Abstract
Converging evidence points to the significant involvement of the immune system in autism spectrum disorders (ASD). Positron emission tomography (PET) can quantify translocator protein 18 kDa (TSPO), a marker with increased expression mainly in microglia and, to some extent astroglia during neuropsychiatric diseases with inflammation. This preliminary analysis explored, for the first time, whether TSPO binding was altered in male and female participants with ASD in vivo using full kinetic quantification. Thirteen individuals with ASD (IQ > 70 [n = 12], IQ = 62 [n = 1]), 5 F, 25 ± 5 years) were scanned with [18F]FEPPA PET. Data from 13 typically developing control participants with matching age and TSPO rs6971 polymorphism (9 F, age 24 ± 5 years) were chosen from previous studies for comparison. The two tissue compartment model (2TCM) was used to determine the total volume of distribution ([18F]FEPPA VT) in four previously identified regions of interest (ROI): prefrontal, temporal, cerebellar, and anterior cingulate cortices. We observe no significant difference in [18F]FEPPA VT relative to controls (F(1,26)= 1.74, p = 0.20). However, 2 ASD participants with higher VT had concurrent major depressive episodes (MDE), which has been consistently reported during MDE. After excluding those 2 ASD participants, in a post-hoc analysis, our results show lower [18F]FEPPA VT in ASD participants compared to controls (F(1,24)= 6.62, p = 0.02). This preliminary analysis provides evidence suggesting an atypical neuroimmune state in ASD.
Similar content being viewed by others
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder with an onset early in development and is defined by social communication deficits and repetitive and restricted behaviors and interests [1]. Individuals with ASD often portray difficulties with nonverbal communication involving decreased eye contact, facial expression, and body movements [2]. ASD is more prevalent among boys [3], highly heritable [4] with a significant genetic component [5], and relatively common, with 1 in 40 children diagnosed in the United States [6, 7].
Although genetic studies have suggested more than 100 ASD [8] related genes, and neuroimaging studies have shown widespread anomalies in brain structure, function, and connectivity [9], we have yet to identify active disease brain biomarkers that could be used to develop disease-modifying interventions. Convergent evidence strongly indicates the role of neuroinflammation as an etiopathogenic pathway to ASD [10]. Numerous findings indicate that peripheral immune dysregulation and neuroinflammation remain in adulthood in ASD [10]. Biological evidence of immune activation has led to several immune-modulating agents being examined as potential disease-modifying treatments for ASD [9]. For example, celecoxib, a cyclooxygenase-2 (COX-2) inhibitor nonsteroidal anti-inflammatory drug, documented to be effective in a small clinical trial, and to improve symptoms in children with ASD when administered as an adjunct to risperidone [11].
Recent data indicate that ASD-linked human leukocyte antigen (HLA) genes (involved in immune processes) may contribute to ASD risk through their role in the regulation of synapse density and neural connectivity in the developing brain [12]. Convergent lines of evidence, therefore, indicate that certain genetic and environmental factors may mediate the risk for ASD through immune activation and microglial activation. Individuals with ASD are reported to have elevated serum levels of major cytokines, including interleukins (IL-1, IL-6, IL-1ra), interferon-Δ (IFN-γ), tumor necrosis factor-α (TNF-α), and soluble TNF receptor (sTNFRII) [13, 14], which are associated with the severity of core ASD symptoms including social impairments and repetitive behaviors [15]. A postmortem report indicated microglial activation in 5 of 13 ASD cases in the region sampled, the dorsolateral prefrontal cortex [16]; and another postmortem study of 15 cases reported greater area of HLA-DR and GFAP immunostaining (of the former inclusive of reflecting microglial activation and the latter indicative of astroglial activation respectively) in the cerebellum (CER), anterior cingulate cortex (ACC), and middle frontal gyrus in ASD, along with selective proinflammatory cytokine upregulation [17].
