Abstract
Background/objectives
In Africa, approximately two-thirds of patients are at risk of malnutrition on admission and the nutritional status of patients deteriorates during hospitalization, with associated increased morbidity, mortality, and hospital-related cost. This cross-sectional study aimed at estimating rates of malnutrition in critical care units and determining the extent to which malnutrition diagnoses are documented in medical records by physicians, at two public tertiary hospitals in Malawi.
Methods
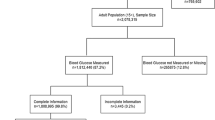
A total of 315 adult (n = 112) and paediatric (n = 203) participants from Queen Elizabeth Central Hospital and Kamuzu Central Hospital, were included in the analysis. Nutrition status was measured by Subjective Global Assessment (SGA) and Mid-Upper Arm circumference (MUAC) and medical notes were reviewed, in both adults and paediatrics.
Results
In adults, more than half were malnourished, with a higher proportion considered moderately-to-severely malnourished using SGA compared to MUAC (84.8%; 57.3%, respectively). Likewise, in paediatrics, a higher proportion was considered moderately-to-severely malnourished using SGA compared to MUAC (84.7%; 23.4%, respectively). Both adult and paediatric patients with cancer had the highest rates of malnutrition. Only 12.9% and 9.6% had documentation of malnutrition diagnosis in the medical record, for paediatrics and adult patients, respectively.
Conclusion
The high rates of hospital malnutrition in critically ill patients in Malawi call for comprehensive screening practices and methods; complemented by documentation of the malnutrition diagnosis and use of nutrition interventions by dietitians. This includes enteral, parenteral and supplemental nutrition as a prerequisite for patient recovery in hospitals.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Russell CA. The impact of malnutrition on healthcare costs and economic considerations for the use of oral nutritional supplements. Clin Nutr. 2007;2:25–32.
Khalatbari-Soltani S, Marques-Vidal P. The economic cost of hospital malnutrition in Europe; a narrative review. Clin Nutr ESPEN [Internet]. 2015;10:e89–94. https://doi.org/10.1016/j.clnesp.2015.04.003.
Correia MITD, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22:235–9.
León-Sanz M, Brosa M, Planas M, García-de-Lorenzo A, Celaya-Pérez S, Hernández JÁ, et al. PREDyCES study: The cost of hospital malnutrition in Spain. Nutrition 2015;31:1096–102.
Correia MITD, Campos ACL. Prevalence of hospital malnutrition in Latin America: the multicenter ELAN study. Nutrition 2003;19:823–5.
Blaauw R, Dolman R, Munyi F, Nyatefe D, Visser J The problem of hospital malnutrition in the African continent. Nutrients. 2019;11:15–8.
Lew CCH, Yandell R, Fraser RJL, Chua AP, Chong MFF, Miller M. Association between malnutrition and clinical outcomes in the intensive care unit: a systematic review. J Parenter Enter Nutr. 2017;41:744–58.
Osooli F, Abbas S, Farsaei S, Adibi P. Identifying critically Ill patients at risk of malnutrition and underfeeding: a prospective study at an academic hospital. Adv Pharm Bull [Internet]. 2019;9:314–20. https://apb.tbzmed.ac.ir.
Delgado AF, Okay TS, Leone C, Nichols B, Del Negro GM, Costa Vaz FA. Hospital malnutrition and inflammatory response in critically ill children and adolescents admitted to a tertiary intensive care unit. Clinics. 2008;63:357–62.
Chimera B, Potani I, Daniel AI, Chatenga H. Clinical nutrition care challenges in low-resource settings during the COVID-19 pandemic: a focus on Malawi. J Glob Health. 2020;10:020363.
Barcus GC, Papathakis PC, Schaffner A, Chimera B. Nutrition screening, reported dietary intake, hospital foods, and malnutrition in critical care patients in Malawi. Nutrients [Internet]. 2021;13:1170. https://doi.org/10.3390/nu13041170.
Blunt SB, Kafatos A. Clinical nutrition education of doctors and medical students: solving the Catch 22. Adv Nutr. 2019;10:345–50.
