Abstract
Objectives
To determine survival outcomes following enucleation for uveal melanoma. To compare these outcomes with the 8th edition AJCC classification and determine the influence of cytogenetics, using Fluorescent in situ Hybridisation (FISH), on survival. To determine whether failure to gain sufficient sample for cytogenetics using Fine Needle Aspiration Biopsy (FNAB) correlates with survival.
Subjects/Methods
All patients undergoing primary enucleation for uveal melanoma at Moorfields Eye Hospital between 2012 and 2015 were included. Clinical, pathological, cytological and survival data were analysed for all patients.
Results
In total, 155 subjects were included. Mean age at enucleation was 65.9 years (SD 14.13). 88 (56.8%) patients died at a mean of three (SD 1.9) years following enucleation. Of these, 52 (33.5%) died from metastatic melanoma, 16 (10.3%) from other causes and 20 (12.9%) causes of death were unknown. Cumulative incidence analysis demonstrated AJCC grade, chromosome 8q gain and monosomy three all predict metastatic mortality. The greatest 5-year mortality rate (62%, SD10.1%) was in those with both chromosome abnormalities and AJCC stage III (Stage IV patients excluded due to low numbers). Largest basal diameter and chromosome status, both independently (p = 0.02 and p < 0.001) predicted metastatic mortality on multivariable regression analysis. Those who had an insufficient sample of cells gained during FNAB (n = 16) had no different prognosis.
Conclusions
This study confirms, in this population, the poor survival of patients enucleated for uveal melanomas. It confirms the prognostic utility of adding AJCC grade to cytogenetic information. It demonstrates that the lack of sample in patients undergoing FNAB is not related to prognosis.
Similar content being viewed by others
Introduction
Uveal melanoma is a relatively rare tumour occurring in 6 per million people per year in England [1]. Metastases develop in almost 50% of patients [2], usually to the liver. The efficacy of current treatments for metastatic uveal melanoma are limited and mortality within the first year is common [2].
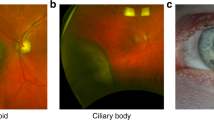
Factors predictive of metastasis are multiple and have been described at length previously [3]. They include: anatomical factors, such as tumour size, extraocular extension and ciliary body involvement; histopathological factors such as the presence of epithelioid cells, closed connective tissue loops and high mitotic count; and genetic aberrations, such as chromosome 3 loss, chromosome 8q gain, BAP1 loss of function mutations and a class 2 gene expression profile.
Patients find it helpful to be given an idea of their life expectancy at the time of diagnosis [4]. Prognostication may enable some practitioners to adjust the intensity of surveillance for metastasis according to each patient’s estimated mortality. The standard prognostic tool is the American Joint Committee on Cancer (AJCC) Tumour Node Metastasis (TNM) classification [5]. This is now in its eighth edition and has been validated and modified from a series of over 7000 uveal melanoma patients provided by the European Ophthalmic Oncology Group [6].
A limitation of the AJCC classification is that it uses only anatomic predictors, without taking into account genetic and histopathological risk factors. Several studies suggest including these laboratory findings, particularly cytogenetic information, can improve the accuracy of prognostication [7,8,9,10]. The Liverpool Uveal Melanoma Prognosticator Online (LUMPO), now in its third iteration, combines anatomic findings with genetic and histopathologic data. An international validation study of LUMPO has validated the use of this prognostic tool in uveal melanoma with data from seven international ocular oncology centres [11].
Moorfields Eye Hospital is one of four Ocular Oncology centres in the UK receiving referrals from a large population in the South of England. Since 2012, we have routinely performed FISH (fluorescence in situ hybridisation) cytogenetic analysis on all consenting patients undergoing primary enucleation for choroidal melanoma.
