Abstract
Anemia, defined as a low blood hemoglobin concentration, is a major global public health problem. Identification of anemia is crucial to public health interventions. It is estimated globally that 273 million children under 5 years of age were anemic in 2011, and about ~50% of those cases were attributable to iron deficiency (Lancet Global Health 1:e16–e25, 2013). Iron-deficiency anemia (IDA) in infants adversely impacts short-term hematological indices and long-term neuro-cognitive functions of learning and memory that result in both fatigue and low economic productivity. IDA contributes to death and disability and is an important risk factor for maternal and perinatal mortality, including the risks for stillbirths, prematurity, and low birth weight (Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors. Ch. 3 (World Health Organization, Geneva, 2004)). Reduction in early infantile anemia and newborn mortality rates is possible with easily implemented, low- to no-cost intervention such as delayed cord clamping (DCC). DCC until 1–3 min after birth facilitates placental transfusion and iron-rich blood flow to the newborn. DCC, an effective anemia prevention strategy, requires cooperation among health providers involved in childbirth, and a participatory culture change in public health. Public intervention strategies must consider multiple factors associated with anemia listed in this review before designing intervention studies that aim to reduce anemia prevalence in infants and toddlers.
Impact
-
Anemia, defined as a low blood hemoglobin concentration, is a major global public health problem and identification of anemia is crucial to public health interventions.
-
Delayed cord clamping (DCC) until 1–3 min after birth facilitates placental transfusion and iron-rich blood flow to the newborn.
-
Reduction in early infantile anemia and newborn mortality rates is possible with easily implemented, low- to no-cost intervention such as DCC.
Similar content being viewed by others
Introduction
Anemia is a condition in which hemoglobin (Hb) concentration is lower than the normal expected ranges for age and sex.1,2 The definition of anemia is not straightforward, and one must consider age-specific variation in Hb cut-offs, clinical, environmental, population distribution of Hb values, and ethnic variation besides laboratory and diagnostic considerations for Hb measurement.3 Physiologically, anemia is defined as a condition in which the number of circulating red blood cells (RBCs) is insufficient to meet the oxygen requirement of tissues and the body’s physiologic needs. Hb thresholds differ for different population groups. Regardless of the type of definition, Hb levels below an established cut-off value impair the capacity of RBCs to transport oxygen. The resultant tissue hypoxia result in fatigue and impairment of work capacity with negative consequences to both physical and cognitive development.4,5 Anemia is an indicator of both poor nutrition and poor health. One in four people are affected by anemia, and the most vulnerable populations are pregnant women and preschool-age children (0–4.99 years).6
Anemia can result from multiple causes, including nutritional deficiency, infection and inflammation from disease, acute or chronic blood loss, and genetic Hb disorders. However, iron deficiency is the most common cause of anemia worldwide.7 Iron-deficiency anemia (IDA) is a widespread public health problem, particularly in low- and middle-income countries. The World Health Organization (WHO) estimates globally that ~273 million young children under 5 years are anemic, among which ~50% are estimated to suffer from iron deficiency.2,6 There is a high demand for dietary iron during infancy and preschool years to support physical growth, rapid brain development, and early learning capacity.8,9 Prompt identification and treatment of anemia leads to overall improvement of population health outcomes, improved physical exercise performance, and well-being that results in enhanced economic productivity. The focus of this review will be on the determinants and solutions to IDA including development of an anemia-control strategy that specifically targets infants under 1 year of age and toddlers.
Global prevalence of anemia
Figure 1a–c depict the global estimates of the prevalence of anemia as a public health problem in infants and children aged 6–59 months, pregnant women aged 15–49 years, and in non-pregnant women aged 15–49 years, 2011.2 In 2011, population-representative data sources from 107 countries worldwide revealed that 29% (496 million) of non-pregnant women and 38% (32.4 million) of pregnant women aged 15–49 years were reported to be anemic.10 Anemia prevalence continues to be the highest in South Asia and Central and West Africa.10 Prevalence of IDA among infants and preschoolers living in rural India was 52.2% and 42.1%, respectively.11 In 2012, the World Health Assembly specified six global nutrition targets for 2025, with a commitment for a 50% reduction of anemia in women of reproductive age by 2025 compared to 2011 levels.12 Table 1 summarizes the top 10 countries across the globe with the highest incidence/burden of iron deficiency.
Effect of IDA on maternal mortality
Low Hb during pregnancy has been associated with an increased risk of maternal mortality,13 perinatal mortality, and low birth weight/small-for-gestational-age outcomes.14,15,16 Table 2 summarizes the ten countries with the highest incidence/burden of maternal deaths across the globe. Hypertensive disorders and hemorrhage further contribute to maternal deaths during pregnancy and childbirth.17 Worldwide, the annual number of maternal deaths has been on a decline. From nearly 600,000 women between the ages of 15 and 49 years dying each year as a result of pregnancy and childbirth-related complications with overwhelming majority in the developing nations in 1990,18 the annual number of maternal deaths has decreased since then by 43%, down to 303,000 in 2015.19,20 Despite declining maternal deaths, in developing nations, pre-existing conditions such as IDA are an important contributor to overall global maternal mortality, especially when it occurs in pregnancy. Maternal and neonatal mortality were responsible for 3.0 million deaths in 2013 to further contribute to overall global mortality.21 It has been estimated that 90,000 deaths in both sexes and all age groups are due to IDA alone.21
Effect of IDA on infant mortality and under 5 year mortality
Worldwide, mortality for children under age 5 years has been on a decline by almost 50% from 12.4 million in 1990 to 5.9 million in 2015.22 Despite the global decline, the number of deaths remain the highest in the neonatal period (the first 28 days of life). Causes of neonatal deaths include preterm birth complications (0.965 million, 15.4%) and intrapartum-related complications (0.662 million, 10.5%).23 Infectious diseases such as pneumonia and diarrhea (3.257 million, 51.8%) are the leading causes of mortality of children under 5 years of age. Newborn mortality currently accounts for 30–50% of all deaths among children younger than 5 years of age in Sub-Saharan Africa and South Asia.24,25,26,27 Table 3 summarizes the ten countries with the highest incidence/burden of infant mortality and under 5 mortality. According to WHO, The Democratic Republic of Congo, Ethiopia, India, Nigeria, and Pakistan collectively contributed to nearly 50% of the total number of global death under age 5 years (48.3%, 2.871 million) and neonatal deaths (50.8%, 1.3662 million) in 2015.22 Anemia contributes to child mortality through malnutrition and increased susceptibility to infection, especially in African and South-East Asian countries.13
Consequences of IDA
Effects of IDA on the developing brain
