Abstract
Spinal Cord Injury (SCI) is a condition whose consequences can impact the physical, emotional, and social aspects of patient’s life, including Depression and Anxiety disorders. Study Design: Using a cross-sectional design, sociodemographic and clinical data were extracted from 556 SCI patients at the time of initial assessment, prior to intensive rehabilitation treatment at the local rehabilitation institute. Objectives: Identify the predictive and multivariate relationship between different sociodemographic and clinical variables of Depression and Anxiety symptoms in SCI patients. Setting: Lucy Montoro Rehabilitation Institute (LMRI), University of Sao Paulo, Sao Paulo, Brazil. Methods: We performed independent univariate and multivariate regression models using the Hospital Anxiety and Depression Scale (HADS) as dependent variable. Results: Symptoms of depression and anxiety present in SCI patients negatively correlate with the level of independence for locomotion, personal hygiene, bowel control, social interaction measured by the Functional Independence Scale (FIM), type of medication in use and the Language subtest of the MoCA Scale. Unlike previous studies, we did not find a relationship with the use of alcohol and illicit drugs, injury levels, etiological diagnosis or duration of injury. For the anxiety models, the main predictor was Depression symptoms, with SCI-related aspects not being significant. It was found that characteristics of the FIM Scale and cognitive aspects of the MoCA Scale were the main predictors of symptoms of Depression. Characteristics of the injury and motor deficit were not statistically significant. Conclusions: These findings can potentially be used to guide clinical practices to identify patients at higher risk of experiencing symptoms of Depression and Anxiety.
Similar content being viewed by others
Introduction
The spinal cord injury (SCI) affects motor, sensory and autonomic functions and could lead to physical incapability and the need to complex cares. In Brazil, according to data from the Especializada [1], there are disagreements regarding the most common etiology of spinal cord injury. A large part of the cases would be related to car accidents, and as the second most common cause, injuries caused by firearm projectiles. In general, as the bibliography presents specific studies in traumatology services, where the survey and description of cases were carried out, according to these studies, the most common cause is related to falls, mainly falls from slabs. Regardless of the injury etiology, the impact of physical, emotional, and social conditions is important and can compromise the rehabilitation program [2]. The incidence of SCI varies around the world. Among developed countries, the incidence of traumatic SCI is higher in North America (39 cases per million inhabitants) than in Australia (16 cases per million inhabitants) or in Western Europe (15 cases per million inhabitants), due to high crime and self-harm rates [3]. In Brazil it is estimated that the occurrence is 40 cases per million inhabitants, adding up to 6–8 thousand cases per year. However, the incidence coefficient of spinal cord injury in Brazil is unknown, since this condition is not subject to notification. In the state of São Paulo, the estimated value of new cases is 3327 per year [4].
Although the incidence of depression on SCI patients is unclear, it is well known that it is a common issue [5]. Based on the criteria of The Diagnosis and Statistical Manual of Mental Disorder - Fifth Edition, it is estimated that 20–38% of individuals with spinal cord injury will present significant symptoms of depression during the rehabilitation treatment period; and 11–31% of individuals already in the community will present a depressive episode [6]. A 2019 Iranian meta-analysis identified that the incidence of Depression in this clinical group was 22.6% for Mild Depression, 19.6% for moderate and 12.1% for severe [7]. Another Taiwanese study identified a 1.29-fold incidence of increased risk of anxiety or depression in SCI compared to the group with other health conditions [8]. Specifically in relation to Brazil, as reviewed in the study by Placeres and Fiorati [9], only two studies sought to understand this prevalence within the SCI group, with Conceição, Auad [10] found a prevalence of 35.2% of mild depression and 36.8% of severe depression, and Almeida, Santo [11] found a prevalence of 28% for mild depression, 16% for moderate and 6% for severe depression. Thus, it is possible to observe that the values change significantly from study to study, also because they use different instruments (Brazilian studies, for example, used the Beck Depression Inventory).
Anxiety symptoms are commonly observed within depression symptoms. Within SCI patients, 45% report fear, panic, excessive worries, and other symptoms which could lead to Generalizes Anxiety Disorder [12]. The traumatic nature related with the lesion probably explains the higher incidence of anxiety in this population [13]. Furthermore, compared to depression patients without SCI, SCI patients were more likely to develop anxiety after leaving hospital. This fact is explained because several confrontation mechanisms could use anxiety as a tool to understand the new condition [8]. Nevertheless, it is important to distinguish an adaptive process from a pathological condition.
The rehabilitation program should be active and dynamic; the presence of depression and anxiety symptoms can compromise the process. Depression is related with diminished leisure and social activities, poor mobility, minor functional gain and unsatisfactory final results [14, 15]. Psychological comorbidities are an important obstacle to intensive rehabilitation, where the patient is under an intense, practical, and integrative learning process. Identifying the factors associated with depression could lower the impact of the disorder on the rehabilitation program.