Higgins PA, Daly BJ, Lipson AR, Su-Er G. Assessing nutritional status in chronically critically Ill adult patients. Am J Crit Care [Internet]. 2006;15:166–77. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3336201/pdf/nihms9218.pdf..
Global Nutrition Report Stakeholder Group. Global nutrition report 2017: nourishing the SDGs [Internet]. Development Initiatives. Bristol,UK; 2017 [cited 2021 Jun 27]. https://globalnutritionreport.org/reports/2017-global-nutrition-report/
Reber E, Gomes F, Vasiloglou MF, Schuetz P, Stanga Z. Nutritional risk screening and assessment. J Clin Med. 2019;8:1065.
Miyoba N, Musowoya J, Mwanza E, Malama A, Murambiwa N, Ogada I, et al. Nutritional risk and associated factors of adult in-patients at a teaching hospital in the Copperbelt province in Zambia; A hospital-based cross-sectional study. BMC Nutr. 2018;4:1–6.
Binns PJ, Dale NM, Banda T, Banda C, Shaba B, Myatt M. Safety and practicability of using mid-upper arm circumference as a discharge criterion in community based management of severe acute malnutrition in children aged 6 to 59 months programmes. Arch Public Heal [Internet]. 2016;74:1–11. https://doi.org/10.1186/s13690-016-0136-x.
Bisai S, Bose K. Undernutrition in the Kora Mudi Tribal Population, West Bengal, India: a comparison of body mass index and mid-upper-arm circumference. Food Nutr Bull. 2009;30:63–7. https://doi.org/10.1177/156482650903000106.
Van Tonder V, Mace L, Steenkamp L, ydeman-Edwards R, Gerber K, Friskin D. Mid-upper arm circumference (MUAC) as a feasible tool in detecting adult malnutrition. South African. J Clin Nutr [Internet]. 2018;32:93–8. https://doi.org/10.1080/16070658.2018.1484622.
Tang AM, Chung M, Dong KR, Bahwere P, Bose K, Chakraborty R, et al. Determining a global mid-upper arm circumference cut-off to assess underweight in adults (men and non-pregnant women). Public Health Nutr. 2020;23:3104–13.
World Health Organization. WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: A Joint Statement by the World Health Organization and the United Nations Children’s Fund. Geneva: World Health Organization; 2009. Available from: [Internet]. 2009. https://www.ncbi.nlm.nih.gov/books/NBK200775/
Luma HN, Eloumou SAFB, Mboligong FN, Temfack E, Donfack OT, Doualla MS. Malnutrition in patients admitted to the medical wards of the Douala General Hospital: A cross-sectional study. BMC Res Notes. 2017;10:1–6.
Paakkari L, Okan O. COVID-19: health literacy is an underestimated problem. Lancet Public Heal [Internet]. 2020;5:e249–50. https://doi.org/10.1016/S2468-2667(20)30086-4.
Niyongabo T, Henzel D, Ndayishimyie JM, Melchior JC, Ndayiragije A, Ndihokubwayo JB, et al. Nutritional status of adult inpatients in Bujumbura, Burundi (impact of HIV infection). Eur J Clin Nutr. 1999;53:579–82.
Hébuterne X, Lemarié E, Michallet M, De Montreuil CB, Schneider SM, Goldwasser F. Prevalence of malnutrition and current use of nutrition support in patients with cancer. J Parenter Enter Nutr. 2014;38:196–204.
Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Maeda S, Haraguchi N, et al. Prevalence of Malnutrition Among Gastric Cancer Patients Undergoing Gastrectomy and Optimal Preoperative Nutritional Support for Preventing Surgical Site Infections. Ann Surg Oncol. 2015;22:778–85.
Kaduka LU, Bukania ZN, Opanga Y, Mutisya R, Korir A, Thuita V, et al. Malnutrition and cachexia among cancer out-patients in Nairobi, Kenya. J Nutr Sci. 2017;6:1–10.