Both iron deficiency and anemia are associated with perinatal mortality, delayed child mental and physical development, and reduced visual and auditory function.28,29,30 Iron is critical for normal myelin synthesis.5 Myelin producing oligodendrocytes require iron for both maturation and function.31,32 Early iron deficiency adversely affects the developing brain through alteration in myelination and major dopamine pathways.33,34 Anemia affects intelligence, perhaps with irreversible and lifelong consequences on cognition, translating to the equivalent of a 5–10-point deficit in intelligence quotient.35 Moreover, IDA at an early age may be associated with permanent cognitive impairment, which may be irreversible even after repletion of iron stores.30,36 Lozoff and others have demonstrated that iron deficiency, aside from causing hematological abnormalities, has long-lasting neurocognitive impairment37,38 with adverse effects on infant psychomotor development.39,40 Iron has a critical role in both learning and memory including the speed of optimal brain processing.41 The developing hippocampus is especially vulnerable to early iron deficiency.41 One possible mechanism of the negative impact of iron deficiency on learning and memory is through abnormalities in hippocampal neuronal differentiation, reduction in metabolic activity, and altered gene expression in the rat hippocampus relative to other brain regions as demonstrated in a rodent model.41,42,43 Children and young adults with iron deficiency as infants showed poorer inhibitory control and executive functioning when assessed by neurocognitive tasks.33 Studies by Lozoff et al. and Walter et al. have shown that iron-deficient infants at ages 5 and 10 years consistently showed impaired cognitive development with a 5-point drop in intellectual quotient, lower school achievement, and poorer fine-hand movements.5,44
Effects of IDA on work productivity
Iron deficiency has been associated with reduced work capacity.4 Iron deficiency affects cognitive ability and skill acquisition, which in turn adversely impacts overall work productivity.45 The median annual economic loss because of IDA in 10 developing countries was estimated at $16.78 per capita (in 1994 US dollars), or 4% of gross domestic product.45 Fixing the problem of IDA in developing nations could result in a 20% increase in economic productivity over the life of an infant.36 As the iron status in an individual improves, the amount of physiological energy required to complete work-related task decreases. This results in increased physical fitness, less fatigue, more energy efficiency, and greater engagement in work-related activities.
Differences between iron deficiency and IDA
Iron deficiency is a state of reduction or depletion in iron stores. Untreated iron deficiency progresses to a state of IDA where the Hb concentrations are reduced and RBCs become hypochromic and microcytic. Anemia is most frequently assessed through measurement of blood Hb concentration on either capillary or venous blood. As Hb is known to have natural variation by age, sex, and physiological status (e.g., pregnancy), Hb concentration below established sex-, age-, and pregnancy-specific cut-off values is indicative of anemia.46 Measurement of Hb concentration is possible using relatively inexpensive equipment and does not require highly skilled individuals for testing. In addition, non-invasive methods of measuring Hb in newborn infants with using white light spectroscopy have been developed.47 For children aged 6–59 months, Hb concentration <11 g/l indicates anemia. In order to determine whether anemia is secondary to iron deficiency, one must monitor additional measures of iron status such as reticulocyte Hb, serum ferritin, serum transferrin receptor, total iron binding capacity, transferrin saturation, zinc protoporphyrin concentration, and erythrocyte protoporphyrin concentration. Reticulocyte Hb is a clinically useful marker for determining iron deficiency and hematological responses during iron administration48 and is an emerging biomarker as an alternative to biochemical iron studies in the diagnosis of IDA.49 There are newer regulators of iron homeostasis such as the hepatic peptide hormone hepcidin that are stimulated by inflammation.50 Serum hepcidin quantification assays are increasingly being used to both identify iron deficiency51 and determine intestinal absorption response to iron administration.52 It is important to remember that IDA is the final stage of iron deficiency and is not an early marker of iron deprivation.53 Figure 2 [adapted from the WHO54] illustrates the change in the different biochemical indices of iron status from normal to functional iron deficiency. It is also important to remember that, despite ferritin being recommended as the primary measure of iron status, interpretation of ferritin values are challenging in settings with infection and inflammation.55
Risk factors and causes of IDA
Understanding the etiology and risk factors for anemia is very important in order to execute effective and strategic interventions that control anemia prevalence. Risk factors for IDA in infants includes those in the perinatal and infancy period. Perinatal risk factors include maternal iron deficiency, prematurity, and perinatal hemorrhagic events, such as twin–twin transfusion or fetal–maternal hemorrhage. Specific neonatal populations at greatest risk factors for IDA include small-for-gestational-age infants, extremely low birth weight infants, and infants of diabetic mothers.
Infantile risk factors include (a) primarily dietary factors, such as prolonged exclusive breast-feeding in the absence of timely introduction of iron-rich complementary feeds,56 use of low-iron infant formula, feeding of unmodified (non-formula) cow’s milk, goat’s milk or soy milk, insufficient iron-rich complementary foods, and excessive intake of cow’s milk53 and (b) non-dietary risk factors include recurrent respiratory tract infections; chronic infections such as malaria and HIV; gastrointestinal (GI) malabsorptive diseases, including celiac disease, chronic intestinal infections/infestations, and disorders with GI blood loss such as milk protein-induced enterocolitis; hook worm infestation; and inflammatory bowel disease. A largely cereal-based diet rich in phytates, polyphenols, and other ligands that are known to inhibit intestinal iron absorption predominate in developing countries.57,58,59 The prevalence of anemia and IDA among infants aged 9–12 months from a random sample in Nablus Governorate, north of Jerusalem, was 34.6% and 32.6%.60 Predictors of IDA in this population were infant’s age, maternal anemia during the third trimester, birth spacing <3 years, exclusive breast feeding during the first 6 months, early and late introduction of complementary feeding, and non-compliance to iron supplement in the correct frequency and duration during pregnancy.
Preventive interventions to control IDA
Anemia-preventive strategies are effective when approached in an integrated, coordinated, and targeted manner. For any intervention that is aimed to successfully reduce the prevalence of IDA in infants, intervention strategies must focus on one or more of the following: identifying the different dietary and non-dietary risk factors for IDA, especially in pregnant women and their infants; establishing a cost-effective, readily accessible, easily affordable, and sustainable intervention in the less-developed regions of the world that can be widely delivered and distributed to the target population and readily made available through locally operated healthcare facilities; and simultaneously tackling the problem of inflammation associated with chronic infection and infestation such as malaria, vitamin A deficiency, and hookworm infestation.