Previous studies have shown that patients at an age between 25 and 49 years old, female, divorced, unemployed, low school level, low income and ethnical minorities, are more likely to develop depression after a SCI [15, 16]. However, those who live longer––20 years or more after the injury––tends to present fewer cases of depression [17].
Other conditions which intensify depression are previously comorbidities such as psychiatric disorders as well as drug or alcohol addiction. Patients who had disfunction, after the injury, such as fecal continence, bladder control and motor control––characterize as worse by ASIA level––also present higher results on Hospital Anxiety and Depression Scale (HADS) [18]. Chronical pain has been shown as an important clinical factor for depression development, and this sign is present in 41% of the patients one year after the injury, and 81% after 5 years passed the lesion [14].
Depression and anxiety disorders in SCI patients are associated with lower life quality, longer rehabilitation program, lower functional gain and social life reestablishment, and higher clinical complications. It is important to understand which patients are at risk of developing symptoms and initiate early interventions to prevent the diseases and guarantee an effective rehabilitation process. Furthermore, as far as we know, studies like this have not been conducted with the SCI population in Brazil. Thus, given the breadth of this investigation, in order to find predictors of anxiety and depression symptoms, the present study adopted a model-building approach, with a planned series of univariate tests which led to more complex multivariate models. Therefore, the present study sought to identify clinical and demographic predictors of anxiety and depression symptoms in patients with SCI.
Methods
Data from all 556 patients were analyzed, who underwent the intensive rehabilitation program in the inpatient modality at the Lucy Montoro Rehabilitation Institute (LMRI) for the first time, from 2015 to 2019. Inclusion criteria were patients diagnosed with paraplegia or quadriplegia due to traumatic or non-traumatic etiology. Exclusion Criteria were patients with incomplete data or no initial assessment. Initially, on the day of collection, all patients underwent an anamnesis, which excluded those with any psychiatric comorbidity (schizophrenic symptoms, for example). The retrospective analysis was performed using demographic and clinical data from the Psychology Service and the Electronic Patient Record (EHR) database. The LMRI is located in the city of São Paulo, with a capacity to serve around 64 patients. The diagnoses given are spinal cord injuries, brain injuries and neuromuscular diseases. To carry out the rehabilitation program, the time of injury and/or onset of disability must be less than two years. The treatment is multidisciplinary and subsidized by the SUS (Brazil’s public health system). Patients are referred from the LMRI by hospitals whose treatment was carried out in the acute phase and by the Basic Health Units in the neighborhood. The LMRI is one of the 5 rehabilitation units of the Institute of Physical Medicine and Rehabilitation (IPMR) of the Clinics Hospital of the University of São Paulo Medical School. Regarding ethical approval, this study was submitted and approved by the Ethics Committee for Analysis of Research Projects - CAPPesq of the Clinics Hospital of the University of São Paulo Medical School (N°. Plataforma Brasil 15138519.0000.0068). Also, been a retrospective study, the present study was approved to evaluate participants measures considering their prior consent.
All instruments chosen for the present study were used following the Brazilian validation and, when necessary, cutoff values followed those recommended by the validation studies were adopted. In addition to demographic measures such as gender, age, education, date of injury and date of assessment, some pre-treatment clinical measures were chosen:
American Spinal Injury Association Impairment Scale – ASIA [19]: scale used to classify the severity of injury in individuals with spinal cord injury. It is a 5-point scale that classifies individuals from A (complete) to E (normal); the final score encompasses the sum of sensory and motor scores, in addition to sensory and anal motor assessment.
Functional Independence Measure – FIM [20]: questionnaire that assesses the degree of request from third parties that the patient requires for the performance of motor and cognitive activities [such as: self-care, transfers, locomotion, sphincter control, communication and social cognition - memory, social interaction and problem solving. The instrument’s score ranges from 1 (total dependence) to 7 (complete independence)].
Hospital Anxiety and Depression Scale – HADS [21]: 14-item scale that quantifies and qualifies symptoms of anxiety and depression. The HADS scale contains 14 multiple-choice questions. It consists of two sub-scales, for anxiety and depression, with seven items each that can be scored from zero to three. The global score in each subscale ranges from 0 to 21 and presents as a cutoff point ≥8 for anxiety and ≥8 for depression. It is intended to detect mild degrees of affective disorders in non-psychiatric environments; it is a short scale and can be filled in quickly; the patient is asked to respond based on how they felt during the past week. It is worth mentioning that in a Brazilian study in 2012 [22], the instruments HAD and BDI (Beck Depression Inventory) presented a correlation of 0.71, demonstrating the equivalence of the HAD instrument with a gold standard instrument for the assessment of Depression. In this sense, we add the following sentences to the manuscript.
