Abstract
Background
Research examining the association between physical activity (PA) and prostate cancer (PCa) has accumulated; however, few studies have examined this association in the context of active surveillance. The current study examines this among men initially diagnosed with favorable-risk PCa and managed by active surveillance at Sunnybrook Health Sciences Centre in Canada and the Royal Marsden Hospital in the United Kingdom.
Methods
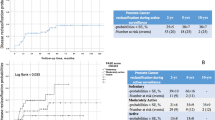
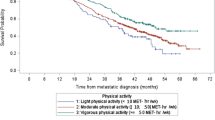
Participants completed a questionnaire on daily participation in non-leisure, transport, and recreational PA. A logistic regression was employed using PA as the independent variable and whether the patient reclassified to higher-risk PCa while on active surveillance as the dependent variable. Demographic and lifestyle covariates were incorporated in the analysis to assess potential confounding and effect modification.
Results
Men from both hospitals presented with similar clinical and demographic characteristics. Total PA was inversely associated with odds of reclassification while on active surveillance (p-trend = 0.027). A weaker inverse association was observed with recreational PA (p-trend = 0.30). Men who participated in weekly vigorous PA were less likely to reclassify than those who did not (odds ratio (95% confidence interval): 0.42 (0.20–0.85)).
Conclusions
Total and vigorous PA were inversely associated with odds of reclassification in two active surveillance cohorts. Given the limitations of this study, more robust prospective observational studies involving objective PA measures are warranted to confirm findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian Cancer Statistics 2016. Toronto: Canadian Cancer Society; 2016.
Klotz L. Active surveillance for low-risk prostate cancer. Curr Urol Rep. 2015;16(4):1–10.
Klotz L, Emberton M. Management of low risk prostate cancer—active surveillance and focal therapy. Nat Rev Clin Oncol. 2014;11(6):324–34.
Cooperberg MR, Carroll PR, Klotz L. Active surveillance for prostate cancer: progress and promise. J Clin Oncol. 2011;29(27):3669–76.
Liu Y, Hu F, Li D, Wang F, Zhu L, Chen W, et al. Does physical activity reduce the risk of prostate cancer? A systematic review and meta-analysis. Eur Urol. 2011;60(5):1029–44.
Antonelli JA, Jones LW, Bañez LL, Thomas J, Anderson K, Taylor LA, et al. Exercise and prostate cancer risk in a cohort of veterans undergoing prostate needle biopsy. J Urot. 2009;182(5):2226–31.
De Nunzio C, Presicce F, Lombardo R, Cancrini F, Petta S, Trucchi A, et al. Physical activity as a risk factor for prostate cancer diagnosis: a prospective biopsy cohort analysis. BJU Int. 2016;117(6B):E29–35.
Richman EL, Kenfield SA, Stampfer MJ, Paciorek A, Carroll PR, Chan JM. Physical activity after diagnosis and risk of prostate cancer progression: data from the cancer of the prostate strategic urologic research endeavor. Cancer Res. 2011;71(11):3889–95.
Kenfield SA, Stampfer MJ, Giovannucci E, Chan JM. Physical activity and survival after prostate cancer diagnosis in the health professionals follow-up study. J Clin Oncol. 2011;29(6):726–32.
Tai S, Hsieh H, Huang S, Wu M. Hair dye use, regular exercise, and the risk and prognosis of prostate cancer: multicenter case–control and case-only studies. BMC Cancer. 2016;16(1):242.
Burton AJ, Martin RM, Donovan JL, Lane JA, Davis M, Hamdy FC, et al. Associations of lifestyle factors and anthropometric measures with repeat PSA levels during active surveillance/monitoring. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1877–85.
Ornish D, Weidner G, Fair WR, Marlin R, Pettengill EB, Raisin CJ, et al. Intensive lifestyle changes may affect the progression of prostate cancer. J Urol. 2005;174(3):1065–70.
Hvid T, Lindegaard B, Winding K, Iversen P, Brasso K, Solomon TP, et al. Effect of a 2-year home-based endurance training intervention on physiological function and PSA doubling time in prostate cancer patients. Cancer Causes Control. 2016;27(2):165–74.
Vandersluis A, Guy D, Klotz L, Fleshner N, Kiss A, Parker C, et al. The role of lifestyle characteristics on prostate cancer progression in two active surveillance cohorts. Prostate Cancer Prostatic Dis. 2016;19:305–10.