Interventions in early infancy—delayed cord clamping (DCC)/umbilical cord milking (UCM)
Non-dietary intervention such as DCC targets early infantile anemia.61,62. DCC has a direct impact on preventing early infantile anemia by facilitating placental transfusion.63 Waiting to cut the umbilical cord until sufficient time (1–3 min) has elapsed to permit blood flow from placenta to newborn while the baby is transitioning to extra-uterine life has enormous benefits to the neonate. Currently, the umbilical cord is generally clamped within 15 s of birth.64 The newborn is then quickly transferred to the pediatric provider to avoid delayed resuscitation. Clamping the umbilical cord while significant circulation is still occurring through the umbilical vessels drops the cardiac output by about 40%.65 This deprives the newborn of the benefit of added circulating blood volume (up to 100 ml) from continuing placental transfusion. This relatively simple, inexpensive, and straightforward intervention of DCC when put into effective practice can save lives. Placental transfusion can also be accomplished by UCM or cord milking through a cut umbilical cord.66,67 Milking refers to the manual expression of blood from the umbilical cord by actively squeezing or milking blood down a short segment of umbilical cord (20–30 cm) that is either cut (cut cord) or attached (intact cord) to the placenta toward the baby 3–4 times at a rate of 10 cm/s before clamping the cord.68 UCM can serve as an alternative to DCC in situations of hypoxic term infant deliveries by simultaneously providing added blood volume from the accelerated process of placental transfusion and not jeopardize timely resuscitative efforts.66,67,68
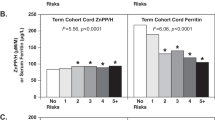
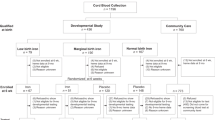
Impact of DCC on iron deficiency
A significant amount of iron-rich RBCs remains in the placental circulation when the cord is clamped early, depriving the newborn of iron-carrying RBCs. The greatest benefit of DCC is seen in children born at term to iron-deficient mothers and babies with birth weights of <3000 g.69 In term infants, a 1-min delay in cord clamping after birth led to additional volumes up to 80 ml of blood from the placenta to the infant’s circulation, which increased to 100 ml by 3 min after birth.70,71 Delaying cord clamping by around 3 min provides an additional 40 ml blood volume per Kg of body weight through placental transfusion with the potential to contribute up to 75 mg of iron in a baby weighing 3 Kg, thereby preventing iron deficiency in infant’s first 6 months of life.61,63,72,73,74,75 A large randomized controlled trial (RCT) in Mexico of 476 infants randomized to 2 min of DCC vs. early cord clamping demonstrated that a 2-min DCC increased 6-month iron stores by about 27–47 mg at 6 months of age.69
Higher Hb, hematocrit, and ferritin levels were observed after UCM in term and late-preterm infants when compared to immediate cord clamping group at 6 weeks of age.68,76,77 While UCM may serve as an alternative to DCC by providing equivalent benefits in term infants and not delaying timely resuscitation, in a post hoc analysis of a randomized clinical trial of UCM vs. DCC for 45–60 s among preterm infants born <32 weeks’ gestation, there was a statistically significant higher rate of severe intraventricular hemorrhage in the UCM group that led to early study termination.78 On the contrary, three other studies with similar study design in preterm infants did not find such a difference in rates of intraventricular hemorrhage in the UCM group.79,80,81 Further clinical trials are needed to investigate the potential benefits of DCC vs. UCM in preterm infants. Until then, extreme caution must be exercised while practicing UCM in the extremely preterm population.
Impact of DCC on IDA
DCC serves as a low-cost non-dietary intervention to reduce the risk for IDA.71,72,82 At 4 months, infants born at term receiving DCC had greater ferritin levels and increasing myelin in brain areas important for early life functional development.83 A positive association between maternal iron stores reflected in plasma ferritin concentration with infant plasma ferritin in the first 6 months has been observed.84 In a RCT of 276 mother–infant pairs, DCC at 3 min significantly increased serum ferritin levels in term infants at 6 months of age compared to early clamping group with a 3 times higher incidence of IDA among infants receiving early cord clamping.85 Moreover, DCC, when compared to early clamping, improved fine motor function at 4 years, indicating that optimizing the time to cord clamping has a positive impact on neurodevelopment.28 Full-term infants benefit from increased Hb, increased iron stores, and better motor outcomes at 4 years of age.2,14,15,16 The WHO recommends delayed clamping of the umbilical cord to reduce infant anemia.82 DCC serves as a means to deliver iron, potentially reducing or eliminating the cost of iron supplements.70 As an alternative to DCC, keeping the umbilical cord long and milking may be an effective method for improving Hb and iron stores at 6 months of age in term infants. Higher ferritin levels were observed at 6 months of age in the UCM group, regardless of maternal anemia status, compared to the immediate cord clamping group.86 Thereafter, both DCC and UCM interventions are particularly relevant for infants living in low-resource settings or in settings with less access to iron-rich foods and thus greater risk of anemia.