Translocator protein (TSPO) PET imaging may be applied to measure gliosis in neuropsychiatric disease. TSPO expression is increased in microglia and, to a lesser extent astroglia, in neuropsychiatric diseases in humans [18, 19]. In the healthy brain, TSPO is largely found in endothelial cells [20] and the differential level of TSPO in neuropsychiatric disease is mainly attributed to gliosis [21]. To date, there has not been a TSPO imaging study in ASD sampling both males and females, nor has there been such a study applying a second-generation TSPO radioligand with full kinetic modeling. Presently, there are two studies that have investigated TSPO binding in ASD. The first study reported higher regional expression of TSPO in adults with ASD, using the first-generation radioligand [11C]PK11195 (ASD [n = 20], control [n = 20]) [22]. Although [11C]PK11195 was once the only radioligand available for PET, it has some disadvantages, mainly low specific binding relative to free and non-specific binding for TSPO [23]. The other PET study applied a second-generation radioligand ([11C]PBR28) and reported reduced TSPO expression in several brain regions in 15 ASD adults compared with 18 controls [24]; however, an arterial input function was not used to quantify TSPO VT in the brain. Both studies restricted their cohort to males with ASD. The present study addresses these gaps in the literature by sampling males and females, and applies full kinetic modeling to quantify TSPO VT with a second-generation radiotracer in the high resolution research tomograph (HRRT). On the basis of the postmortem reports, we hypothesized that TSPO VT would be elevated in ASD in the prefrontal cortex (PFC), ACC, Temporal Cortex, and CER compared to healthy, age-matched controls. The PFC, CER, and ACC were chosen because they showed elevated microglia activation in the described postmortem studies [16, 17] and higher TSPO as measured with [11C](R)-PK11195 BPnd [22]. The temporal cortex was also included as it showed a significant difference in the [11C](R)-PK11195 study [22].
Methods
Participants
Participants with ASD were recruited from the community and the Centre for Addiction and Mental Health (CAMH), Toronto, Ontario. Data from thirteen controls, approximately matching the mean and standard deviation of age and genotype (TSPO rs6971 polymorphism) of thirteen ASD participants, were selected from previously published works of our group [25,26,27]. As previous studies have reported sex-dependent differences in ASD [28] and TSPO [29], both male and female participants were included in the current work. This study was approved by the Research Ethics Board at CAMH. All participants provided written informed consent after all procedures were explained thoroughly.
To be eligible for the study, ASD participants had to have a diagnosis of ASD according to The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [1], confirmed using the Autism Diagnostic Observation Schedule-II (ADOS-II) [30]. The intelligent quotient (IQ) was assessed with either the Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV) [31] or the Wechsler Abbreviated Scale of Intelligence (WASI-II) [32]. The presence of psychiatric disorders in the control group was assessed using the Structured Clinical Interview for DSM-IV Axis I Disorders [33], since data from this group was collected from a previously acquired dataset [25,26,27]. Control volunteers were excluded if they had a first-degree family history of psychotic disorders (e.g., schizophrenia) due to significant overlap with ASD-genetic risk factors in these conditions [34]. All participants were excluded for any of the following reasons: being classified as a low-affinity binder for [18F]FEPPA based on the TSPO rs6971 polymorphism (see below), taking any anticoagulation or anti-inflammatory medications; history of seizures; pregnancy or currently breastfeeding; current or past substance use disorder of any recreational drugs (cannabis, cocaine, etc.); and the presence of metal implants precluding a Magnetic Resonance Imaging (MRI) scan.
In ASD participants, comorbidity was evaluated using MINI International Neuropsychiatric Interview [35]. Severity of ASD symptoms was assessed using the Adult Autism Spectrum Quotient (AQ, score range: 0–50, higher scores indicating more autistic traits) [36] the Adaptive Behavior Assessment System, Third Edition (ABAS-3, score range: 70–120, higher scores indicating better adaptive functioning) [37], the Repetitive Behavior Scale-Revised (RBS-R, score range: 1–129, higher scores indicating greater repetitive behaviors) [38], the Social Responsiveness Scale for adults (SRS-A, score range: 0–195, higher scores indicating greater social impairment) [39], the Behavior Rating Inventory for Executive Functions- Adult version (BRIEF-A, score range: 30–100, higher scores indicating greater executive functioning) [40] and the MATRICS Consensus Cognitive Battery (MCCB, score range: 10–100, higher scores reflecting better cognitive performance) [41]
DNA extraction and polymorphism genotyping
Each participant was genotyped for the TSPO rs6971 polymorphism, as previously described [42], and classified as high, mixed, or low-affinity binders (HAB, MAB, and LAB, respectively). Only HABs and MABs were included in the study, as LABs cannot be reliably quantified with [18F]FEPPA. While ASD participants were genotyped using saliva samples (Oragene DNA, DNA Genotek Inc., Ottawa, Canada) [43], the controls were genotyped using blood DNA [44].