In this paper, we compare survival outcomes following primary enucleation for choroidal melanoma with the standard 8th edition AJCC classification based on TNM and determine the influence of cytogenetic FISH results, and other known prognostic markers on this cohort of patients. We also sought to investigate whether failure to obtain enough sample for FISH analysis using fine-needle aspiration biopsy (FNAB) indicates a better prognosis as has been suggested previously [12]. In theory, smaller tumours with cohesive spindle cells, indicating better prognosis, may be less likely to yield sufficient cells for cytogenetic analysis.
Methods
This is a single centre case series study. Subjects were identified from the enucleation database of the Department of Pathology, University College London Institute of Ophthalmology. All primary enucleation cases performed by the department between 1 January 2012 and 31 December 2014 were included.
With prior consent from patients, cells for cytogenetic analysis were gained from enucleation specimens following eye removal using trans-scleral fine-needle aspiration biopsy (FNAB). FISH analysis was carried out using centromeric and subtelomeric probes for chromosome 3 (D3S4559, D3Z1, Cytocell Ltd, Cambridge, United Kingdom) and centromeric and MYC probes for chromosome 8 (D8Z2, MYC, Abbott Molecular Inc., Des Plaines, IL, USA). At least 100 cells from each enucleation specimen were evaluated when possible, and abnormalities were reported when more than 10% of cells showed cytogenetic changes.
Clinical records were reviewed for demographic data, including age and sex. Pathology findings were reviewed for data on tumour size, mitotic count, the presence or absence of ciliary body involvement (defined as including the pars plana), epithelioid cells, extravascular matrix loops and extraocular extension.
The United Kingdom National Health Service keeps Summary Care Records for the entire population (The NHS Digital Spine). These Summary Care Records can be accessed digitally by registered health professionals. These records were searched on 13th May 2020 to identify whether patients in this study were alive or dead and the date of death of the deceased. The General Practitioners (family doctors) of all the deceased patients were contacted to find out the cause of death. If the General Practitioners were not able to provide us with this information we attempted to contact next of kin of the deceased patients.
Statistical analysis
For the analysis, the statistical software package R (version 3.6.3) was used (www.r-project.org). Participant characteristics were summarised using percentages, means and standard deviations (SD). Pearson’s chi-squared, Fisher’s exact test and the Kruskal–Wallis test were performed to evaluate the inter-correlations between baseline characteristics.
Missing and non-missing cases were compared using sensitivity analysis to assess the robustness of the missing at random assumption. Schoenfeld’s residuals were plotted against failure time for each covariate to assess the proportional hazards assumption. Violations in the proportional hazard’s assumption were handled via stratification or time-dependent covariate methods. To enhance statistical power and ensure stable model estimation, AJCC stages I and IV were discounted from analyses due to low numbers (n = 1 and n = 7) and also due to relatively low numbers in each subgroup, stages IIA and IIB were grouped to form stage II and stages IIIA, IIIB and IIIC grouped as stage III.
Cumulative incidence functions (CIFs) were plotted to show the estimated marginal probability of each cause of death post treatment accompanied by the numbers at risk. Gray’s test for equality of CIFs was performed to evaluate statistical significance. Cumulative incidence rates (95% CI) of death due to melanoma were computed at five years of follow-up. Largest basal diameter (LBD) and mitotic count were categorised for graphical visualisation; however, when taken forward into the multivariable models these variables remained continuous to increase power and limit loss of information.
Subdistribution-hazard ratios with 95% CI’s were estimated using the Fine and Gray regression model in both univariate and multivariable analysis [13]. For ease of interpretation, additional analyses were performed using the Cox regression model. In this model, effect estimates were reported as hazard ratios (HRs) with 95% CIs.