Preterm infants have the added benefit of a 27% increase in survival rate if they receive DCC at birth.62 In these infants, DCC enables a better transition to extrauterine life by increasing blood pressure and reducing the need for volume therapy, blood transfusions, and inotropes. Owing to additional iatrogenic blood losses, preterm infants benefit thereafter from a combination strategy of DCC, limited phlebotomy blood sampling, and early introduction to adequate protein and iron supply to boost endogenous erythropoiesis. Iron supplementation starting from the early neonatal period has been shown to be beneficial to both preterm and term infants. A combined approach of a 30-s DCC, early protein and iron supplementation (6 mg/kg from days 7 to 10 of life), and change to a restrictive transfusion threshold resulted in a reduced number of RBC transfusions by half in preterm infants <32 weeks’ gestational age and <1500 g birth weight population.87 In a randomized interventional trial, early supplementation of iron at a dose of 2 mg/kg from the second day after birth improved both iron status and motor development at 6 months in term infants at risk for early iron deficiency compared with the no iron-supplementation group.88
Impact of DCC on maternal health
Postpartum hemorrhage (PPH), is defined as a blood loss of ≥500 ml within 24 h after birth. Reduction in PPH risk directly impacts maternal health.89 According to WHO, PPH is associated with nearly one-quarter of all maternal deaths globally and is the leading cause of maternal mortality in most low-income countries.90 As anemia contributes to 20% of all maternal deaths, PPH is a burden for anemic mothers in the perinatal period. Any intervention that reduces the risk of PPH could impact maternal morbidity and mortality.89 Most PPH is avoidable through timely and appropriate management of the third stage of labor, which begins after the birth of the baby and ends with delivery of the placenta and fetal membranes. There appears to be no risk to the mother of a delay of 1–3 min to clamping the umbilical cord, and this practice could potentially prevent the mother from becoming anemic during the third stage of labor by facilitating optimal delivery of the placenta and reducing the risk of PPH.91,92 Studies have shown that the incidence of PPH is not increased with DCC for 1–3 min.71,93,94 The 2012 WHO guidelines for the management of PPH strongly endorse DCC for all infants who do not require immediate resuscitation after both vaginal and cesarean births.90
Despite endorsements by numerous governing bodies (Table 4), including the WHO, the American Academy of Pediatrics, the American College of Obstetrics and Gynecology, the European Association of Perinatal Medicine, the Society of Obstetricians and Gynecologists of Canada, the Royal College of Obstetricians and Gynaecologists, and the International Liaison Committee on Resuscitation, the practice of DCC has been slow to be adopted.95 In a review by Anton et al., reported barriers and strategic methods to improve placental transfusion protocol were closely examined.95 Preferred methods of successful implementation of DCC to establish placental transfusion include protocol development and targeted education of the stakeholders involved in obstetric and pediatric practice through simulation exercises, as well as feedback and auditing of placental transfusion practice through quality improvement projects.96,97,98,99
Interventions in late infancy and toddlers—iron fortification
Despite the observed protection against early infantile iron deficiency from placental transfusion of maternal iron stores, prevalence of anemia continues to remain high among infants aged 7–12 months. In maternal–infant pairs from a peri-urban municipality in Nepal,84 prevalence of anemia among infants aged 7–12 months was 72% (Hb <11.3 g/dl). According to WHO, while infants should be exclusively breastfed for the first 6 months of life, beyond 6 months, infants should receive nutritionally adequate and safe complementary foods, to achieve optimal growth and development.54
There is a major global nutrition effort to decrease IDA through the provision of iron fortified food. Iron deficiency can be treated with dietary oral iron supplementation, intravenous iron therapy, and/or red cell transfusion, depending on the patient’s Hb status and underlying co-morbid illness. Dietary intervention with iron supplementation and fortification of infant food with iron addresses late infantile anemia. Iron is considered an essential dietary component and is necessary for development and health. The recommended dietary allowance for total iron intake (mg/d) during early infancy (0–6 months) is 0.27 mg/day and late infancy (7–12 months) is 11 mg/day.100,101 Dietary iron is a widely administered supplement for pregnant women and is a key ingredient in infant formulas. Food items that are rich in iron content include liver, legumes, beans, nuts, green leafy vegetables, and fortified cereals but have very variable bio-absorption.58 Daily oral iron supplementation is a commonly recommended intervention both for treatment and prevention of anemia related to iron deficiency. In an effort to prevent infantile anemia, WHO recommends use of fortified foods or home fortificants such as micronutrient powders or lipid-based nutrient supplements for feeding non-breastfed children 6–24 months of age.102 Iron supplementation has been shown to benefit infants with the poorest iron status.54 Moreover, healthy full-term un-supplemented infants at 12 months of age showed less positive response to both physical and social environment compared to the iron-supplemented group in the first year of life after initiating iron supplementation from 6 months of age.103 This study highlights the potential for reversing a preventable intellectual deficit from iron deficiency if oral iron supplementation is started early in infancy.
Measures of successful oral iron supplementation and improvement of maternal–infant iron stores
The WHO recommends daily iron supplementation as a public health intervention in infants and young children aged 6–23 months, living in settings where the prevalence of anemia is ≥40% in order to prevent iron deficiency and anemia.54 Suggested schemes include daily iron supplement of 10–12.5 mg elemental iron either as drops or syrup for 3 consecutive months per year. The WHO also recommends a supervised provision of iron supplementation in malaria-endemic areas in conjunction with local public measures to prevent, diagnose, and treat malaria.104 In Venezuela, the prevalence of anemia in children aged 7, 11, and 15 years decreased by 50% within 12 months of introduction of iron fortification of flours that included precooked maize and white wheat.105
Improvement of maternal iron stores in women of reproductive age group is vital in order to improve pregnancy outcomes for mothers and infants.54 Iron supplementation during pregnancy increases maternal and fetal iron stores with >66% of the infant’s total body iron being acquired during the final trimester of pregnancy.106 The WHO recommends daily oral iron and folic acid supplementation with 30–60 mg of elemental iron and 400 µg (0.4 mg) folic acid for pregnant women and adolescent girls to prevent maternal anemia, puerperal sepsis, low birth weight, and preterm birth.107 A small iron cooking tool such as the Lucky Iron Fish that infuses meals with iron can serve as an alternative to help prevent iron deficiency and anemia, especially in conditions when iron-fortified diet is neither affordable nor possible, and supplements are expensive, not consistently available, and often culturally unacceptable.108 Lucky Iron Fish are fish-shaped cast iron ingots. The ingots are placed in a pot of boiling water to leach elemental iron into the water and food. The ingots provide dietary supplementation of iron to individuals affected by IDA when used as directed during the cooking process. Lucky Iron Fish can restore circulating and stored levels of iron and reduces the prevalence of anemia by ∼43%.108
Improvements in the prevalence of anemia among women of reproductive age through successful implementation strategies are being observed globally. In Viet Nam, the prevalence of anemia fell from 38% at baseline to 19% after 12 months of weekly iron–folic supplementation in conjunction with de-worming among women of reproductive age 15–45 years. Furthermore, continued use of this program intervention led to elimination of IDA in Venezuela as the prevalence of IDA fell further from 18% to 4% at 54 months post-implementation.109 In India, evaluation of a pilot program of weekly iron–folic supplementation to over 1.2 million adolescent girls led to reduction in the prevalence of anemia from 74.2% to 53.5% within 1 year, with estimated compliance >90%.110 A universal iron-supplementation strategy was effective in reducing the prevalence of anemia among low-income postpartum women across 11 health clinics in Mississippi. The prevalence of anemia among low-income postpartum women (Hb < 12.0 g/dl) dropped from 52% to 33% at 6 months after the intervention.50 In Thailand, between 1986 and 1996/97, anemia prevalence reduced by 50% in pregnant women through provision of free iron and folic supplementation.111 The above studies demonstrate that population-based interventions can efficiently and effectively reduce anemia but requires cooperation of the local health authorities besides nutritional education of the community.