Klotz L. Active surveillance for prostate cancer: overview and update. Curr Treat Options Oncol. 2013;14(1):97–108.
Ng MK, Van AsN, Thomas K, Woode‐Amissah R, Horwich A, Huddart R, et al. Prostate‐specific antigen (PSA) kinetics in untreated, localized prostate cancer: PSA velocity vs PSA doubling time. BJU Int. 2009;103(7):872–6.
Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6(6):790–804.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9; Suppl 1):S498–S504.
Byrne NM, Hills AP, Hunter GR, Weinsier RL, Schutz Y. Metabolic equivalent: one size does not fit all. J Appl Physiol. 2005;99(3):1112–9.
Vuillemin A, Oppert J, Guillemin F, Essermeant L, Fontvieille A, Galan P, et al. Self-administered questionnaire compared with interview to assess past-year physical activity. Med Sci Sports Exerc. 2000;32(6):1119–24.
Wekesa A, Harrison M, Watson R. Physical activity and its mechanistic effects on prostate cancer. Prostate Cancer Prostatic Dis. 2015;18(3):197.
Barnard RJ, Ngo TH, Leung P, Aronson WJ, Golding LA. A low‐fat diet and/or strenuous exercise alters the IGF axis in vivo and reduces prostate tumor cell growth in vitro. Prostate. 2003;56(3):201–6.
Schumann M, Mykkänen OP, Doma K, Mazzolari R, Nyman K, Häkkinen K. Effects of endurance training only versus same-session combined endurance and strength training on physical performance and serum hormone concentrations in recreational endurance runners. Appl Physiol Nutr Metab. 2014;40(1):28–36.
Heinlein CA, Chang C. Androgen receptor in prostate cancer. Endocr Rev. 2004;25(2):276–308.
Teixeira G, Fávaro W, Pinheiro P, Chuffa L, Amorim J, Mendes L, et al. Physical exercise on the rat ventral prostate: steroid hormone receptors, apoptosis and cell proliferation. Scand J Med Sci Sports. 2012;22(5):e86–e92.
Deschenes MR, Maresh CM, Armstrong LE, Covault J, Kraemer WJ, Crivello JF. Endurance and resistance exercise induce muscle fiber type specific responses in androgen binding capacity. J Steroid Biochem Mol Biol. 1994;50(3):175–9.
Patten SB. Epidemiology for Canadian students: principles, methods and critical appraisal. Canada: Brush Education Inc.; 2015.
Latini DM, Hart SL, Knight SJ, Cowan JE, Ross PL, DuChane J, et al. The relationship between anxiety and time to treatment for patients with prostate cancer on surveillance. J Urol. 2007;30178(3):826–32.
Galvão DA, Taaffe DR, Spry N, Gardiner RA, Taylor R, Risbridger GP, et al. Enhancing active surveillance of prostate cancer: the potential of exercise medicine. Nat Rev Urol. 2016;13(5):258.
Kristal AR, Stanford JL. Cruciferous vegetables and prostate cancer risk: confounding by PSA screening. Cancer Epidemiol Biomarkers Prev. 2004;13(7):1265.
Parsons JK, Pierce JP, Mohler J, Paskett E, Jung SH, Morris MJ, et al. The Men’s Eating and living (MEAL) study (CALGB 70807 [Alliance]): recruitment feasibility and baseline demographics of a randomized trial of diet in men on active surveillance for prostate cancer. BJU Int. 2017. https://doi.org/10.1111/bju.13890.
Acknowledgements
Funding was not required or mobilized for this project. No additional personnel significantly contributed to this study other than the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Guy, D.E., Vandersluis, A., Klotz, L.H. et al. Total energy expenditure and vigorous-intensity physical activity are associated with reduced odds of reclassification among men on active surveillance. Prostate Cancer Prostatic Dis 21, 187–195 (2018). https://doi.org/10.1038/s41391-017-0010-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-017-0010-0
This article is cited by
-
More evidence that physical activity is beneficial for prostate cancer
Prostate Cancer and Prostatic Diseases (2022)
-
Physical activity decreases the risk of cancer reclassification in patients on active surveillance: a multicenter retrospective study
Prostate Cancer and Prostatic Diseases (2021)
-
Post-Diagnostic Dietary and Lifestyle Factors and Prostate Cancer Recurrence, Progression, and Mortality
Current Oncology Reports (2021)