In the multivariable analyses, a backward stepwise procedure with entry selection criterion set at a nominal p value of 10% and elimination criterion at 5% were employed to select the final model. Forward-selection was also performed with the same entry and stay criterions and models were compared. In both model selection routines, confounders such as age and gender were forced in regardless of statistical significance, unless either variable had a negative effect on the model accuracy. The relative effect of incorporating variables into the model was assessed based on model apparent and bootstrap adjusted C-statistics with 95% CIs, as well as Akaike information criterion (AIC), allowing a rank order of relative importance to be produced. Time-dependent Receiver Operating Characteristic (ROC) and Brier scores were also checked, as per Blanche et al. 2019 [14]. Unadjusted p values are provided unless indicated otherwise.
This study was approved by the Institutional Review Board at Moorfields Eye Hospital (CA20/ONC/606). The study adhered to the tenets of the Declaration of Helsinki.
Results
From 1 January 2012 to 31 December 2014, 159 primary enucleations were performed for uveal melanoma at Moorfields Eye Hospital. There were four patients excluded from the analysis because of the lack of either survival data or pathology/cytopathology results, leaving a total of 155 cases. Table 1 summarises the population characteristics of the cohort. There were 90/155 (58%) males and 65/155 (42%) females. The average age at enucleation was 65.9 years (SD 14.13). 88 (56.8%) patients died at a mean of three (SD 1.9) years following enucleation. 52 (33.5%) patients died from metastatic melanoma, 16 (10.3%) from other causes and 20 (12.9%) causes of death were unknown. The 20 unknown deaths were excluded from further statistical analysis leaving 135 patients in the final sample for analysis. Demographic and tumour characteristics of individuals with known and unknown causes of death were compared and no statistically significant differences were noted (Table S1).
A total of 29.6% of tumours were graded as AJCC stage IIB and 35% as stage IIIA. Tumours missing data on genotype were compared to those where the data was not missing, and no statistically significant differences in demographics or other tumour characteristics were noted (Table S2).
As shown in Table 1, mean age and basal diameter were higher in those who died during the follow-up period (p < 0.001). There was a higher proportion of patients with tumours showing both monosomy 3 (M3) and chromosome 8q gain who died during the study period (p = 0.005 and p = 0.002; chi-squared test). Table 2 shows the p values for the correlations between all tumour characteristics at baseline together with the statistical tests performed to investigate these correlations. AJCC stage and presence of M3 and 8q gain, had a significant association (p = 0.025). AJCC stage and presence of just M3 had a trend towards significance (p = 0.057), whereas there was little to no association with the presence of just chromosome 8q gain (p = 0.209). There was strong evidence for an association between M3 and chromosome 8q gain (p < 0.001).
Cumulative incidence analysis
Cumulative incidence curves are shown in Fig. 1. These demonstrate graphically the prognostic risk factors that statistically significantly predict metastatic mortality (AJCC grade, chromosome 8q gain, monosomy 3, tumour diameter, ciliary body involvement and mitotic rate). For example, Fig. 1B–D show the cumulative incidence curves by presence or absence of chromosome 8q gain and/or monosomy 3 (M3). The presence of 8q gain or M3 is associated with a higher overall incidence in melanoma-related death (p = 0.001; p = 0.002 for chromosome 8q gain and M3 respectively). Taking the respective categories of no M3 or gains in 8q, and both gains in 8q and M3, the incidence of death from melanoma is highest in those who have both aberrations (p < 0.001; Fig. 2D). Table S3 presents the cumulative incidence curve results numerically. The table shows that those with the highest five-year mortality rate (62% SD; 10.1%) are those with both chromosome abnormalities and AJCC stage III.
Curves are plotted for AJCC stage II (Fig. 2A) and III (Fig. 2B) subjects. Plotted on the same graphs are curves for stage II and III patients with monosomy 3 and 8q gain and curves from the European Ophthalmic Oncology group’s 2013 study that formed the basis for the most recent AJCC staging criteria (6).