Despite universal iron-supplementation strategy being effective in reducing the prevalence of anemia among low-income postpartum women, challenges remain in the preschool population. The global burden of anemia remains high especially in low-income settings of Africa and parts of Asia even after distribution of iron. Anemia prevalence continues to be high among infants and preschoolers in India.11 In India, the current anemia prevalence among preschool aged children (0–4.99 years) and pregnant mothers (15–49 years) is 59% and 54%, respectively. Various cost-effective interventions and policies including the National Nutrition Policy, Integrated Child Development Services, Mid-day Meal Programme, and other initiatives under National Rural Health Mission are currently being implemented that facilitates prevention and control of anemia in infants and women of reproductive age.
Risks of routine iron supplementation
There are concerns of potential adverse effects to children from iron-supplementation regimens, such as increased risk for malarial parasitemia in malaria-endemic regions.35 It has been shown that iron deficiency offers protection against malaria infection, although the precise mechanism of this protective benefit remains unknown.112,113 In a meta-analysis of 68 trials, Ojukwu et al. showed that iron does not increase the risk of clinical malaria or death, when regular malaria surveillance and treatment services are provided.114 Regardless, guidelines for iron supplementation that will provide greatest benefit with least harm in areas with high malaria prevalence requires further clarification. There is also an added urgency to clarify the safety of iron supplementation and fortification where inherited Hb disorders are highly prevalent. Currently, WHO does not offer guidelines on iron supplementation in settings of inherited red cell disorders and other hemoglobinopathies. The safety of long-term iron supplementation in inherited Hb disorders, a population at risk for iron overload, has not been established. Other risks of oral iron supplementation include GI side effects including vomiting in up to 50% of adult patients leading to reduced tolerance and adherence to iron supplementation.115,116 Based on a systematic review, extended release ferrous sulfate with mucoproteose appeared to be the best tolerated of the several oral iron supplements evaluated by the study group.116 Newer innovative oral iron formulation such as sucrosomial iron with its protective phospholipid bilayer that offers higher iron bioavailability and improved GI tolerance are emerging.117
Conclusion
In summary, anemia reduction interventions in neonates, infants, and toddlers must start with:
(1) Universal implementation of delayed umbilical cord clamping; (2) In populations where anemia is a public health problem, providing point-of-use fortification of complementary foods with iron-containing micronutrient powders to infants and preschool children; (3) Control of inflammation through prevention and treatment of HIV, malaria, and helminthic infections in children aged under 3 years; (4) Counseling of pregnant women on optimal dietary practices and (5) Raising awareness of anemia-prevention programs through (a) community participation, (b) strengthening of various existing preventive programs through integration and coordination, (c) sustained training and surveillance of healthcare workers, and (d) increase compliance among beneficiaries through public–private partnerships.
IDA continues to be a major contributor to overall anemia prevalence worldwide. Limited health services undeniably are a major factor for high maternal and perinatal mortality in resource-limited settings. Public intervention strategies must consider the various factors associated with anemia before designing intervention studies to reduce anemia prevalence. Anemia-preventive strategies are effective when approached in an integrated, coordinated, and targeted manner. Collaborative partnerships from governmental and non-governmental organizations and local communities are vital to achieving successful reduction of the prevalence of anemia in infants and toddlers.
References
United Nations World Health Organization. Iron Deficiency Anaemia: Assesment, Prevention and Control: a Guide for Programme Managers (World Health Organization, 2001).
World Health Organization. The Global Prevalence of Anaemia in 2011 (WHO, 2015).
Beutler, E. & Waalen, J. The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood 107, 1747–1750 (2006).
Haas, J. D. & Brownlie, T. t. Iron deficiency and reduced work capacity: a critical review of the research to determine a causal relationship. J. Nutr. 131, 676S–688S (2001). Discussion 688S–690S.
Walter, T. Effect of iron-deficiency anemia on cognitive skills and neuromaturation in infancy and childhood. Food Nutr. Bull. 24, S104–S110 (2003).
De Benoist, B., Cogswell, M., Egli, I. & McLean, E. Worldwide prevalence of anaemia 1993-2005 (WHO Global Database of Anaemia, 2008).
McLean, E., Cogswell, M., Egli, I., Wojdyla, D. & de Benoist, B. Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993-2005. Public Health Nutr. 12, 444–454 (2009).
Hadler, M. C., Juliano, Y. & Sigulem, D. M. [Anemia in infancy: etiology and prevalence]. J. Pediatr. (Rio J.) 78, 321–326 (2002).
Kotecha, P. V. Nutritional anemia in young children with focus on Asia and India. Indian J. Community Med. 36, 8–16 (2011).
Stevens, G. A. et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995-2011: a systematic analysis of population-representative data. Lancet Glob. Health 1, e16–e25 (2013).
Nair, K. M. et al. Characterisation of anaemia and associated factors among infants and pre-schoolers from rural India. Public Health Nutr. 19, 861–871 (2015).
World Health Organization. Global Nutriton Targets 2025: Anaemia Policy Brief (World Health Organization, Geneva, 2014).
Stoltzfus, R. J., Mullany, L. & Black, R. E. in Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors (eds Ezzati, M., Lopez, A. D., Rodgers, A. & Murray, C. J. L.) Ch. 3 (World Health Organization, Geneva, 2004).
Kozuki, N., Lee, A. C., Katz, J., & Child Health Epidemiology Reference Group. Moderate to severe, but not mild, maternal anemia is associated with increased risk of small-for-gestational-age outcomes. J. Nutr. 142, 358–362 (2012).
Zhang, Q., Ananth, C. V., Rhoads, G. G. & Li, Z. The impact of maternal anemia on perinatal mortality: a population-based, prospective cohort study in China. Ann. Epidemiol. 19, 793–799 (2009).
Steer, P. J. Maternal hemoglobin concentration and birth weight. Am. J. Clin. Nutr. 71, 1285S–1287S (2000).
Bauserman, M. et al. Risk factors for maternal death and trends in maternal mortality in low- and middle-income countries: a prospective longitudinal cohort analysis. Reprod. Health Suppl 2, S5 (2015).
World Health Organization. Reduction of Maternal Mortality: A Joint WHO/UNFPA/UNICEF/World Bank Statement (WHO, 1999).
Gulmezoglu, A. M. et al. in Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities 3rd edn, Vol. 2 (eds Black, R. E., Laxminarayan, R., Temmerman, M. & Walker, N.) Ch. 7 (World Bank, Washington, DC, 2016).