PET and MRI acquisition
Details of PET and MRI data acquisition have been described thoroughly elsewhere [45]. Briefly, all [18F]FEPPA PET scans were performed using a high-resolution PET scanner (CPS HRRT; Siemens) for 120 min following an intravenous bolus injection of 180 ± 15 MBq of [18F]FEPPA. All participants underwent a structural (PD—proton density weighted) MRI scan using a 3 T MR-750 scanner (General Electric Medical Systems, Milwaukee, WI, USA) with the following parameters (2D/FSE-XL/ASSET, echo time ≈ 15 ms, repetition time ≈ 6000 ms, FOV = 22 cm, matrix = 256 × 256, Slices = 86, spacing interleave, slice thickness = 2 mm, number of excitations (NEX) = 1. These images were then co-registered with the averaged PET images for the delineation of individual regions of interest (ROI).
Arterial sampling
Arterial sampling was withdrawn continuously for the first 22 min from a radial artery cannula and counted using an automatic blood sampling system (ABSS, Model # PBS-101 from Veenstra Instruments, Joure, Netherlands). Additional manual samples were collected at specific time points from the same arterial cannula. Blood samples were centrifuged and the fraction of parent compound in the resulting plasma was determined using Oasis HLB cartridge (Waters, 6 cc) similarly as we described previously [46]. This method was validated using high-performance liquid chromatography analytical analysis. Radioactivity was counted with either a Packard Cobra II (Perkin-Elmer, Waltham, MA, USA), or a Wizard 2480 gamma counter cross-calibrated with the PET system. The delay and dispersion corrected input function was created as previously described [47].
Image analysis
Time-activity curves (TACs) were extracted for the bilateral PFC, temporal cortex, cerebellar cortex, ACC, and the gray matter as a whole using a validated in-house imaging pipeline (ROMI) [48]. All ROIs were delineated using individual PD-weighted MRI [48]. We restricted our initial analyses for this study to those four specific regions because they show strong evidence of pronounced neuropathology in ASD (including signs of inflammation) [16, 17, 22, 49]. Kinetic parameters of [18F]FEPPA were derived from the TACs using a two-tissue compartment model (2TCM) and plasma input function to obtain the total distribution volume (VT) for each ROI, which has been validated for [18F]FEPPA quantification and described elsewhere [45, 47]. The kinetic analysis of the radioligand was performed using in-house software (fMOD).
Statistical analysis
Statistical analyses were performed using SPSS Statistics (version 27.0, IBM, Armonk, NY, USA). Demographic and clinical characteristics were compared between ASD and control participants using independent sample t-tests for continuous variables, and chi-square tests for categorical variables. Group differences in [18F]FEPPA total distribution volume (VT) were analyzed using random effects mixed model analysis, with prioritized ROI, group and TSPO genotype as fixed factors, participant identification number as a random effect (including the intercept), and regional [18F]FEPPA VT as the dependent variable. In a mixed model analysis, all results were controlled for four brain regions: PFC, temporal cortex, cerebellar cortex, and ACC. Gray matter as a whole was analyzed separately using analysis of variance, controlling for TSPO genotype. Effect size (Cohen’s d) was calculated as the difference between the estimated marginal means from SPSS divided by the mean SD across all prioritized brain regions. As described by Cohen, effect sizes were interpreted as follows: Cohen’s d = 0.2 a small effect, Cohen’s d = 0.5 a medium effect, and Cohen’s d = 0.80 a large effect [50].
