Abstract
Introduction NHS dental treatment for pregnant and nursing mothers with children aged less than 1 year is free for the patient. The rationale being women during this time are more susceptible to dental disease. By providing this free service it is hoped that access rates will increase by removing barriers in inequality and therefore reducing dental disease prevalence.
Aim Identify variations in the uptake of free NHS dental treatment by nursing mothers during pregnancy across different local authorities in England and investigate possible factors linked to this variation.
Methodology Public Health NHS Business Services Authority (BSA) data on mothers' exemption forms was compared to a three-year average from Office for National Statistics (ONS) birth data in 2016, 2017 and 2018; the percentage uptake of free dental care for nursing mothers was derived for lower tier local authorities (LTLAs) in England. Using Local Health (Public Health England) mapping data, this was compared to markers of deprivation and other indices to illustrate poor areas of uptake.
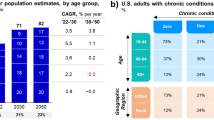
Results The proportion of mothers accessing dental care ranged from 28-61%. Correlations between access and socioeconomic and ethnic backgrounds within local authorities are illustrated.
Conclusion The general low uptake of free dental services among nursing mothers shows more can be done to improve access for this vulnerable group.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
NHS. Who is entitled to free NHS dental treatment in England? 2017. Available from: https://www.nhs.uk/commonhealthquestions/dental-health/whoisentitledtofreenhsdentaltreatmentin-england/ (accessed March 2020).
Rivett G. From Cradle to Grave: The History of the NHS 1988 onwards Second Part. London: Blurb, 2017.
Petersen P E. Global policy for improvement of oral health in the 21st century - implications to oral health research of World Health Assembly 2007, World Health Organisation. Community Dent Oral Epidemiol 2009; 37: 1-8.
Clifford H, Johnson N W, Brown C, Battistutta D. When can oral health education begin? Relative effectiveness of three oral health education strategies starting pre-partum. Community Dent Health 2012; 29: 162-167.
Tickle M. Revolution in the provision of dental services in the UK. Community Dent Oral Epidemiol 2012; DOI: 10.1111/j.1600-0528.2012.00729.x.
Gomez S S, Weber A A. Effectiveness of a caries preventive programme in pregnant women and new mothers on their offspring. Int J Paediatr Dent 2001; 11: 117-122.
Zanata R L, Navarro M F, Pereira J C, Franco E B, Lauris J R P, Barbosa S H. Effect of caries preventive measures directed to expectant mothers on caries experience in their children. Braz Dent J 2003; 14: 75-81.
Medeiros P B V, Otero S A M, Frencken J E, Bronkhorst E M, Leal S C. Effectiveness of an oral health programme for mothers and their infants. Int J Paediatr Dent 2015; 25: 29-34.
Acharya S, Bhat P V. Oralhealthrelated quality of life during pregnancy. J Public Health Dent 2009; 69: 74-77.
Zachariasen R D. Pregnancy gingivitis. J Gt Houst Dent Soc 1997; 69: 10-12.
Laine M A. Effect of pregnancy on periodontal and dental health. Acta Odontol Scand 2002; 60: 257-264.
Priyamvara A, Dey A K, Bagchi A, Kelkar R, Sharma R. Importance of Oral Health in Pregnancy: A Mini-symposium. Current Women Health Rev 2019; DOI: 10.2174/1573404815666190107095920.
Marchi K S, Fisher-Owens S A, Weintraub J A, Yu Z, Braveman P A. Most pregnant women in California do not receive dental care: Findings from a population-based study. Public Health Rep 2010; 125: 831-842.
Boggess K A, Urlaub D M, Massey K E, Moos M K, Matheson M B, Lorenz C. Oral hygiene practices and dental service utilization among pregnant women: An in vitro study. J Am Dent Assoc 2010; 141: 553-561.
Xiong X, Buekens P, Fraser W D, Beck J, Offenbacher S. Periodontal disease and adverse pregnancy outcomes: A systematic review. BJOG 2006; 113: 135-143.
Public Health England. Fingertips: Technical Guidance. Available online at https://fingertips.phe.org.uk/profile/guidance (accessed September 2019).
Department for Communities and Local Government. The English Indices of Deprivation 2015. 2015. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/465791/English_Indices_of_Deprivation_2015_-_Statistical_Release.pdf (accessed May 2020).
Public Health England. Public Health Profiles. Available online at https://fingertips.phe.org.uk (accessed May 2020).
Coleman J S M. Spearman Rank Order Correlation. In Salkind N J (ed) Encyclopaedia of Research Design. California: Sage Publications, 2010: 1405-1408.
Office for National Statistics. Birth Characteristics. Available online at https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/datasets/birthcharacteristicsinenglandandwales (accessed September 2012).
Tudor Hart J. The inverse care law. Lancet 1971; 297: 405-412.
Schneider E C, Sarnak D O, Squires D, Shah A, Doty M M. Mirror, Mirror 2017: International Comparison Reflects Flaws and Opportunities for Better U S. Health Care. 2017. Available at https://interactives.commonwealthfund.org/2017/july/mirror-mirror/assets/Schneider_mirror_mirror_2017.pdf (accessed May 2020).
Dental Public Health Intelligence Team. National Dental Epidemiology Programme for England: oral health survey of fiveyearold children 2017: A report on the inequalities found in prevalence and severity of dental decay. 2018. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/768368/NDEP_for_England_OH_Survey_5yr_2017_Report.pdf (accessed May 2020).
Hullah E, Turok Y, Nauta M, Yoong W. Self-reported oral hygiene habits, dental attendance and attitudes to dentistry during pregnancy in a sample of immigrant women in North London. Arch Gynecol Obstet 2008; 277: 405-409.
Locker D. Deprivation and oral health: A review. Community Dent Oral Epidemiol 2000; 28: 161-169.
Jamieson L M, Thomson W M. Adult oral health inequalities described using area-based and household-based socioeconomic status measures. J Public Health Dent 2006; 66: 104-109.
Riley J L, Gilbert G H, Heft M W. Dental attitudes: Proximal basis for oral health disparities in adults. Community Dent Oral Epidemiol 2006; 34: 289-298.
Armfield J M, Spencer A J, Stewart J F. Dental fear in Australia: Who's afraid of the dentist? Aust Dent J 2006; 51: 78-85.
Hwang S S, Smith V C, McCormick M C, Barfield W D. Racial/ethnic disparities in maternal oral health experiences in 10 states, pregnancy risk assessment monitoring system, 2004-2006. Matern Child Health J 2011; 15: 722-729.
Smaje C, Le Grand J. Ethnicity, equity and the use of health services in the British NHS. Soc Sci Med 1997; 45: 485-496.
Szczepura A. Access to health care for ethnic minority populations. Postgrad Med J 2005; 81: 141-147.
National Research Council and Institute of Medicine. Improving access to oral health care for vulnerable and underserved populations. 2011. Available at https://www.nap.edu/resource/13116/oralhealthaccess2011reportbrief.pdf (accessed May 2020).
Public Health England. Local Health [Internet]. Available from: https://www.localhealth.org.uk/#c=home (accessed May 2020).
Acknowledgements
We are very grateful to the North East Knowledge and Intelligence and Newcastle University for their help with statistical analysis. Thanks to Richard Holmes for peer-reviewing the paper. The views expressed throughout are those of the authors and not necessarily those of Public Health England or the National Health Service.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Webster, J., Landes, D. Evaluation of NHS dental uptake by nursing mothers for local authorities throughout England in 2016-2018. Br Dent J 229, 47–51 (2020). https://doi.org/10.1038/s41415-020-1703-7
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-020-1703-7