World Health Organization & UNICEF. Trends in Maternal Mortality: 1990-2015: Estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division (WHO, 2015).
World Health Organization. Global Health Estimates 2014 Summary Tables: Deaths by Cause, Age and Sex, by WHO Region, 2000-2012 (World Health Organization Geneva, 2014).
Liu, L. et al. in Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities 3rd edn, Vol. 2 (eds Black, R. E., Laxminarayan, R., Temmerman, M. & Walker, N.) Ch. 4 (Washington, DC, 2016).
Liu, L. et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 385, 430–440 (2015).
Bhutta, Z. A. & Black, R. E. Global maternal, newborn, and child health-so near and yet so far. N. Engl. J. Med. 369, 2226–2235 (2013).
Lozano, R. et al. Progress towards millennium development goals 4 and 5 on maternal and child mortality: an updated systematic analysis. Lancet 378, 1139–1165 (2011).
UNICEF. Levels and Trends in Child Mortality: Report 2011. Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation (United Nation’s Children Fund, New York, 2011).
Liu, L. et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379, 2151–2161 (2012).
Andersson, O. et al. Effect of delayed cord clamping on neurodevelopment at 4 years of age: a randomized clinical trial. JAMA Pediatr. 169, 631–638 (2015).
Algarin, C., Peirano, P., Garrido, M., Pizarro, F. & Lozoff, B. Iron deficiency anemia in infancy: long-lasting effects on auditory and visual system functioning. Pediatr. Res. 53, 217–223 (2003).
Lozoff, B., Jimenez, E. & Smith, J. B. Double burden of iron deficiency in infancy and low socioeconomic status: a longitudinal analysis of cognitive test scores to age 19 years. Arch. Pediatr. Adolesc. Med. 160, 1108–1113 (2006).
Connor, J. R. & Menzies, S. L. Relationship of iron to oligodendrocytes and myelination. Glia 17, 83–93 (1996).
Todorich, B., Pasquini, J. M., Garcia, C. I., Paez, P. M. & Connor, J. R. Oligodendrocytes and myelination: the role of iron. Glia 57, 467–478 (2009).
Lozoff, B. Early iron deficiency has brain and behavior effects consistent with dopaminergic dysfunction. J. Nutr. 141, 740S–746S (2011).
Beard, J. L. & Connor, J. R. Iron status and neural functioning. Annu. Rev. Nutr. 23, 41–58 (2003).
Pasricha, S.-R., Drakesmith, H., Black, J., Hipgrave, D. & Biggs, B.-A. Control of iron deficiency anemia in low-and middle-income countries. Blood 121, 2607–2617 (2013).
Organization WH. Guideline: Intermittent Iron Supplementation in Preschool and School-age Children (World Health Organization, Geneva, 2011).
Lozoff, B. et al. Iron deficiency anemia and iron therapy effects on infant developmental test performance. Pediatrics 79, 981–995 (1987).
Lozoff, B., Jimenez, E. & Wolf, A. W. Long-term developmental outcome of infants with iron deficiency. N. Engl. J. Med. 325, 687–694 (1991).
Walter, T., De Andraca, I., Chadud, P. & Perales, C. G. Iron deficiency anemia: adverse effects on infant psychomotor development. Pediatrics 84, 7–17 (1989).
De Andraca, I. et al. Iron Deficiency Anemia and its Effects upon Psychological Development at Preschool Age: A Longitudinal Study. Nestle Foundation Annual Report: 53–62 (Nestle Foundation, 1990).
Fretham, S. J., Carlson, E. S. & Georgieff, M. K. The role of iron in learning and memory. Adv. Nutr. 2, 112–121 (2011).
deUngria, M. et al. Perinatal iron deficiency decreases cytochrome c oxidase (CytOx) activity in selected regions of neonatal rat brain. Obstet. Gynecol. Surv. 56, 191–193 (2001).
Rao, R., Tkac, I., Townsend, E. L., Gruetter, R. & Georgieff, M. K. Perinatal iron deficiency alters the neurochemical profile of the developing rat hippocampus. J. Nutr. 133, 3215–3221 (2003).
Lozoff, B. Methodologic issues in studying behavioral effects of infant iron-deficiency anemia. Am. J. Clin. Nutr. 50, 641–651 (1989). discussion 652-644.
Horton, S. & Ross, J. The economics of iron deficiency. Food Pol. 28, 51–75 (2003).
World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity (World Health Organization, 2011).
Rabe, H., Alvarez, R. F., Whitfield, T., Lawson, F. & Jungmann, H. Spectroscopic noninvasive measurement of hemoglobin compared with capillary and venous values in neonates. Neonatology. 98, 1–5 (2010).
Toki, Y. et al. Reticulocyte hemoglobin equivalent as a potential marker for diagnosis of iron deficiency. Int. J. Hematol. 106, 116–125 (2017).
Brugnara, C., Zurakowski, D., DiCanzio, J., Boyd, T. & Platt, O. Reticulocyte hemoglobin content to diagnose iron deficiency in children. JAMA 281, 2225–2230 (1999).
Mitra, A. K. & Khoury, A. J. Universal iron supplementation: a simple and effective strategy to reduce anaemia among low-income, postpartum women. Public Health Nutr. 15, 546–553 (2012).
Pasricha, S. R. et al. Expression of the iron hormone hepcidin distinguishes different types of anemia in African children. Sci. Transl. Med. 6, 235re233 (2014).
Young, M. F. et al. Serum hepcidin is significantly associated with iron absorption from food and supplemental sources in healthy young women. Am. J. Clin. Nutr. 89, 533–538 (2009).
Powers, J. M. & Buchanan, G. R. Diagnosis and management of iron deficiency anemia. Hematol. Oncol. Clin. North Am. 28, 729–745 (2014).
World Health Organization. Nutritional Anaemias: Tools for Effective Prevention and Control (WHO, 2017).
Namaste, S. M. et al. Adjusting ferritin concentrations for inflammation: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am. J. Clin. Nutr. 106, 359S–371S (2017).
Meinzen-Derr, J. K. et al. Risk of infant anemia is associated with exclusive breast-feeding and maternal anemia in a Mexican cohort. J. Nutr. 136, 452–458 (2006).
Hallberg, L., Rossander, L. & Skanberg, A. B. Phytates and the inhibitory effect of bran on iron absorption in man. Am. J. Clin. Nutr. 45, 988–996 (1987).
Lynch, S. et al. Biomarkers of Nutrition for Development (BOND)-iron review. J. Nutr. 148, 1001S–1067S (2018).