Results
Demographics and injection parameters
A total of 21 ASD participants were enrolled in the study. Of those, five did not meet the inclusion criteria or withdrew consent and 3 were not scanned with [18F]FEPPA because either radiochemistry, or arterial or venous catheterization was unsuccessful. The remaining 13 ASD participants were scanned with [18F]FEPPA and included in the study (\(\bar x \pm {{{{{\rm{sd}}}}}}\); 24.9 ± 5.2 years old, 5 females, 8 males, 8 HABS, 5 MABS). However, we could not find an identifiable solution for the 2TCM for the TAC of the ACC of one ASD subject, consequently, the associated VT value was unreliable and not used. A patient left the scanner earlier, at 90 min after injection. The inclusion or exclusion of this subject did not change the results following analyses to account for this methodological deficiency. The clinical measurement is presented in Table 1. While taking any anticoagulation or anti-inflammatory medications was part of the exclusion criteria, six participants from the ASD cohort were taking other medications: subject a: lorazepam (PET and MRI); subject b: Sertraline (PET) and citalopram (MRI), subject c: fluoxetine and methylphenidate (PET and MRI), subject d: lisdexamfetamine and vitamin D (PET and MRI), subject e: acetaminophen (PET) and pantoprazole (MRI), subject f: bupropion and methylphenidate (MRI). The MINI International Neuropsychiatric Interview revealed the presence of comorbidities which included concurrent Major Depressive Episode (n = 2), Dysthymia (1), Manic Episode (1), Agoraphobia, current w/o history of panic disorder (n = 3), Generalized Anxiety Disorder (4). Thirteen typically developing controls approximately matching age and genotype of the ASD participants (25.0 ± 5.2 years old, 9 females, 8 HABS, 5 MABS) were selected from previously published works of our group [25,26,27]. While there were no significant group differences in [18F]FEPPA activity injected, there was a significant group difference in the mass injected (1.6 ± 0.7 vs 0.9 ± 0.6 μg) due to a difference in specific activity (Table 1).
Differences in [18F]FEPPA V T between ASD participants and controls
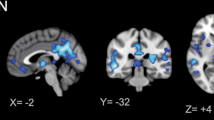
There was no effect of group (ASD participants vs controls) on [18F]FEPPA VT (main group effect: F(1,26)= 1.74, p = 0.20; ROI effect: F(3,77) = 9.94, p < 0.001) (Fig. 1). However, two ASD participants who had the highest [18F]FEPPA VT values (Fig. 1) were also diagnosed with major depressive episode, based on the MINI international Neuropsychiatric interview. Re-analysis of the data excluding those participants revealed a significant effect of group, such that ASD participants had lower [18F]FEPPA VT compared to controls (main group effect: F(1,24)= 6.62, p = 0.02; ROI effect: F(3,71) = 8.57, p < 0.001; Cohen’s d = 0.85, large effect size; 27% lower in the temporal cortex and cerebellar cortex, 28% lower in the PFC, 29% lower in the ACC). Similar results were observed using the whole gray matter region: main group effect F(1,23) = 1.46, p = 0.24 and in the post-hoc analysis excluding the ASD participants with MDE F(1,21) = 6.66, p = 0.017 with [18F]FEPPA VT 28% lower in ASD.
Groups were classified according to their TSPO rs6971 genotype as high-affinity binders (HABs) or mixed affinity binders (MABs). ASD participants with a concurrent major depressive episode (MDE) were both HABs, and are highlighted with a square symbol (n = 2). The individual data points show the original [18F]FEPPA VT values and the horizontal bars indicate group means adjusted for TSPO rs6971 genotype using the estimated marginal means of each region (including ASD participants with a concurrent MDE).
Discussion
To our knowledge, this is the first in vivo quantification of brain TSPO in ASD participants with a second-generation radiotracer and full kinetic modeling using state-of-the-art methodology (arterial input function in HRRT) that includes both female and male participants. Contrary to our hypothesis, participants with ASD either had no significant differences when compared to typically developing controls, or significantly lower levels of TSPO in the brain (when excluding participants with MDE). To a greater extent this contrasts postmortem studies, and to a lesser extent previous neuroimaging findings.
Many studies have suggested that neuroinflammation plays a role in the pathogenesis of ASD. For example, postmortem studies [16, 17, 51,52,53,54] have shown a significant higher microglial activation in patients with ASD. Additionally, other studies have reported a higher expression of microglial marker genes in post-mortem brains of ASD subjects relative to controls [55, 56]. Cerebrospinal fluid [17] also revealed higher concentrations of the proinflammatory marker MCP-1. Peripheral blood studies have also shown higher activation of microglia cells in ASD subjects [57, 58]. However, there are also post-mortem studies that showed no difference in microglial activation between ASD subjects and controls [59, 60]. At the cellular level the present study argues against a gliosis labeled with TSPO in high-functioning ASD, but would not rule out a gliosis with different characteristics that does not overexpress TSPO. For example gliosis with overexpression of GFAP, which is often reported in ASD, is largely reflective of astroglial activation, not microglial activation and does not typically correlate with TSPO binding [61].
