Abstract
Background
The utilization of MRI to risk stratify elevated PSA prior to prostate biopsy has been inconsistently adopted and varies considerably by practice setting. This study aims to evaluate the usage and performance of MRI as an advanced risk stratification tool of elevated PSA prior to biopsy and identify factors associated with differential utilization of MRI at a large academic setting with ready access to 3T multiparametric MRI of the prostate.
Methods
A retrospective single-center study of 2900 men presenting with elevated PSA 2–20 ng/mL from 2018 through 2021 was conducted. We analyzed trends in MRI utilization and outcomes of prostate biopsy by MRI usage. Univariate and multivariate logistic regressions were performed to calculate odds ratios to identify patient- and provider-level predictors of MRI usage.
Results
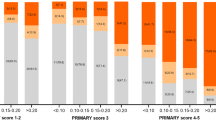
Rates of prebiopsy MRI utilization increased from 56% in 2018 to 89% in 2021 (p < 0.001). Prebiopsy MRI led to biopsy avoidance in 31% of men. MRI usage enhanced detection of clinically significant prostate cancer by 13% and reduced identification of Gleason Grade Group 1 disease by 3% and negative biopsies by 10% (p < 0.001). Men who received MRI were more likely to be younger than 75 years in age and have private or Medicare insurance, PSA >4 ng/mL, and PHI >27. In both univariate and multivariate analysis, black race and Medicaid insurance were associated with reduced MRI utilization (all p < 0.001). Urologic provider was an independent predictor of MRI usage (p < 0.001).
Conclusions
Use of MRI as a risk stratification tool for elevated PSA rose during this 4-year study period. Men who self-identify as black or men with Medicaid coverage have diminished rates of MRI usage. Considerable provider-level variability in MRI use was observed. Future research aimed at identifying factors affecting implementation of MRI as a routine risk assessment tool is warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data are included in the manuscript and/or the Supplementary material. De-identified data can be shared upon request.
References
American Cancer Society. Cancer Facts & Figures 2022. Atlanta: American Cancer Society. 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf.
Andriole GL, Crawford ED, Grubb RL, Buys SS, Chia D, Church TR, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009;360:1310–9. https://www-nejm-org.ezproxy.galter.northwestern.edu/doi/10.1056/NEJMoa0810696.
Hugosson J, Roobol MJ, Månsson M, Tammela TLJ, Zappa M, Nelen V, et al. A 16-yr follow-up of the european randomized study of screening for prostate cancer. Eur Urol. 2019;76:43.
Schröder FH, Hugosson J, Roobol MJ, Tammela TLJ, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360:1320–8. https://pubmed-ncbi-nlm-nih-gov.ezproxy.galter.northwestern.edu/19297566/.
Loeb S, Sanda MG, Broyles DL, Shin SS, Bangma CH, Wei JT, et al. The Prostate Health Index selectively identifies clinically significant prostate cancer. J Urol. 2015;193:1163.
Kasivisvanathan V, Jichi F, Klotz L, Villers A, Taneja SS, Punwani S, et al. A multicentre randomised controlled trial assessing whether MRI-targeted biopsy is non-inferior to standard transrectal ultrasound guided biopsy for the diagnosis of clinically significant prostate cancer in men without prior biopsy: a study protocol. BMJ Open. 2017;7:e017863.
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 2017;389:815–22.
Bass EJ, Pantovic A, Connor MJ, Loeb S, Rastinehad AR, Winkler M, et al. Diagnostic accuracy of magnetic resonance imaging targeted biopsy techniques compared to transrectal ultrasound guided biopsy of the prostate: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2021;1–6. https://www-nature-com.ezproxy.galter.northwestern.edu/articles/s41391-021-00449-7.
Eklund M, Jäderling F, Discacciati A, Bergman M, Annerstedt M, Aly M, et al. MRI-targeted or standard biopsy in prostate cancer screening. N Engl J Med. 2021;385:908–20.
Feuer Z, Meng X, Rosenkrantz AB, Kasivisvanathan V, Moore CM, Huang R, et al. Application of the PRECISION trial biopsy strategy to a contemporary magnetic resonance imaging-targeted biopsy cohort–how many clinically significant prostate cancers are missed? J Urol. 2021;205:740–7. https://pubmed-ncbi-nlm-nih-gov.ezproxy.galter.northwestern.edu/33026927/.