Cumulative rates of melanoma-related deaths for AJCC stage II and III patients are shown in Fig. 2A and B respectively. These figures, for comparison, have superimposed the cumulative incidence curves from the European Ophthalmic Oncology group’s 2013 study of 7369 patients, the data of which was used to create the 7th edition of the AJCC [6]. To illustrate how adding information about chromosome status to the AJCC data enhances prognostic ability, curves for monosomy 3 and 8q gain patients are also shown.
Shown in Fig. 3 are cumulative incidence curves showing survival in those patients whose FISH failed due to insufficient sample for at least one chromosome (n = 16, 14%) compared to those whose FISH was successful for both chromosomes (n = 99, 86%). No statistically significant difference was noted between these groups.
Regression analysis
Results from the univariate analyses for the Fine and Gray model are shown in table S4. Only baseline demographics (age and gender), mitosis rate, chromosome status, ciliary body involvement and largest basal diameter passed the nominal threshold for inclusion at 10%. Higher AJCC stage (p = 0.007), larger basal diameter (p < 0.001), gain in chromosome 8q (p < 0.001), monosomy 3 (p = 0.003), mitotic rate (p = 0.004), ciliary body involvement (p = 0.014) and higher age (p = 0.011) were found to be associated with melanoma-related death however sex was not associated with metastatic mortality. Univariate cox regression analysis (cause-specific hazards) was in concordance with the results from the Fine–Gray model (table S5), where hazard ratios and 95% CIs are presented for ease of interpretation.
Multivariable analysis limited to chromosome status and largest basal diameter is presented in table S6. We studied the combined variable chromosome status (categorised into two groups- absence of both chromosome abnormalities vs both chromosome abnormalities present) to offset issues related to multicollinearity between the binary variables (p < 0.001; chi2-test). We decided to group the presence of only one chromosomal defect (e.g. M3 or 8q gain) with none due to similar survival experience at five-years in this sample (see Figs. 1 and 2D) and to enhance statistical power for multivariable analysis. Furthermore, because of inadequate sample size in AJCC stage (low numbers in groups other than stage II and III) largest basal diameter was taken forward into the multivariable analysis only.
Residual diagnostic plots for the Fine–Gray model are shown in figures S1-–S4. Calibration curves for the Fine–Gray model are shown in figure S5. As shown in table S7, taking age and gender in a “base” model, adding the largest basal diameter produced better model discrimination than chromosome status; however, taken together these gave the highest AUC (95% CI) (bootstrap adjusted ROC: 72 (67.9,83.7), Time-dependent AUC (AUCt): 77.7 (69.3, 86.2)) and smallest prediction error (Brier score; 16.3 (11.3,21.3)). These two marker-model, despite having more parameters, also had the lowest AIC (281.37). For AIC, smaller values indicate better model fit. Brier score combines discrimination and calibration. Smaller values indicate higher predictive accuracy.
Discussion
This study specifically focuses on survival in patients with large, advanced tumours who have not received previous treatment. The results demonstrate that in our particular population of patients, survival following enucleation for large uveal melanoma is poor. Fifty-seven percent of our cohort of patients enucleated between 2012 and 2014 had died by May 2020. Only 18% of these patients were known to have died from other causes. The remaining 82% either died from metastatic melanoma or had unknown causes of death.
As shown in Fig. 2, our survival results based on AJCC criteria are comparable to the European Ophthalmic Oncology Group’s 2013 study that validated the AJCC criteria [6]. Over and above this, using both cumulative incidence analysis and multivariable regression analysis, we corroborate the findings of previous studies that have demonstrated the utility of combining the additional information from cytogenetics with tumour size/AJCC grade [7,8,9,10]. In our patients, adding information about chromosome status to information about tumour size, more accurately predicts mortality than AJCC data alone (see Fig. 2). Overall, patients with the worst prognosis are those with tumours with a diameter of 16 mm or more with both monosomy of chromosome 3 and chromosome 8q gains. In these patients, the five-year mortality rate measures 61%.