Gibson, R. S., Bailey, K. B., Gibbs, M. & Ferguson, E. L. A review of phytate, iron, zinc, and calcium concentrations in plant-based complementary foods used in low-income countries and implications for bioavailability. Food Nutr. Bull. 31, S134–S146 (2010).
Hasab, A. A., El-Nimr, N. A. & Tayel, D. I. The Prevalence and Predictors of Iron Deficiency Anemia among Rural Infants in Nablus Governorate. J. Res. Health Sci. 18 (2018).
McDonald, S. J., Middleton, P., Dowswell, T. & Morris, P. S. Cochrane in context: effect of timing of umbilical cord clamping in term infants on maternal and neonatal outcomes. EBCH: A Cochrane Rev. J. 9, 398–400 (2014).
Rabe, H., Gyte, G. M., Díaz‐Rossello, J. L. & Duley, L. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst. Rev. 2019.
Pisacane, A. Neonatal prevention of iron deficiency. BMJ 312, 136–137 (1996).
Kim, A. J. & Warren, J. B. Optimal timing of umbilical cord clamping: is the debate settled? Part 2 of 2: Evidence in preterm and term infants, alternatives, and unanswered questions. Neoreviews 16, e270–e277 (2015).
Raju, T. N. Don’t rush to cut the cord: new recommendations call for delaying cord clamping in preterm infants. AAP News 34, 17–17 (2013).
Katheria, A. C., Brown, M. K., Rich, W. & Arnell, K. Providing a placental transfusion in newborns who need resuscitation. Front. Pediatr. 5, 1 (2017).
Katheria, A. C., Lakshminrusimha, S., Rabe, H., McAdams, R. & Mercer, J. S. Placental transfusion: a review. J. Perinatol. 37, 105–111 (2017).
Basile, S., Pinelli, S., Micelli, E., Caretto, M. & Benedetti Panici, P. Milking of the umbilical cord in term and late preterm infants. Biomed. Res. Int. 2019, 9185059 (2019).
Chaparro, C. M., Neufeld, L. M., Tena Alavez, G., Eguia-Liz Cedillo, R. & Dewey, K. G. Effect of timing of umbilical cord clamping on iron status in Mexican infants: a randomised controlled trial. Lancet 367, 1997–2004 (2006).
Mercer, J. & Erickson-Owens, D. Delayed cord clamping increases infants’ iron stores. Lancet 367, 1956–1958 (2006).
World Health Organization. Guideline: Delayed Umbilical Cord Clamping for Improved Maternal and Infant Health and Nutrition Outcomes (World Health Organization, 2014).
Kc, A. et al. Effects of delayed umbilical cord clamping vs early clamping on anemia in infants at 8 and 12 months: a randomized clinical trial. JAMA Pediatr. 171, 264–270 (2017).
Andersson, O., Hellstrom-Westas, L., Andersson, D. & Domellof, M. Effect of delayed versus early umbilical cord clamping on neonatal outcomes and iron status at 4 months: a randomised controlled trial. BMJ 343, d7157 (2011).
Hutton, E. K. & Hassan, E. S. Late vs early clamping of the umbilical cord in full-term neonates: systematic review and meta-analysis of controlled trials. JAMA 297, 1241–1252 (2007).
DuPont, T. L. & Ohls, R. K. Placental transfusion: current practices and future directions. Neoreviews 19, e1–e10 (2018).
Upadhyay, A. et al. Effect of umbilical cord milking in term and near term infants: randomized control trial. Am. J. Obstet. Gynecol. 208, 120.e1–120.e6. (2013).
Kumar, B. et al. Umbilical cord milking and hematological parameters in moderate to late preterm neonates: a randomized controlled trial. Indian Pediatr. 52, 753–757 (2015).
Katheria, A. et al. Association of umbilical cord milking vs delayed umbilical cord clamping with death or severe intraventricular hemorrhage among preterm infants. JAMA 322, 1877–1886 (2019).
Shirk, S. K., Manolis, S. A., Lambers, D. S. & Smith, K. L. Delayed clamping vs milking of umbilical cord in preterm infants: a randomized controlled trial. Am. J. Obstet. Gynecol. 220, 482 e481–482. e488 (2019).
Rabe, H. et al. Milking compared with delayed cord clamping to increase placental transfusion in preterm neonates: a randomized controlled trial. Obstet. Gynecol. 117, 205–211 (2011).
Katheria, A. C., Truong, G., Cousins, L., Oshiro, B. & Finer, N. N. Umbilical cord milking versus delayed cord clamping in preterm infants. Pediatrics 136, 61–69 (2015).
World Health Organization. Delayed Clamping of the Umbilical Cord to Reduce Infant Anaemia (WHO, 2014).
Mercer, J. S. et al. Effects of delayed cord clamping on 4-month ferritin levels, brain myelin content, and neurodevelopment: a randomized controlled trial. J. Pediatr. 203, 266.e2–272.e2 (2018).
Chandyo, R. K. et al. The prevalence of anemia and iron deficiency is more common in breastfed infants than their mothers in Bhaktapur, Nepal. Eur. J. Clin. Nutr. 70, 456–462 (2016).
Ceriani, J. C. et al. The effect of early and delayed umbilical cord clamping on ferritin levels in term infants at six months of life: a randomized, controlled trial. Arch. Argentinos Pediatr. 108, 201–208 (2010).
Bora, R., Akhtar, S. S., Venkatasubramaniam, A., Wolfson, J. & Rao, R. Effect of 40-cm segment umbilical cord milking on hemoglobin and serum ferritin at 6 months of age in full-term infants of anemic and non-anemic mothers. J. Perinatol. 35, 832–836 (2015).
Rabe, H., Alvarez, J. R., Lawn, C., Seddon, P. & Amess, P. N. A management guideline to reduce the frequency of blood transfusion in very-low-birth-weight infants. Am. J. Perinatol. 26, 179–183 (2009).
Bora, R., Ramasamy, S., Brown, B., Wolfson, J. & Rao, R. Effect of iron supplementation from neonatal period on the iron status of 6-month-old infants at-risk for early iron deficiency: a randomized interventional trial. J. Matern. Fetal Neonatal Med. 1–9 (2019).
Kavle, J. A. et al. Association between anaemia during pregnancy and blood loss at and after delivery among women with vaginal births in Pemba Island, Zanzibar, Tanzania. J. Health Popul. Nutr. 26, 232–240 (2008).
WHO. WHO Recommendations for the Prevention and Treatment of Postpartum Haemorrhage (World Health Organization, Geneva, 2012).