Montreal Cognitive Assessment Scale – MoCA [23]: scale for screening the following domains: executive function, visual-spatial ability, memory, attention, concentration, working memory, language, and time/spatial orientation. The maximum score is 30 points and a score of 26 or more is considered normal. Application time is approximately 10 min. Because some patients have a neurological picture of quadriplegia, disabling the performance of execution tasks (visuospatial/executive), we used as a reference the adaptation of the application of the MoCA Scale in people with visual impairment suggested by Nasreddine, Phillips [23], where these items were excluded. To calculate the score, we used the rule of three to consider the normality cutoff. Thus, in this study, the maximum score on this scale will be 25 points, and a score of 22 points or more is considered normal.
The scales were applied in the first week of the patient’s hospitalization in the rehabilitation program, always by the responsible psychologists who make up the rehabilitation team.
Data analysis
For these cross-sectional analyses, no sample calculation was performed, and all 556 patients included were analyzed. Univariate and multivariate linear regression analyses were performed considering, Hospital Anxiety and Depression Scale [21] scores, in order to measure associations between the subdomains of anxiety and depression as a dependent variable, and each demographic and clinical variable as an independent variable. For logistic regression, univariate and multivariate, the HADS scale scores were categorized as suggestive or not of anxiety or depression. The cutoff value ≥8 for anxiety and depression was used, as recommended in the scale validation (Zigmond, 1983).
For all models, a univariate analysis was initially performed for each of the predictors used in the linear or logistic regression in order to determine the values of the unadjusted β coefficients or Odds Ratios (OR) and the 95% confidence intervals (CI). Also, all variables chosen for the univariate analyzes were reviewed and chosen based on a criterion and biological relevance. That is, only the variables that actually made sense to evaluate were analyzed (for example, we disregarded variables such as height and BMI). In the final model, the variables that had a p value < 0.1 were included as independent variables (see supplementary information), in order to include potential confounding factors that did not reach the significance level of 0.05 in the univariate analysis. Variables that did not maintain statistical significance were excluded one by one from the model (backward stepwise regression), a method that is typically adopted based on the validity of this procedure in its ability to avoid suppressor effects. The analyzed variables were tested as potential confounders in the final model. The change in the β coefficient or the OR by more than 10%, or the change in the significance of the variable in the model, was considered confounding. In order to guarantee the statistical quality of the models presented here, the four assumptions defended by Osborne and Waters [24] were adopted, namely: Linearity Homoscedasticity Independence Normality.
Statistical analyzes were performed using STATA 12.1® (StataCorp LP, Texas) and MATLAB® (IBM).
Results
Participants
The sample evaluated was mainly composed of males (76%), with a mean age of 40.6 years and the mean of formal schooling in elementary school of 9.6 years of schooling (see supplementary information). The injuries were predominantly traumatic (72%), approximately half of this sample had a neurological classification of paraplegia (59%) and according to the ASIA scale, complete injuries were the most common (34%). About 27% of patients have traumatic brain injury (TBI). The mean time between the onset of the disability (injury date) and evaluation (start of the inpatient rehabilitation program) was an average of 467 days (15 months).
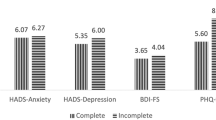
The mean result of the Functional Independence Measure (FIM) was 76.2 (±20.4). The mean scores on the anxiety and depression subscales, measured by the HAD Scale, were respectively 5.8 (±3.7) and 4.4 (±3.6). According to the HAD Scale, anxiety and depression symptoms were present in approximately 28% and 20% of the sample, respectively. The mean score on the MoCA Scale was 19.4 (±3.7). Importantly, these percentages represent patients with significant symptoms of depression and anxiety but not necessarily the clinical diagnosis of these clinical groups.
Pre-rehabilitation treatment clinical data related to comorbidities and habits/addictions showed systemic arterial hypertension (SAH) as the predominant comorbidity, with 18% of the sample, followed by Diabetes Melitus (DM) 8% and Dyslipidemia with 7% of patients. Smoking and alcoholism were the most common habits/addictions, with about 23% and 15%, respectively. As for the use of medications, there is mainly the use of antidepressants (40%), followed by baclofen (37%) and anticonvulsants (33%).
HAD scale – Anxiety
When the demographic variables were analyzed in isolation using univariate logistic regression, the anxiety symptoms of patients with SCI were statistically lower in patients with more years of formal education (p = 0.011; CI = 0.88–0.98). The other demographic and lesion characteristics do not have a statistically significant with anxiety in the univariate linear regression analysis (p < 0.05).
Anxiety symptoms, alone, were statistically higher in patients with low scores in the sub-items of the MoCA Scale, both in the univariate logistic regression analysis: Naming (p = 0.033; CI = 0.49–0.97), Language (p = 0.001; CI = 0.58–0.86) and Late Evocation (p = 0.019; CI = 0.75–0.97); and in the univariate linear regression analysis Naming (p = 0.044; CI = −1.22 to −0.16), Language (p = 0.001 CI = −0.90 to −0.23), Late Evocation (p = 0.063 CI = −0.42–0.01). Furthermore, statistically, the greater the anxiety symptoms, the lower the results of the MoCA Scale (univariate logistic regression: p = 0.005, CI = 0.88−0.97; univariate linear regression: p = 0.008, CI = −0.21 to −0.33).
