin cancer chemoprevention: effects of nicotinamide on melanoma in vitro and in vivo. Photochem Photobio Sci. 2020;19:171–9.
Scatozza F, Moschella F, D’Arcangelo D, Rossi S, Tabolacci C, Giampietri C, et al. Nicotinamide inhibits melanoma in vitro and in vivo. J Exp Clin Cancer Res. 2020;39:211.
Esposito E, Aldrees S, Mastromonaco C, Zoroquiain P, Vila N, Logan PT, et al. Evaluation of nicotinamide as an anti-inflammatory and anti-angiogenic agent in uveal melanoma cell lines. Arq Bras Oftalmol. 2017;80:74–7.
Author information
Authors and Affiliations
Contributions
RM proposed and devised the scope of the article, critically reviewed and made edits to the article. SH undertook the literature search, wrote the article and made edits. AJ contributed to the literature search and writing of the article, critically reviewed the article and suggested edits.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hunt, S.V., Jamison, A. & Malhotra, R. Oral nicotinamide for non-melanoma skin cancers: A review. Eye 37, 823–829 (2023). https://doi.org/10.1038/s41433-022-02036-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02036-z
This article is cited by
-
Ocular oncology demystified
Eye (2023)
-
NAD(H) homeostasis underlies host protection mediated by glycolytic myeloid cells in tuberculosis
Nature Communications (2023)