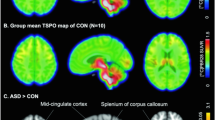
While imaging methods differ because the present study applied full kinetic modeling, the conclusions of the present study are more in line with Zurcher et al. [24], who applied a second-generation TSPO PET radiotracer in autism. Using [11C]PBR28, Zurcher et al. found an undisclosed, but significant, lower SUVR60–90 min (whole brain normalization) in a voxelwise analysis in the insular cortex, precuneus/posterior cingulate cortex, and the temporal, angular, and supramarginal gyri in adult males with high and low functional ASD compared to controls [24]. While lower SUVR may represent a decrease in TSPO levels, this quantification approach is problematic. Using the whole brain as a reference region includes the uptake of the region of interest in both the numerator and denominator, and other factors can confound changes in SUVR (e.g., the clearance of radioligand from plasma [62]). It should be mentioned that analyzing the regional TACs of the present work (prefrontal, temporal, cerebellar and anterior cingulate cortices) with SUVR (100–120 min) using the gray and white matter as reference region, we did not observe any significant group difference, either including or not the subjects with MDE. The SUVR of the ASD participants with concurrent MDE were not higher than the SUVR of the rest of the HAB ASD participants. Our current study addresses previous methodological issues and in a post-hoc analysis, when excluding subjects with MDE (n = 2), showed lower TSPO binding in ASD relative to controls. The two participants with MDE were HABs and showed higher VT than the rest of the subjects. A previous study from our group showed that individuals with MDE have a higher [18F]FEPPA VT (about 30%) compared to controls [44, 54], and six studies across four different sites report higher TSPO binding in the gray matter regions sampled during MDE [21, 63,64,65,66,67,68]. We focused on MDE based on our previous works, however, there were other comorbidities present in this population and the same 2 participants presented generalized anxiety disorder.
The reasons for a lower [18F]FEPPA VT in ASD (after excluding ASD participants with MDE) are unknown but could be related to the time in the stage of illness in which the sampling was done. A similar issue has been raised in previous studies in TSPO in patients with psychosis [69] and a first episode psychosis [70] also have shown lower in TSPO binding contrary to the prevalent hypothesis of increased neuroinflammation. Newer results from animal models of schizophrenia showed that while TSPO is upregulated after a severe neuroinflammatory insult, TSPO is downregulated in adult animals with a prenatal induced infection in a neurodevelopmental mouse model of schizophrenia which presented increased inflammatory cytokine expression [71]. Our study focuses on ASD participants older than 18 years of age, however, it is well-known that this neurodevelopmental disorder begins very early in development [72]. Environment and genetic factors are involved in the etiology of ASD [73]. One of the best examples of known environmental risk factors for ASD is prenatal exposure to the antiepileptic and mood stabilizer drug valproic acid (VPA). When this drug is taken during pregnancy, it can result in children displaying autistic-like features, such as impaired communication, reduced sociability, and stereotyped behaviors [74, 75]. Thus, when considering the participants without MDE, our study could be an analog situation to the Notter et al. study [71]: we could have observed a lower TSPO levels in adult ASD participants as a consequence of the exposure to a neuroimmune alteration earlier in life. On the contrary, the ASD participants with MDE, who present a current neuroinflammatory process, consequently presented higher TSPO levels. This hypothesis needs to be addressed in future studies. A study comparing ASD participants with and without depression could shed light on this suggestion as well.