In the isolated univariate logistic regression analysis of anxiety symptoms assessed using the HADS Scale, these were statistically higher in patients who used antidepressants (p = 0.018; CI = 1.08–2.31), anticonvulsants (p = 0.003; CI = 1.22–2.65), Benzodiazepines (p = 0.008; CI = 1.22–3.81), Neuroleptics (p = 0.003; CI = 1.49–6.61), Analgesics with Opioids (p = 0.024; CI = 1.07–2.94 and Opioid (p = 0.029; CI = 1.07–4.06). The univariate linear regression analysis revealed: Antidepressants p = 0.002 CI = 0.38–1.66), Anticonvulsants (p = 0.001 CI = 0.66–1.98), Benzodiazepines (p = 0.044 CI = 0.02–2.11), Neuroleptics (p = 0.001 CI = 1.8–4.51), Analgesic with Opioid (p = 0.17 CI = 0.19–1.99), Opioid (p = 0.05 CI = 0.52–2.95. Regarding comorbidities, habits and addictions, there were no statistically significant values.
Regarding the Functional Independence Measure (FIM), the univariate logistic analysis showed that patients had lower results in the Social Interaction (p = 0.005; CI = 0.60–0.91), Problem Solving (p = 0.018; CI = 0.66–0.96) and Memory (p = 0.033; CI = 0.61–0.98) were also associated with a higher incidence of anxiety. In the univariate linear analysis, the factors related to anxiety were initial FIM (p = 0.06 CI = −0.30–0.00), Social Interaction (p = 0.001 CI = −1.12 to −0, 40), Troubleshooting (p = 0.001 CI = −0.79 to −0.14) and Memory (p = 0.001 CI = −0.96 to −0.15).
HAD scale – Depression
When analyzed separately in univariate logistic regression, symptoms of depression are statistically higher in female patients (p = 0.023; CI = 0.36–0.92). The other demographic and lesion characteristics did not correlate to depression symptoms.
Regarding the MoCA Scale, in isolation, the univariate logistic regression analysis of symptoms of depression was statistically higher in patients with low scores in the Language sub-item (p = 0.002; CI = 0.57–0.88). Furthermore, statistically, the greater the symptoms of depression, the lower the total results of the MoCA Scale (p = 0.042; CI = 0.99–0.99). In the univariate linear regression analysis, the topics Attention (p = 0.069; CI = −0.43–0.01), Language (p = 0.001; CI = −1.00 to −0.37) were statistically relevant. Late Evocation (p = 0.055 CI = −0.49–0.48) and lower MoCA scores (p = 0.003; CI = −0.21 to −0.04).
The evaluation using the HADS Scale showed an association in the univariate logistic and linear analysis, respectively, in patients who used antidepressants (logistic: p = 0.021; CI = 1.07–2.55/linear: p = 0.001 CI = 0.37–1.59), Anticonvulsants (logistic: p = 0.001; CI = 1.37–3.29/linear: p = 0.001 CI = 0.062–1.88), Benzodiazepines (logistic: p = 0.003; CI = 1.35–4. 53/linear: p = 0.002 CI = 0.56–2.54) and Neuroleptics (logistic: p = 0.001; CI = 2.23–10.02/ linear: p = 0.001 CI = 1.83–4.41). The association with the use of analgesics with opioids and opioids alone showed no association in the logistic analysis, but there was statistical relevance in the univariate linear analysis (Analgesics with opioids p = 0.045 CI = 0.04–1.76/Opioid p = 0.040 CI = 0.02–2.35). Depression symptoms, when analyzed in isolation, did not have statistically significant results in relation to comorbidities, habits, and addictions.
The relationship between depression and FIM items revealed an association in the univariate logistic regression analysis for Social Interaction (p = 0.001; CI = 0.50–0.80), Problem Solving (p = 0.009; CI = 0.62–0.93) and Memory (p = 0.049; CI = 0.60–0.99). In the univariate linear regression analysis, there was an association with the following items: Bowel Feces Control (p = 0.029; CI = −0.27 to −0.01), Bed to wheelchair transfer (p = 0.046; CI = −0.29–0.00), Locomotion (p = 0.021; CI = −0.31 to −0.02); Locomotion Stairs (p = 0.013 CI = −0.43 to −0.05), Comprehension (p = 0.027; CI = −1.25 to −0.07), Social Interaction (p = 0.001; CI = −1.16 to −0.47), Problem Solving (p = 0.001; CI = −0.83 to −0.21), Memory (p = 0.001 CI = −1.01 to −0.24) and Result (p = 0.045; CI = −0.52–0.00)
Predictive models of HADS scale – Anxiety
Tables 1 and 2 shows the predictive models from the multivariate logistic regression and multivariate linear regression analyses, respectively, using the Hospital Anxiety and Depression Scale (HADS) scores - Anxiety subscale with demographic and injury characteristics, drug classes, comorbidities, MoCA Scale and FIM Scale.