Since 2012, we have routinely performed FISH (fluorescence in situ hybridisation) cytogenetic analysis on all consenting patients undergoing primary enucleation for advanced uveal melanoma. Although several other techniques for genetic analysis exist, with this study we have demonstrated that FISH remains a useful tool. Benefits of FISH over these other methods include the fact that it is able to assess for heterogeneity in tumours and that it can also be used to detect the percentage of cells with monosomy 3 and 8q amplification, which has been shown previously to correlate with patient survival [15]. By using two probes for chromosome 3 (a centromeric and sub-telomeric probe) we are able to detect partial deletions of chromosome 3, which used to be a weakness of FISH as compared to MLPA. We demonstrate that tumours providing insufficient sample for FISH analysis have a similar prognosis to those who have successful FISH, although the numbers involved are small (n = 16). This result is in contrast to previous theories that insufficient-sample FNAB results are more likely in more cohesive, spindle-cell tumours that are smaller and have a better overall prognosis [12].
The strengths and challenges of this study included the ascertainment of survival data on a cohort of enucleated patients with advanced uveal melanoma, all of whom had been discharged from routine Ocular Oncology follow-up but still attended other hospitals for surveillance scans of the liver. Although we had robust data on whether patients were alive or deceased from the NHS Digital Spine, obtaining the cause of death data was more difficult. This meant that 20/88, 22% of patients had unknown causes of death. National collection of survival data for uveal melanoma in the United Kingdom is flawed because, in central registries, it is coded as head and neck cancer rather than eye cancer.
Chromosome 8 status was known only in 104/155 (67%), and chromosome 3 status only in 100/155 (64%). Despite this, we have used robust statistical methods to ensure that the conclusions we have drawn from the study are valid. The main reasons for lack of cytogenetic information in patients were because patients declined the test or the cytogenetic test failed due to insufficient material (16 samples). Performing cytogenetic testing on all patients is a possible way of increasing the amount of cytogenetic information available for further studies. Rather than a fine needle aspirate, a scleral flap approach or punch biopsy may permit a greater yield. Newer molecular techniques may also yield better results. Next-generation sequencing (NGS) in choroidal melanoma analysis [16], may provide further avenues of research as to whether NGS provides the same, or better ability to add to AJCC prognostic ability as FISH. In this study, we relied on pathology measurements of tumour size due to inconsistencies in the reporting of ultrasound and clinical measurements. It should be acknowledged that pathology measurements, depending on where the globe is cut, can provide inaccurate measurements in some cases. This, however, is the same with both ultrasound and clinical measurements, which also include an element of subjectivity and can vary between operators.
In conclusion, this study will help patients and ocular oncology practitioners in the future with prognostication as it has confirmed in our population the results of previous studies demonstrating poor survival in patients enucleated for large uveal melanomas. It has also confirmed results from previous studies that have demonstrated the utility of adding AJCC grade to cytogenetic information in producing more accurate prognostication. In addition, it demonstrates that FISH remains a useful tool and that lack of samples in patients undergoing FNAB is not related to prognosis.
Summary
What was known before
-
AJCC grading can be a helpful tool in prognostication of uveal melanoma. Cytogenetic information can also be a helpful tool in prognostication. Failure to obtain a FNAB sample for cytogenetic testing may correlate with survival.
What this study adds
-
In the large, diverse population studied, AJCC grading is relevant and can help patients understand their prognosis. Cytogenetic information obtained using FISH analysis adds to the prognostic information gained from AJCC grading. Failure to obtain a FNAB sample for cytogenetic testing does not correlate with survival in this population. Patients undergoing primary enucleation for uveal melanoma tend to have large tumours and their prognosis is often poor.
References
Keenan TDL, Yeates D, Goldacre MJ. Uveal melanoma in england: trends over time and geographical variation. Br J Ophthalmol. 2012;96:1415–9.
Jager MJ, Shields CL, Cebulla CM, Abdel-Rahman MH, Grossniklaus HE, Stern MH, et al. Uveal melanoma. Nat Rev. 2020;6:1–25.