Iroh Tam P-Y, Wiens OM, Kabakyenga J, Kiwanuka J, Kumbakumba E, Moschovis PP. Pneumonia in HIV-exposed and Infected Children and Association With Malnutrition. Pediatr Infect Dis J. 2018;37:1011–3.
De Vita MV, Scolfaro C, Santini B, Lezo A, Gobbi F, Buonfrate D, et al. Malnutrition, morbidity and infection in the informal settlements of Nairobi, Kenya: An epidemiological study. Ital J Pediatr. 2019;45:1–11.
Mills RM, Seager E, Harris CA, Hiwa TN, Blackstock SJ, Pumphrey J, et al. The causes of paediatric inpatient deaths in malawi. Arch Dis Child [Internet] 2017;102:A126 LP–A126. http://adc.bmj.com/content/102/Suppl_1/A126.2.abstract.
Allain TJ, Aston S, Mapurisa G, Ganiza TN, Banda NP, Sakala S, et al. Age related patterns of disease and mortality in hospitalised adults in Malawi. PLoS One. 2017;12:1–13.
Planas M, Audivert S, Pérez-Portabella C, Burgos R, Puiggrós C, Casanelles JM, et al. Nutritional status among adult patients admitted to an university-affiliated hospital in Spain at the time of genoma. Clin Nutr. 2004;23:1016–24.
Bakshi N, Singh K Nutrition assessment in patients undergoing liver transplant. Indian J Crit Care Med [Internet]. 2014;18. www.ijccm.org.
Håkonsen SJ, Pedersen PU, Bath-Hextall F, Kirkpatrick P. Diagnostic test accuracy of nutritional tools used to identify undernutrition in patients with colorectal cancer: a systematic review. JBI Database Syst Rev Implement Rep. [Internet] 2015;13:141–87. https://journals.lww.com/jbisrir/Abstract/2015/13040/Diagnostic_test_accuracy_of_nutritional_tools_used.12.aspx.
Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr. 2008;27:5–15.
Mowé M, Bøhmer T. The prevalence of undiagnosed protein‐calorie undernutrition in a population of hospitalized elderly patients. J Am Geriatr Soc. 1991;39:1089–92.
Bunyani A, Mtimuni B, Kalimbira A, Kamalo P. Experiences of health professionals with nutritional support of critically ill patients in tertiary hospitals in Malawi. Malawi Med J [Internet]. 2015;27:1–4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4478396/.
Ministry of Health (MOH). Guidelines for Community-Based Management of Acute Malnutrition. Lilongwe Malawi; 2016.
Rupert AA, Seres DS, Li J, Faye AS, Jin Z, Freedberg DE. Factors associated with delayed enteral nutrition in the intensive care unit: a propensity score–matched retrospective cohort study. Am J Clin Nutr. 2021;1:295–302.
Souza TT, Sturion CJ, Faintuch J. Is the skeleton still in the hospital closet? A review of hospital malnutrition emphasizing health economic aspects. Clin Nutr [Internet]. 2015;34:1088–92. https://doi.org/10.1016/j.clnu.2015.02.008.
Acknowledgements
We would like to thank Ulemu Luwinga, Oswin Kamangira, Chipi Dannayo, Limbikira Wasambo, Takondwa Limbe, and Joseph Mulekano, for their assistance with screening of hospitalized patients.
Funding
This research was funded by the 2019 Wimpfheimer-Guggenheim Fund for International Exchange in Nutrition, Dietetics, and Management Award; Academy of Nutrition and Dietetics.
Author information
Authors and Affiliations
Contributions
BC- Conceived and designed the study, performed study, wrote paper; GB- Analysed data and wrote paper; AS-Analysed data and wrote paper; PP- Designed and performed study and wrote paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chimera-Khombe, B., Barcus, G., Schaffner, A. et al. High prevalence, low identification and screening tools of hospital malnutrition in critically- ill patients in Malawi. Eur J Clin Nutr 76, 1158–1164 (2022). https://doi.org/10.1038/s41430-022-01087-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01087-5