Predictive models of HADS scale – Depression
Tables 3 and 4 present the predictive models from logistic regression and multivariate linear regression analyses, respectively, using the Hospital Anxiety and Depression Scale (HADS) scores - Depression subscale with demographic and injury characteristics, classes of medications, comorbidities, MoCA Scale and FIM Scale.
Discussion
This research aimed to identify the clinical and demographic predictors of symptoms of Depression and Anxiety in patients with SCI.
Our multivariate regression models provide evidence for the following predictors: (i) Depression symptoms––bowel control, social interaction and personal hygiene, language, anxiety symptoms, use of benzodiazepines and anticonvulsants; and (ii) Anxiety symptoms––depressive symptoms and neuroleptics use. Below we discuss the predictive models of Depression and Anxiety, respectively.
Depression
We found that bowel control, personal hygiene, and locomotion, were negatively correlated with depressive symptoms.
In addition to the sensory and motor impairment that occurs after a spinal cord injury, individuals suffer from several secondary complications, such as bladder and bowel dysfunction due to autonomic problems. Of the two dysfunctions, bladder dysfunction is the best described [25], but as far as we know, there are knowledge gaps on bowel dysfunction in this population. A study by Ng C et al. [18] found an association between bowel incontinence and higher depression levels.
Patients with Depression symptoms may show self-care negligence. However, with the onset of disability, for some patients, performing these activities requires modifying objects and the environment, making them adaptable and accessible. As the patients in this study, up to the time of the evaluation, had not undergone a rehabilitation program, their knowledge about adaptations and accessibility was impoverished. Thus, another hypothesis to be raised is that the difficulty or inability to perform these activities can also lead them to develop depressive symptoms.
With regard to Locomotion, patients presenting higher scores on the HADS scale had lower scores on the FIM Scale for this item. A hypothesis for this result is that the degree of disability that could be a physical limitation, such as the neurological level in the ASIA Scale, was not a Depression predictor. That is, regarding the neurological level and type of injury from the ASIA scale, as well as in some other studies [26, 27], the present work did not find an association between depressive symptoms and injury and severity levels. Thus, psychological manifestations related to Depression are not explained by the severity of the disability but can be explained by the ability or not to ambulation in their daily lives. A quadriplegic patient with the necessary adaptations for ambulation and getting around does not necessarily present depressive symptoms. However, as this scale assesses based on what the individual does and not their ability to do, the patient with Depressive symptoms who is able to move may not move as a result of their emotional state.
Patients with low scores on social interaction presented higher depressive symptoms. Social cognition skills are needed to properly interact with others in personal, work and academic settings. Psychiatric conditions (such as Depressive symptoms) affect social capacity, making it difficult to adapt in most environments [28]. Thus, the results found in this study indicate that the depressive symptoms in people with SCI significantly correlates to patients’ need assistance to perform the task. It is worth mentioning that regarding FIM Social interaction item, low levels on this item mean that the subjects need assistance to perform the task, not that they don’t have social interactions. Probably, social isolation related to the SCI condition could affect patient’s mood, however, future studies should address this specific point using another specific social interaction measure.
A relevant finding of our study was the correlation between the MoCA Language subtest with depressive symptoms. Depression patients often perform poorly on executive function tests, as Stroop test [29]. Norris, Blankenship–Reuter [30] suggested that verbal fluency tests may be especially sensitive to depressive illness, as there are clear similarities between cognitive demands for fluency and deficits typically associated with Depression, including the ability to sustain attention, concentration, recovery, and processing speed. A first study [31] examining the internal consistency and accuracy of the MoCA Scale in Depression patients showed that verbal fluency, may reflect the individual’s processing speed. It is important to highlight that, although the regression analysis used the MoCA variable as independent and the HADS Depression variable as dependent, the results need to be interpreted with caution regarding the linearity of the relationship. We understand that the regression applied here play a role in revealing information that complements the simple relationship between measures, also revealing how much one measure can predict another and vice versa. This is significantly relevant/evident when we think about these analyzed variables, since it is difficult to say which comes first, if the patient is depressed as a result of the social isolation to which he is subjected, or if depression impairs the capacity for social interaction. The same applies to cognitive aspects. In any case, the results defend that, in addition to a simple relationship, both measures discussed here have a predictive character for each other.
At the time of admission for intensive rehabilitation treatment, most patients were using some type of medication. The drugs most used by our sample were antidepressants (40%), followed by baclofen (37%) and anticonvulsants (33%). A considered hypothesis points to the prescription of antidepressants for pain treatment (mainly serotonin-norepinephrine receptor inhibitors or low-dose antidepressants), and not necessarily for the management of any mood change. Similarly, Craig, Perry [32] found that psychotropic medications were prescribed to more than 36% of the sample, with the majority being antidepressants. However, the use of antidepressants was not statistically significant in our model. Probably, in our sample we have patients in the initial phase of treatment, whose drug response has not yet occurred, since 20–40% of patients respond to the antidepressant only after two months of starting to use the drug [33] and 50% of patients who do not respond to a primary antidepressant improve when another antidepressant is introduced [34]. In addition, some patients were taking antidepressants for pain, which is another reason why we have not found a clear correlation between the use of antidepressants and Depression.
