Abstract
Study design
A retrospective study.
Objective
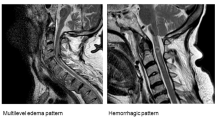
Traumatic cervical spinal cord injury (TSCI) is often associated with disc rupture. It was reported that high signal of disc and anterior longitudinal ligament (ALL) rupture on magnetic resonance imaging (MRI) were the typical signs of ruptured disc. However, for TSCI with no fracture or dislocation, there is still difficult to diagnose disc rupture. The purpose of this study was to investigate the diagnostic efficiency and localization method of different MRI features for cervical disc rupture in patient with TSCI but no any signs of fracture or dislocation.
Setting
Affiliated hospital of University in Nanchang, China.
Methods
Patients who had TSCI and underwent anterior cervical surgery between June 2016 and December 2021 in our hospital were included. All patients received X-ray, CT scan, and MRI examinations before surgery. MRI findings such as prevertebral hematoma, high-signal SCI, high-signal posterior ligamentous complex (PLC), were recorded. The correlation between preoperative MRI features and intraoperative findings was analyzed. Also, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of these MRI features in diagnosing the disc rupture were calculated.
Results
A total of 140 consecutive patients, 120 males and 20 females with an average age of 53 years were included in this study. Of these patients, 98 (134 cervical discs) were intraoperatively confirmed with cervical disc rupture, but 59.1% (58 patients) of them had no definite evidence of an injured disc on preoperative MRI (high-signal disc or ALL rupture signal). For these patients, the high-signal PLC on preoperative MRI had the highest diagnostic rate for disc rupture based on intraoperative findings, with a sensitivity of 97%, specificity of 72%, PPV of 84% and NPV of 93%. Combined high-signal SCI with high-signal PLC had higher specificity (97%) and PPV (98%), and a lower FPR (3%) and FNR (9%) for the diagnosis of disc rupture. And combination of three MRI features (prevertebral hematoma, high-signal SCI and PLC) had the highest accuracy in diagnosing traumatic disc rupture. For the localization of the ruptured disc, the level of the high-signal SCI had the highest consistency with the segment of the ruptured disc.
Conclusion
MRI features, such as prevertebral hematoma, high-signal SCI and PLC, demonstrated high sensitivities for diagnosing cervical disc rupture. High-signal SCI on preoperative MRI could be used to locate the segment of ruptured disc.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Rozzelle CJ, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Ryken TC, et al. Spinal cord injury without radiographic abnormality (SCIWORA). Neurosurgery. 2013;72:227–33.
Hasler RM, Exadaktylos AK, Bouamra O, Benneker LM, Clancy M, Sieber R, et al. Epidemiology and predictors of spinal injury in adult major trauma patients: European cohort study. Eur Spine J. 2011;20:2174–80.
Taylor AR, Blackwood W. Paraplegia in hyperextension cervical injuries with normal radiographic appearances. J Bone Jt Surg Br. 1948;30B:245–8.
Davis SJ, Teresi LM, Bradley WG Jr., Ziemba MA, Bloze AE. Cervical spine hyperextension injuries: MR findings. Radiology. 1991;180:245–51.
Macnab I. Acceleration Injuries of the Cervical Spine. J Bone Jt Surg Am. 1964;46:1797–9.
Goradia D, Linnau KF, Cohen WA, Mirza S, Hallam DK, Blackmore CC. Correlation of MR imaging findings with intraoperative findings after cervical spine trauma. AJNR Am J Neuroradiol. 2007;28:209–15.
Saifuddin A, Green R, White J. Magnetic resonance imaging of the cervical ligaments in the absence of trauma. Spine (Philos Pa 1976). 2003;28:1686–91.
Quinn JC, Kiely PD, Lebl DR, Hughes AP. Anterior surgical treatment of cervical spondylotic myelopathy: review article. HSS J. 2015;11:15–25.
Vaccaro AR, Madigan L, Schweitzer ME, Flanders AE, Hilibrand AS, Albert TJ. Magnetic resonance imaging analysis of soft tissue disruption after flexion-distraction injuries of the subaxial cervical spine. Spine (Philos Pa 1976). 2001;26:1866–72.
Tator CH. Strategies for recovery and regeneration after brain and spinal cord injury. Inj Prev. 2002;8:IV33–6.
Burke DA, Linden RD, Zhang YP, Maiste AC, Shields CB. Incidence rates and populations at risk for spinal cord injury: A regional study. Spinal Cord. 2001;39:274–8.