2.2021 NG version. Prostate Cancer Early Detection. 2021. www.NCCN.org.
EAU Guidelines. Edn. Presented at the EAU Annual Congress: Milan; 2021.
Kim SJ, Vickers AJ, Hu JC. Challenges in adopting level I evidence for multiparametric magnetic resonance imaging as a biomarker for prostate cancer screening. JAMA Oncol. 2018;4:1663.
Liu W, Patil D, Howard DH, Moore RH, Wang H, Sanda MG, et al. Adoption of prebiopsy magnetic resonance imaging for men undergoing prostate biopsy in the United States. Urology. 2018;117:57–63. http://www.goldjournal.net/article/S009042951830325X/fulltext.
Gaffney CD, Cai P, Li D, Margolis D, Sedrakyan A, Hu JC, et al. Increasing utilization of MRI before prostate biopsy in black and non-black men: an analysis of the SEER-medicare cohort. Am J Roentgenol. 2021;217:389–94.
Catalona WJ, Partin AW, Sanda MG, Wei JT, Klee GG, Bangma C, et al. A multi-center study of [−2]pro-prostate-specific antigen (PSA) in combination with PSA and free PSA for prostate cancer detection in the 2.0 to 10.0 ng/mL PSA Range William. J Urol. 2011;23:1–7.
Barnett CL, Davenport MS, Montgomery JS, Wei JT, Montie JE, Denton BT. Cost-effectiveness of magnetic resonance imaging and targeted fusion biopsy for early detection of prostate cancer. BJU Int. 2018;122:50–8. https://pubmed-ncbi-nlm-nih-gov.ezproxy.galter.northwestern.edu/29388388/.
Rosenkrantz AB, Hemingway J, Hughes DR, Duszak R, Allen B, Weinreb JC. Evolving use of prebiopsy prostate magnetic resonance imaging in the medicare population. J Urol. 2018;200:89–94. https://pubmed-ncbi-nlm-nih-gov.ezproxy.galter.northwestern.edu/29410202/.
Manley BJ, Brockman JA, Raup VT, Fowler KJ, Andriole GL. Prostate MRI: a national survey of urologist’s attitudes and perceptions. Int Braz J Urol. 2016;42:464–71.
Abashidze N, Stecher C, Rosenkrantz AB, Duszak R, Hughes DR. Racial and ethnic disparities in the use of prostate magnetic resonance imaging following an elevated prostate-specific antigen test. JAMA Netw Open. 2021;4:e2132388. https://jamanetwork-com.ezproxy.galter.northwestern.edu/journals/jamanetworkopen/fullarticle/2785789.
Smith ZL, Eggener SE, Murphy AB. African-American prostate cancer disparities. Curr Urol Rep. 2017;18:81. https://pubmed-ncbi-nlm-nih-gov.ezproxy.galter.northwestern.edu/28808871/.
Walton EL, Deebajah M, Keeley J, Fakhouri S, Yaguchi G, Pantelic M, et al. Barriers to obtaining prostate multi-parametric magnetic resonance imaging in African-American men on active surveillance for prostate cancer. Cancer Med. 2019;8:3659–65. https://pubmed-ncbi-nlm-nih-gov.ezproxy.galter.northwestern.edu/31111654/.
Author information
Authors and Affiliations
Contributions
MRS led the study from conception to completion and prepared the manuscript. BA, PVS, JAA, and EVL assisted in data clean-up and manuscript preparation. JMR and AKM helped with data clean-up as well. SASM, M-KK, and QM helped with data processing. XM provided biostats assistance. EMS and AER are senior authors who guided all of the aforementioned processes from study conception to its completion.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Siddiqui, M.R., Ansbro, B., Shah, P.V. et al. Real-world use of MRI for risk stratification prior to prostate biopsy. Prostate Cancer Prostatic Dis 26, 353–359 (2023). https://doi.org/10.1038/s41391-022-00543-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00543-4
This article is cited by
-
Serum free prostate-specific antigen density (fPSAD) as a predictor of prostate cancer: a new parameter worthy of attention
Irish Journal of Medical Science (1971 -) (2024)