However, two other drug classes were part of the model and are predictors of Depressive symptoms, benzodiazepines and anticonvulsants. Possibly, most patients with SCI have chronic neuropathic pain. It is known that for the treatment of neuropathic pain, the use of anticonvulsants such as gabapentin and pregabalin are first-line medications capable of reducing pain intensity and frequency [35]. Neuropathic pain is a chronic, complex and challenging condition after SCI. Furthermore, clinical and preclinical studies indicate that chronic pain corresponds to adaptations in various brain networks involved in mood, motivation and reward [36]. The same hypothesis can be raised in relation to benzodiazepines, since an alternative view is that some benzodiazepines are used to treat neuropathic pain. Also, the benzodiazepine can be a confounder for other symptoms commonly related to depression, such as anxiety and insomnia, as it can be used for such symptoms.
The occurrence rates of Anxiety and depressive symptoms in patients with SCI found in this study ranged around 28% and 19%, respectively, and are in agreement with previous studies that estimate 20–38% for depressive symptoms [37] and 15–32% for Anxiety symptoms [13]. Observing that Anxiety symptoms were greater compared to depressive symptoms can be explained from the understanding that Anxiety symptoms occurred as a coping mechanism for the consequences of SCI [8].
Anxiety
We found that HADS-Depression and the use of neuroleptics were important predictors for Anxiety symptoms.
Comorbidity between mood and Anxiety disorders is known to be common [38]. Epidemiological data indicate that subjects who had Major Depression diagnosis (57.5%) also met criteria for at least one Anxiety disorder [39]. Another study indicated that subjects with generalized Anxiety disorder (59%) met criteria for major depression [40]. Therefore, these findings suggest that comorbidity between depressive and Anxiety symptoms are common rather than an exception.
Patient who uses neuroleptics present greater Anxiety symptoms. Possibly, this medication was prescribed for patients with higher anxiety symptoms, such as excessive worry, irritability, restlessness, hypervigilance, and insomnia.
Health professionals and SCI family members may benefit from the present results, since tracking the functionality, medications in use and cognitive status of patients with SCI is important to early identify such psychological changes, which may lead to better results in intensive inpatient rehabilitation treatment.
Regarding the study main limitations, the absence of the normality value for the population with SCI in the MoCA Scale total score, possibly impact the present study. It is known that, frequently, in studies with patients whose manual and upper limb motor functions are compromised, items that require manual execution, are removed. Thus, the elimination of these items can lead to reduced validity of the cognitive scale. However, this study pointed out the need for future research, with this same population, with methods that use new technologies, such as Eye Tracking, which is capable of tracking and recording eye movements in real time.
Data need to be interpreted in relation to the country of collection, in this case Brazil. We understand that this point represents both a limitation and an innovative fact. Possibly the level of assistance and accessibility existing in the Brazilian context, specific to the region of the city of São Paulo, presented prior to hospitalization (time of the evaluation under discussion), negatively influenced the levels of anxiety and depression, since the public systems are not as effective as expected. Thus, this factor may have revealed an atypical scenario of SCI patients in the world. On the other hand, many countries have similar and even worse public health situations than Brazil, possibly presenting similar or even more negative results, with regard to the impact of functional limitations on symptoms of Depression and Anxiety.
Another limitation of this study concerns the correlation of pain and sleep quality with symptoms of anxiety and depression. A care taken in the collection of data from the electronic medical record was the accuracy of the information, in order to ensure the production of reliable information. Thus, it was possible to note the existence of an overlap between the data found in clinical practice and those collected for a robust clinical study. Thus, as data related to pain and sleep quality were not described in a standardized and systematic way, we chose to remove this information from the study. Another important point to be mentioned is the absence of measures related to pain and sleep. Since it is a retrospective study that did not have these measures as an evaluation objective, it is not possible to measure these two relevant aspects for the review and discussion of the results presented here. We believe that both measures should be part of assessments in future studies, as they can substantially contribute to the discussion of predictors of depression and anxiety, as well as to the statistical models presented here. Anyway, despite a significant limitation of the present study, the absence of these measures does not make the results presented here unfeasible, since several independent measures included in our models do not have a priori relationship with the measures of sleep and pain (such as, for example, locomotion).
Also, our study, as a cross-section study only evaluated the patients in a single moment, specifically in the first week of treatment. Possibly the results presented here may vary depending on the moment of rehabilitation in which the assessment is carried out. Importantly, in the present study, we sought to evaluate the first week to exclude possible effects of the intervention and characterize the phenomenon at the initial moment of rehabilitation. Future studies can assess whether the predictive measures presented here vary throughout rehabilitation and even whether these independent measures can predict possible variations between the initial and final moments of rehabilitation.