Soltani, H., Dickinson, F., Symonds, I. & Soltani, H. Placental cord drainage after spontaneous vaginal delivery as part of the management of the third stage of labour. Cochrane Database Syst. Rev. CD004665 (2005).
Shravage, J. & Silpa, P. Randomized controlled trial of placental blood drainage for the prevention of postpartum hemorrhage. J. Obstet. Gynecol. India 57, 213–215 (2007).
Purisch, S. E. et al. Effect of delayed vs immediate umbilical cord clamping on maternal blood loss in term cesarean delivery: a randomized clinical trial. JAMA 322, 1869–1876 (2019).
Andersson, O., Hellstrom-Westas, L., Andersson, D., Clausen, J. & Domellof, M. Effects of delayed compared with early umbilical cord clamping on maternal postpartum hemorrhage and cord blood gas sampling: a randomized trial. Acta Obstet. Gynecol. Scand. 92, 567–574 (2013).
Anton, O., Jordan, H. & Rabe, H. Strategies for implementing placental transfusion at birth: a systematic review. Birth 46, 411–427 (2018).
McAdams, R. M., Backes, C. H. & Hutchon, D. J. Steps for implementing delayed cord clamping in a hospital setting. Matern Health Neonatol. Perinatol. 1, 10 (2015).
Bacon, P. L., Johnson, C. T., Frank, K., Diaz, J., Bullard, J. E. & Jelin, A. C. Implementation of delayed cord clamping in premature neonates. Reprod. Sci. 24, 246A (2017).
Bolstridge, J. et al. A quality improvement initiative for delayed umbilical cord clamping in very low-birthweight infants. BMC Pediatr. 16, 155 (2016).
Perrone, B., Ghirardello, S. & Italian Survey on Placental Transfusion Group. Placental transfusion strategies in Italy: a nationwide survey of tertiary-care delivery wards. Am. J. Perinatol. 34, 722–728 (2017).
Russell, R. et al. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. A Report of the Panel on Micronutrients, Subcommittees on Upper Reference Levels of Nutrients and of Interpretation and Uses of Dietary Reference Intakes, and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes Food and Nutrition Board Institute of Medicine (National Academies Press, Washington, DC, 2001).
Zlotkin, S. Clinical nutrition: 8. The role of nutrition in the prevention of iron deficiency anemia in infants, children and adolescents. CMAJ 168, 59–63 (2003).
World Health Organization. Guiding Principles for Feeding Non-breastfed Children 6-24 Months of Age (WHO, 2005).
Lozoff, B. et al. Behavioral and developmental effects of preventing iron-deficiency anemia in healthy full-term infants. Pediatrics 112, 846–854 (2003).
WHO. Iron Supplementation of Young Children in Regions Where Malaria Transmission is Intense and Infectious Disease is Highly Prevalent (WHO, 2006).
García-Casal, M. N. & Layrisse, M. Iron fortification of flours in Venezuela. Nutr. Rev. 60, S26–S29 (2002).
Scholl, T. O. Maternal iron status: relation to fetal growth, length of gestation, and iron endowment of the neonate. Nutr. Rev. 69(Suppl 1), S23–S29 (2011).
World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience (World Health Organization, 2016).
Armstrong, G. R. The Lucky Iron Fish: a simple solution for iron deficiency. Blood Adv. 1, 330–330 (2017).
Casey, G. J. et al. Elimination of iron deficiency anemia and soil transmitted helminth infection: evidence from a fifty-four month iron-folic acid and de-worming program. PLoS Negl. Trop. Dis. 7, e2146 (2013).
UNICEF. The Adolescent Girls Anaemia Control Programme: Breaking the Inter-generational Cycle of Undernutrition in India with a Focus on Adolescent Girls. Briefing Paper Series: Innovations, Lessons and Good Practices (UNICEF, New York, 2011).
Galloway, R & Galloway, R. Anemia Prevention and Control: What Works. Part I: Program Guidance. Report Number 56174 (World Bank, Washington, DC, 2003).
Kabyemela, E. R., Fried, M., Kurtis, J. D., Mutabingwa, T. K. & Duffy, P. E. Decreased susceptibility to Plasmodium falciparum infection in pregnant women with iron deficiency. J. Infect. Dis. 198, 163–166 (2008).
Gwamaka, M. et al. Iron deficiency protects against severe Plasmodium falciparum malaria and death in young children. Clin. Infect. Dis. 54, 1137–1144 (2012).
Ojukwu, J. U., Okebe, J. U., Yahav, D. & Paul, M. Oral iron supplementation for preventing or treating anaemia among children in malaria-endemic areas. Cochrane Database Syst. Rev. CD006589 (2009).
Tolkien, Z., Stecher, L., Mander, A. P., Pereira, D. I. & Powell, J. J. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS ONE 10, e0117383 (2015).
Cancelo-Hidalgo, M. J. et al. Tolerability of different oral iron supplements: a systematic review. Curr. Med. Res. Opin. 29, 291–303 (2013).
Gomez-Ramirez, S., Brilli, E., Tarantino, G. & Munoz, M. Sucrosomial((R)) iron: a new generation iron for improving oral supplementation. Pharmaceuticals (Basel) 11, 97 (2018).
Stoltzfus, R. J. Iron deficiency: global prevalence and consequences. Food. Nutr. Bull. 24 (4_suppl_1), S99–S103 (2003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sundararajan, S., Rabe, H. Prevention of iron deficiency anemia in infants and toddlers. Pediatr Res 89, 63–73 (2021). https://doi.org/10.1038/s41390-020-0907-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0907-5
This article is cited by
-
Relationship between the natural cessation time of umbilical cord pulsation in full-term newborns delivered vaginally and maternal-neonatal outcomes: a prospective cohort study
BMC Pregnancy and Childbirth (2024)
-
Synthesis of Di(thiophen-2-yl) Substituted Pyrene-Pyridine Conjugated Scaffold and DFT Insights: A Selective and Sensitive Colorimetric, and Ratiometric Fluorescent Sensor for Fe(III) Ions
Journal of Fluorescence (2024)
-
Challenges in the management of iron-deficiency anemia in Senegal, West Africa
Annals of Hematology (2024)
-
Iron nanoparticles as food additives and food supplements, regulatory and legislative perspectives
Food Science and Biotechnology (2024)
-
Alkaline and acidic soil constraints on iron accumulation by Rice cultivars in relation to several physio-biochemical parameters
BMC Plant Biology (2023)