Damato B, Eleuteri A, Hussain R, Kalirai H, Thornton S, Taktak A, et al. Parsimonious models for predicting mortality from choroidal melanoma. Invest Ophthalmol Vis Sci. 2020;61:35. 9
Beran TM, McCannel TA, Stanton AL, Straatsma BR, Burgess BL. Reactions to and desire for prognostic testing in choroidal melanoma patients. J Genet Couns. 2009;18:265–74.
Amin MB, Edge S, Greene F, et al. eds. AJCC Cancer Staging Manual. 8th ed. Cham, Switzerland: Springer; 2017. p. 813–26.
Kujala E, Damato B, Coupland SE, Desjardins L, Bechrakis NE, Grange JD, et al. Staging of ciliary body and choroidal melanomas based on anatomic extent. J Clin Oncol. 2013;31:2825–31.
Dogrusöz M, Bagger M, van Duinen SG, Kroes WG, Ruivenkamp CA, Böhringer S, et al. The prognostic value of AJCC staging in uveal melanoma is enhanced by adding chromosome 3 and 8q status. Invest Ophthalmol Vis Sci. 2017;58:833–42.
Damato B, Duke C, Coupland SE, Hiscott P, Smith PA, Campbell I, et al. Cytogenetics of uveal melanoma: a 7-year clinical experience. Ophthalmology. 2007;114:1925–31.
Bagger M, Andersen MT, Andersen KK, Heegaard S, Andersen MK, Kiilgaard JF. The prognostic effect of American Joint Committee on Cancer staging and genetic status in patients with choroidal and ciliary body melanoma. Invest Ophthalmol Vis Sci. 2014;56:438–44.
Walter SD, Chao DL, Feuer W, Schiffman J, Char DH, Harbour JW. Prognostic implications of tumor diameter in association with gene expression profile for uveal melanoma. JAMA Ophthalmol. 2016;134:734–40.
Cunha Rola A, Taktak A, Eleuteri A, Kalirai H, Heimann H, Hussain R, et al. Multicenter external validation of the liverpool uveal melanoma prognosticator online: an OOG collaborative study. Cancers (Basel). 2020;12:477.
Augsburger JJ, Corrêa ZM, Trichopoulos N. Prognostic implications of cytopathologic classification of melanocytic uveal tumors evaluated by fine-needle aspiration biopsy. Arq Bras Oftalmol. 2013;76:72–9.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Blanche P, Kattan MW, Gerds TA. The c-index is not proper for the evaluation of $t$-year predicted risks. Biostatistics. 2019;20:347–57.
van den Bosch T, van Beek JG, Vaarwater J, Verdijk RM, Naus NC, Paridaens D, et al. Higher percentage of FISH-determined monosomy 3 and 8q amplification in uveal melanoma cells relate to poor patient prognosis. Invest Ophthalmol Vis Sci. 2012;53:2668–74.
Afshar AR, Damato BE, Stewart JM, Zablotska LB, Roy R, Olshen AB, et al. Next-generation sequencing of uveal melanoma for detection of genetic alterations predicting metastasis. Transl Vis Sci Technol. 2019;8:18.
Acknowledgements
We would like to acknowledge the significant contribution that Victoria Cohen made to this paper before her tragic death in December 2020.
Funding
SS and SG were funded by Global Challenges Research Fund and UK Research and Innovation through the Medical Research Council grant number MR/P027881/1.
Author information
Authors and Affiliations
Contributions
All the authors made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. All the authors were involved in drafting the work or revising it critically for important intellectual content. All the authors were involved in the final approval of the version to be published. All the authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Negretti, G.S., Gurudas, S., Gallo, B. et al. Survival analysis following enucleation for uveal melanoma. Eye 36, 1669–1674 (2022). https://doi.org/10.1038/s41433-021-01710-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01710-y