Lastly, it is important to highlight that the findings of the present study, although relevant to the international scenario, represent an assessment of a significant sample of patients with SCI in Brazil. Thus, the results need to be interpreted with caution regarding extrapolation to patients from other national and international centers.
Finally, based on the results found in this study, it is imperative to think that it is up to the rehabilitation professional to look at the patient considering their functionality, much more than the degree of their disability. As recommended by the ICF, consider functionality as a “dynamic interaction between the individual’s health condition, environmental factors and personal factors” [41]. As important as seeking the recovery of motor function, it is to adapt and compensate for deficits, seeking to maximize functional independence to lead individuals with SCI to reintegrate society and potentially improve their quality of life.
References
Especializada BMdSSdAàSDdAPEeDdA. Diretrizes de Atenção à Pessoa com Lesão Medular. Ministério da Saúde Brasília; 2013.
Hitzig SL, Titman R, Orenczuk S, Clarke T, Flett H, Noonan VK, et al. Development of Emotional Well-Being indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J spinal cord Med. 2019;42:85–98. sup1.
Cripps RA, Lee BB, Wing P, Weerts E, Mackay J, Brown D. A global map for traumatic spinal cord injury epidemiology: towards a living data repository for injury prevention. Spinal cord. 2011;49:493–501.
Metrics IfH, Evaluation. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Results. Institute for Health Metrics and Evaluation Seattle; 2017.
Frank RG, Elliott TR, Corcoran JR, Wonderlich SA. Depression after spinal cord injury: Is it necessary? Clin Psychol Rev. 1987;7:611–30.
Bombardier CH, Adams LM, Fann JR, Hoffman JM. Depression trajectories during the first year after spinal cord injury. Arch Phys Med rehabilitation. 2016;97:196–203.
Hatefi M, Abdi A, Tarjoman A, Borji M. Prevalence of depression and pain among patients with spinal cord injury in Iran: a systematic review and meta-analysis. Trauma Monthly. 2019;24:e87503–e.
Lim S-W, Shiue Y-L, Ho C-H, Yu S-C, Kao P-H, Wang J-J, et al. Anxiety and depression in patients with traumatic spinal cord injury: a nationwide population-based cohort study. PLoS One. 2017;12:e0169623.
Placeres AF, Fiorati RC Assessment instruments and depression rates in people with spinal cord injury: a systematic review. Revista da Escola de Enfermagem da USP. 2018;52:1–10.
Conceição MIG, Auad JC, Vasconcelos L, Macêdo A, Bressanelli R. Avaliação da depressão em pacientes com lesão medular. Rev Brasileira de Ter Comportamental e Cognitiva. 2010;12:43–59.
Almeida SAd, Santo PFdE, Silveira MM, Openheimer DG, Dutra RAA, Bueno MdLGB, et al. Depression in patients with traumatic spinal cord injuries and pressure ulcers. Revista Brasileira de Cirurgia Plástica. 2013;28:282–8.
Mitchell M, Burns N, Dorstyn D. Screening for depression and anxiety in spinal cord injury with DASS-21. Spinal Cord. 2008;46:547–51.
Le J, Dorstyn D. Anxiety prevalence following spinal cord injury: a meta-analysis. Spinal Cord. 2016;54:570–8.
Williams RT, Wilson CS, Heinemann AW, Lazowski LE, Fann JR, Bombardier CH. Identifying depression severity risk factors in persons with traumatic spinal cord injury. Rehabilitation Psychol. 2014;59:50.
Bombardier CH, Richards JS, Krause JS, Tulsky D, Tate DG. Symptoms of major depression in people with spinal cord injury: implications for screening. Arch Phys Med rehabilitation. 2004;85:1749–56.
Saunders LL, Krause J, Focht KL. A longitudinal study of depression in survivors of spinal cord injury. Spinal cord. 2012;50:72–7.
Krause JS, Saunders LL, Newman S. Posttraumatic stress disorder and spinal cord injury. Arch Phys Med rehabilitation. 2010;91:1182–7.
Ng C, Prott G, Rutkowski S, Li Y, Hansen R, Kellow J, et al. Gastrointestinal symptoms in spinal cord injury: relationships with level of injury and psychologic factors. Dis colon rectum. 2005;48:1562–8.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, et al. International standards for neurological classification of spinal cord injury. J spinal cord Med. 2003;26:S50–S6. sup1.
Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the Functional Independence Measure. Arch Phys Med rehabilitation. 1994;75:127–32.
Zigmond A, Snaith R. A escala de ansiedade e depressão hospitalar. Acta Psychiatr Scand. 1983;67:361–70.
Falavigna A, Righesso O, Teles AR, Baseggio N, Velho MC, Ruschel LG, et al. Depression Subscale of the Hospital Anxiety and Depression Scale applied preoperatively in spinal surgery. Arquivos de neuro-psiquiatria. 2012;70:352–6.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. JAGS. 2019;53:695–9.