Brightman RP, Miller CA, Rea GL, Chakeres DW, Hunt WE. Magnetic resonance imaging of trauma to the thoracic and lumbar spine. The importance of the posterior longitudinal ligament. Spine (Philos Pa 1976). 1992;17:541–50.
Flanders AE, Tartaglino LM, Friedman DP, Aquilone LF. Magnetic resonance imaging in acute spinal injury. Semin Roentgenol. 1992;27:271–98.
Hall AJ, Wagle VG, Raycroft J, Goldman RL, Butler AR. Magnetic resonance imaging in cervical spine trauma. J Trauma. 1993;34:21–6.
Keiper MD, Zimmerman RA, Bilaniuk LT. MRI in the assessment of the supportive soft tissues of the cervical spine in acute trauma in children. Neuroradiology. 1998;40:359–63.
Silberstein M, Tress BM, Hennessy O. Prevertebral swelling in cervical spine injury: identification of ligament injury with magnetic resonance imaging. Clin Radio. 1992;46:318–23.
Tehranzadeh J, Kerr R, Amster J. Magnetic resonance imaging of tendon and ligament abnormalities: Part I. Spine and upper extremities. Skelet Radio. 1992;21:1–9.
Kim TH, Kim DH, Kim KH, Kwak YS, Kwak SG, Choi MK. Can the Zero-profile implant be used for anterior cervical discectomy and fusion in traumatic subaxial disc injury? A preliminary, retrospective study. J Korean Neurosurg Soc. 2018;61:574–81.
Maeda T, Ueta T, Mori E, Yugue I, Kawano O, Takao T, et al. Soft-tissue damage and segmental instability in adult patients with cervical spinal cord injury without major bone injury. Spine (Philos Pa 1976). 2012;37:E1560–6.
Malham GM, Ackland HM, Varma DK, Williamson OD. Traumatic cervical discoligamentous injuries: Correlation of magnetic resonance imaging and operative findings. Spine (Philos Pa 1976). 2009;34:2754–9.
Zhuge W, Ben-Galim P, Hipp JA, Reitman CA. Efficacy of MRI for assessment of spinal trauma: Correlation with intraoperative findings. J Spinal Disord Tech. 2015;28:147–51.
Jackson AB, Dijkers M, Devivo MJ, Poczatek RB. A demographic profile of new traumatic spinal cord injuries: Change and stability over 30 years. Arch Phys Med Rehabil. 2004;85:1740–8.
Bernhard M, Gries A, Kremer P, Bottiger BW. Spinal cord injury (SCI)-prehospital management. Resuscitation. 2005;66:127–39.
Spinal cord injury facts and figures at a glance. J Spinal Cord Med. 2013;36:568–9 https://doi.org/10.1179/1079026813Z.000000000209.
Henninger B, Kaser V, Ostermann S, Spicher A, Zegg M, Schmid R, et al. Cervical disc and ligamentous injury in hyperextension trauma: MRI and intraoperative correlation. J Neuroimaging. 2020;30:104–9.
Prasad SS, O’Malley M, Caplan M, Shackleford IM, Pydisetty RK. MRI measurements of the cervical spine and their correlation to Pavlov’s ratio. Spine (Philos Pa 1976). 2003;28:1263–8.
Aebli N, Ruegg TB, Wicki AG, Petrou N, Krebs J. Predicting the risk and severity of acute spinal cord injury after a minor trauma to the cervical spine. Spine J. 2013;13:597–604.
Takao T, Okada S, Morishita Y, Maeda T, Kubota K, Ideta R, et al. Clinical influence of cervical spinal canal stenosis on neurological outcome after traumatic cervical spinal cord injury without major fracture or dislocation. Asian Spine J. 2016;10:536–42.
Penning L. Prevertebral hematoma in cervical spine injury: Incidence and etiologic significance. AJR Am J Roentgenol. 1981;136:553–61.
Funding
This work is supported by the Department of Science and Technology Program of Jiangxi Province, China (No. 20223BBG71S02, 20203BBG73045), and Jiangxi Province “Double Thousand Plan” Talent Project.
Author information
Authors and Affiliations
Contributions
J-ML, Z-LL, and S-HH contributed to the study’s conception and design. Material preparation and data collection were performed by W-JL, B-LS, J-BW, NZ, and R-PZ. The first draft of the manuscript was written by W-JL and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liao, WJ., Sun, BL., Wu, JB. et al. Role of magnetic resonance imaging features in diagnosing and localization of disc rupture related to cervical spinal cord injury without radiographic abnormalities. Spinal Cord 61, 323–329 (2023). https://doi.org/10.1038/s41393-023-00886-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00886-2