When interpreting the results, the limitations of this study should be considered. First, although [18F]FEPPA VT is mostly attributed to microglial function, studies show that TSPO is also expressed by astrocytes and vascular endothelial cells. However, both astrocytes and endothelial cells are known to be key factors in brain immunity, and our conclusion is not undermined by the potential role these cells play in the [18F]FEPPA VT signal. Second, the sample size is admittedly small, and it included both male and female participants. The number of females with ASD in this cohort was an over-representation of its actual proportion in the general population, where ASD is more prevalent in males than in females. A significant association between sex and TSPO has been previously reported [76]; although, this was not found in all previous studies. In our cohort, sex had no significant effect on [18F]FEPPA VT (with MDE: main sex effect: F (1,26) = 1.23, p = 0.28; without MDE: main sex effect: F (1,24) = 0.01, p = 0.92). This may be related to small sample sizes of each group by sex. Third, the control group (n = 13, age 25 ± 5.2, M = 4, 8 HABs) is a subset of a greater sample (n = 27, age 23.6 ± 4.2, 9 males, 19 HABs) published previously [25]. The 13 subjects were selected based on the demographic variables (age 24.8 ± 5.2), and genotype (8 HABs) following the order in which they appeared in our database. It should be noted that, the means and variability of the 13 control subjects selected match very well the mean and variability of [18F]FEPPA VT of the larger population (For example, for the whole gray matter for HABs [18F]FEPPA VT = 10.8 ± 3.7 (n = 19 [25]) vs. [18F]FEPPA VT = 11.6 ± 3.5 (n = 8, here) and for MABs [18F]FEPPA VT = 8.6 ± 2.9 (n = 8 [25]) vs [18F]FEPPA VT = 8.4 ± 2.9 (n = 5, here)). Thus, the 13 selected control cases very well match the ASD cases and do not differ from the larger sample. For consistency, the matched cases (n = 13) were kept for statistical testing. Fourth, some of the ASD participants were not drug-free: while participants were excluded for anti-inflammatory medications, some of them were prescribed antidepressants, anxiolytics, or stimulants as part of their clinical care that could potentially affect the uptake of [18F]FEPPA [65, 77]. One of the participants with MDE was taking Zoloft (50 mg) when the PET scan was acquired, and greater TSPO VT has also been reported in MDE treated with serotonin reuptake inhibitor antidepressants [68]. In order to investigate the effect of specific drugs on [18F]FEPPA uptake in ASD, further within participant studies are required. Fifth, most ASD participants in this study are high-functioning and it is unknown whether these preliminary findings apply to low functioning ASD individuals. Sixth, the mass of radioligand injected in the ASD group was greater than in the control groups. While a non-tracer dose effect is unlikely (see calculation below) and there has never been an apparent mass effect on [18F]FEPPA VT, it cannot be completely ruled out. Using the maximum mass injected (2.9 μg), a typical subject weight of 70 kg, a mean [18F]FEPPA plasma free fraction fp = 5% (unpublished) and the in-vitro Ki affinity for HABs = 0.5 nM [78], a maximum of 1% of TSPO would be bound to [18F]FEPPA [79]. A mass effect would reduce the VT, however the subject with the maximum mass injected, is the ASD subject with concurrent MDE and highest VT of the study (Fig. 1). Seventh, in this study we did not measure [18F]FEPPA fp. It has been difficult to obtain reliable fp measurements [80] and it is known that VT/fp for [11C]PBR28 increase its variability (e.g., [81]); thus, consistent with previous studies with [18F]FEPPA, VT/fp was not used as outcome measure in this study
Contrary to the hypothesis of elevated levels of TSPO in ASD, we conclude that participants with ASD present either no significant difference in TSPO concentration when compared to matched controls, or significantly lower levels of TSPO when excluding concurrent MDE.
References
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Arlington, VA. American Psychiatric Association Publishing; 2013.
Park HR, Lee JM, Moon HE, Lee DS, Kim BN, Kim J, et al. A short review on the current understanding of autism spectrum disorders. Exp Neurobiol. 2016;25:1–13.
Ofner MCA, Decou ML, Do MT, Bienek A, Snider J, Ugnat AM. The prevalence of autism spectrum disorder (ASD) among 5-17 year olds in seven provinces and territories in Canada in 2015 A national ASD surveillance system (NASS) report. Ottawa, ON: Public Health Agency of Canada; 2018.
Ronald A, Hoekstra RA. Autism spectrum disorders and autistic traits: a decade of new twin studies. American journal of medical genetics Part B, Neuropsychiatric genetics: the official publication of the International Society of Psychiatric Genetics. Am J Med Genet Part B, Neuropsychiatr Genet. 2011;156B:255–74.
Lord CEM, Baird G, Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. 2018;392:508–20.
Xu G, Strathearn L, Liu B, O'brien M, Kopelman TG, Zhu J, et al. Prevalence and treatment patterns of autism spectrum disorder in the United States, 2016. JAMA Pediatr. 2019;173:153–59.
Kogan MD, Vladutiu CJ, Schieve LA, Ghandour RM, Blumberg SJ, Zablotsky B, et al. The prevalence of parent-reported autism spectrum disorder among US children. Pediatrics. 2018;142:e20174161
De Rubeis S, He X, Goldberg AP, Poultney CS, Samocha K, Cicek AE, et al. Synaptic, transcriptional and chromatin genes disrupted in autism. Nature. 2014;515:209–15.