Osborne JW, Waters E. Four assumptions of multiple regression that researchers should always test. Practical Assess, Res, evaluation. 2002;8:2.
Hu HZ, Granger N, Jeffery N. Pathophysiology, clinical importance, and management of neurogenic lower urinary tract dysfunction caused by suprasacral spinal cord injury. J Vet Intern Med. 2016;30:1575–88.
Craig A, Hancock K, Dickson H. A longitudinal investigation into anxiety and depression in the first 2 years following a spinal cord injury. Spinal Cord. 1994;32:675–9.
Bombardier CH, Fann JR, Tate DG, Richards JS, Wilson CS, Warren AM, et al. An exploration of modifiable risk factors for depression after spinal cord injury: which factors should we target? Arch Phys Med Rehabilitation. 2012;93:775–81.
Gillen G. Cognitive and perceptual rehabilitation. Optimizing function Missouri: Mosby Elsevier. 2009.
Lee RS, Hermens DF, Porter MA, Redoblado-Hodge MA. A meta-analysis of cognitive deficits in first-episode major depressive disorder. J Affect Disord. 2012;140:113–24.
Norris MP, Blankenship-Reuter L, Snow-Turek AL, Finch J. Influence of depression on verbal fluency performance. Aging, Neuropsychol, cognition. 1995;2:206–15.
Srisurapanont M, Eurviriyanukul K, Suttajit S, Varnado P. Internal consistency and concurrent validity of the Montreal Cognitive Assessment in individuals with major depressive disorder. Psychiatry Res. 2017;253:333–7.
Craig A, Perry KN, Guest R, Tran Y, Dezarnaulds A, Hales A, et al. Prospective study of the occurrence of psychological disorders and comorbidities after spinal cord injury. Arch Phys Med Rehabilitation. 2015;96:1426–34.
Shelton RC. Treatment options for refractory depression. J Clin Psychiatry. 1999;60:57–63.
Panel DG Depression in Primary Care: volume 2 treatment of major depression. Clinical practice guideline. 1993.
Levendoglu F, Ögün CÖ, Özerbil Ö, Ögün TC, Ugurlu H. Gabapentin is a first line drug for the treatment of neuropathic pain in spinal cord injury. Spine 2004;29:743–51.
Descalzi G, Mitsi V, Purushothaman I, Gaspari S, Avrampou K, Loh Y-HE, et al. Neuropathic pain promotes adaptive changes in gene expression in brain networks involved in stress and depression. Sci Signal. 2017;10:1–39.
Bombardier CH, Hoekstra T, Dikmen S, Fann JR. Depression trajectories during the first year after traumatic brain injury. J neurotrauma. 2016;33:2115–24.
Johansson R, Carlbring P, Heedman Å, Paxling B, Andersson G. Depression, anxiety and their comorbidity in the Swedish general population: point prevalence and the effect on health-related quality of life. PeerJ 2013;1:e98.
Kessler RC, Merikangas KR, Wang PS. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annu Rev Clin Psychol. 2007;3:137–58.
Carter RM, Wittchen HU, Pfister H, Kessler RC. One‐year prevalence of subthreshold and threshold DSM‐IV generalized anxiety disorder in a nationally representative sample. Depression anxiety. 2001;13:78–88.
Organization WH. How to use the ICF: A practical manual for using the International Classification of Functioning, Disability and Health (ICF). Exposure draft for comment Geneva: WHO. 2013;10:1–127.
Acknowledgements
Authors are grateful to Margarida H. Miyazaki, executive director of IMREA, Fabio Pacheco Muniz de Souza e Castro, executive director of LMRI, Katia Lina Miyahara and Mariane Tateishi, Clinical Director of IMREA, for the great support of the hospital. Besides, Vera Lucia Rodrigues Alves, Valéria Dini Leite, Daniel Rubio de Souza, Artur César Aquino dos Santos for assistance with study monitoring.
Funding
This work was supported by Núcleo de Apoio a Pesquisa-Núcleo de Estudos Avançados em Reabilitação (NAP-NEAR). The researchers received support from the São Paulo Research Foundation (FAPESP- SPEC, grant #2017/12943-8). Specifically, LMM is supported by a postdoctoral research grant #2021/05897-5, São Paulo Research Foundation (FAPESP).
Author information
Authors and Affiliations
Contributions
SMS and LRB developed the study concept and design. Data collection was performed by ACP-H and NCA, MS and ACP-H performed the data analysis. FF contributed to data interpretation. LMM, ACP-H and all other authors contributed to manuscript writing and approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was submitted and approved by the Ethics Committee for Analysis of Research Projects - CAPPesq of the Clinical Hospital of the Faculty of Medicine of USP (N°. Plataforma Brasil 15138519.0000.0068).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hara, A.C.P., Aching, N.C., Marques, L.M. et al. Clinical and demographic predictors of symptoms of depression and anxiety in patients with spinal cord injury. Spinal Cord 60, 1123–1129 (2022). https://doi.org/10.1038/s41393-022-00831-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00831-9