Rudie JD, Brown JA, Beck-Pancer D, Hernandez LM, Dennis EL, Thompson PM, et al. Altered functional and structural brain network organization in autism. NeuroImage Clin. 2013;2:79–94.
McDougle CJ, Landino SM, Vahabzadeh A, O’Rourke J, Zurcher NR, Finger BC, et al. Toward an immune-mediated subtype of autism spectrum disorder. Brain Res. 2015;1617:72–92.
Asadabadi M, Mohammadi MR, Ghanizadeh A, Modabbernia A, Ashrafi M, Hassanzadeh E, et al. Celecoxib as adjunctive treatment to risperidone in children with autistic disorder: a randomized, double-blind, placebo-controlled trial. Psychopharmacology. 2013;225:51–59.
McAllister AK, Patterson PH. Introduction to special issue on neuroimmunology in brain development and disease. Dev Neurobiol. 2012;72:1269–71.
Croonenberghs J, Wauters A, Devreese K, Verkerk R, Scharpe S, Bosmans E, et al. Increased serum albumin, gamma globulin, immunoglobulin IgG, and IgG2 and IgG4 in autism. Psychol Med. 2002;32:1457–63.
Rossignol DA, Frye RE. A review of research trends in physiological abnormalities in autism spectrum disorders: immune dysregulation, inflammation, oxidative stress, mitochondrial dysfunction and environmental toxicant exposures. Mol Psychiatry. 2012;17:389–401.
Ashwood P, Enstrom A, Krakowiak P, Hertz-Picciotto I, Hansen RL, Croen LA, et al. Decreased transforming growth factor beta1 in autism: a potential link between immune dysregulation and impairment in clinical behavioral outcomes. J Neuroimmunol. 2008;204:149–53.
Morgan JT, Chana G, Pardo CA, Achim C, Semendeferi K, Buckwalter J, et al. Microglial activation and increased microglial density observed in the dorsolateral prefrontal cortex in autism. Biol Psychiatry. 2010;68:368–76.
Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann Neurol. 2005;57:67–81.
Venneti S, Wang G, Nguyen J, Wiley CA. The positron emission tomography ligand DAA1106 binds with high affinity to activated microglia in human neurological disorders. J Neuropathol Exp Neurol. 2008;67:1001–10.
Cosenza-Nashat M, Zhao ML, Suh HS, Morgan J, Natividad R, Morgello S, et al. Expression of the translocator protein of 18 kDa by microglia, macrophages and astrocytes based on immunohistochemical localization in abnormal human brain. Neuropathol Appl Neurobiol. 2009;35:306–28.
Betlazar C, Harrison-Brown M, Middleton RJ, Banati R, Liu GJ. Cellular sources and regional variations in the expression of the neuroinflammatory marker translocator protein (TSPO) in the normal brain. Int J Mol Sci. 2018;19:2707.
Meyer JH, Cervenka S, Kim MJ, Kreisl WC, Henter ID, Innis RB. Neuroinflammation in psychiatric disorders: PET imaging and promising new targets. Lancet Psychiatry. 2020;7:1064–74.
Suzuki K, Sugihara G, Ouchi Y, Nakamura K, Futatsubashi M, Takebayashi K, et al. Microglial activation in young adults with autism spectrum disorder. JAMA Psychiatry. 2013;70:49–58.
Chauveau F, Boutin H, Van Camp N, Dolle F, Tavitian B. Nuclear imaging of neuroinflammation: a comprehensive review of [11C]PK11195 challengers. Eur J Nucl Med Mol Imaging. 2008;35:2304–19.
Zurcher NR, Loggia ML, Mullett JE, Tseng C, Bhanot A, Richey L, et al. [(11)C]PBR28 MR-PET imaging reveals lower regional brain expression of translocator protein (TSPO) in young adult males with autism spectrum disorder. Mol Psychiatry. 2021; 26:1659–69.
Da Silva T, Hafizi S, Watts JJ, Weickert CS, Meyer JH, Houle S, et al. In vivo imaging of translocator protein in long-term cannabis users. JAMA Psychiatry. 2019;76:1305–13.
Hafizi S, Silva TDA, Gerritsen C, Kiang M, Bagby RM, Prce I, et al. Imaging microglial activation in individuals at clinical high risk for psychosis: an in vivo PET study with [(18)F]FEPPA. Neuropsychopharmacology. 2017;42:2474–81.
Hafizi S, Tseng HH, Rao N, Selvanathan T, Kenk M, Bazinet RP, et al. Imaging microglial activation in untreated first-episode psychosis: a PET study with [(18)F]FEPPA. Am J Psychiatry. 2017;174:118–24.
Lai MC, Lombardo MV, Auyeung B, Chakrabarti B, Baron-Cohen S. Sex/gender differences and autism: setting the scene for future research. J Am Acad Child Adolesc Psychiatry. 2015;54:11–24.
Tuisku JP, Sigray P, Gaiser EC, Airas L, Al-Abdulrasul H, Brück A, et al. Effects of age, BMI and sex on the glial cell marker TSPO — a multicentre [11C]PBR28 HRRT PET study. Eur J Nucl Med Mol Imaging. 2019;46:2329–38.
Lord C, Risi S, Lambrecht L Jr, Cook EH Jr, Leventhal BL, DiLavore PC, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30:205–23.
Wechsler, D. Wechsler Adult Intelligence Scale—Fourth Edition. San Antonio, TX: Pearson. 2008.
Wechsler D. Wechsler Abbreviated Scale of Intelligence–Second Edition (WASI-II). San Antonio, TX. Pearson. 2011.
First MSR, Gibbon M, Williams J. Structured clinical interview for DSM-IV axis I disorders: patient edition (SCIDI/P), Version 2.0. Biometric Research. New York: New York State Psychiatric Institute; 1995.
Hormozdiari FPO, Borenstein E, Eichler EE. The discovery of integrated gene networks for autism and related disorders. Genome Res. 2015;25:142–54.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59:22–33.
Woodbury-Smith MR, Robinson J, Wheelwright S, Baron-Cohen S. Screening adults for Asperger syndrome using the AQ: a preliminary study of its diagnostic validity in clinical practice. J Autism Dev Disord. 2005;35:331–35.
Harrison P, Oakland T. Adaptive Behavior Assessment System, Third edition (ABAS-3). San Antonio, TX: Pearson. 2015.
Lam KSL, Aman MG. The repetitive behavior scale-revised: independent validation in individuals with autism spectrum disorders. J Autism Dev Disord. 2007;37:855–66.
S. B. Brief Report: the Social Responsiveness Scale for Adults (SRS-A): initial results in a German cohort. J Autism Dev Disord. 2012;42:1998–9.
Roth RM, Isquith PK, Gioia GA. BRIEF—A: Behavior Rating Inventory of Executive Function— Adult Version. Psychological Assessment Resources, Lutz, FL. 2005.
August SM, Kiwanuka J, McMahon RP, Gold JM. The MATRICS Consensus Cognitive Battery (MCCB): clinical and cognitive correlates. Schizophr Res. 2012;134:76–82.
Lahiri DK, Nurnberger JI Jr. A rapid non-enzymatic method for the preparation of HMW DNA from blood for RFLP studies. Nucleic Acids Res. 1991;19:5444.
Rathitharan G, Truong J, Tong J, Mccluskey T, Meyer JH, Mizrahi R. et al. Microglia imaging in methamphetamine use disorder: a positron emission tomography study with the 18 kDa translocator protein radioligand [F-18]FEPPA. Addict Biol.2020;26:e12876
Mizrahi R, Rusjan PM, Kennedy J, Pollock B, Mulsant B, Suridjan I, et al. Translocator protein (18 kDa) polymorphism (rs6971) explains in-vivo brain binding affinity of the PET radioligand [18F]-FEPPA. J Cereb Blood F Met. 2012;32:968–72.
Kenk M, Selvanathan T, Rao N, Suridjan I, Rusjan P, Remington G, et al. Imaging neuroinflammation in gray and white matter in schizophrenia: an in-vivo PET study with [18F]-FEPPA. Schizophr Bull. 2015;41:85–93.
Rusjan PM, Wilson AA, Mizrahi R, Boileau I, Chavez SE, Lobaugh NJ, et al. Mapping human brain fatty acid amide hydrolase activity with PET. J Cereb Blood Flow Metab. 2013;33:407–14.
Rusjan PM, Wilson A, Bloomfield PM, Vitcu I, Meyer JH, Houle S, et al. Quantitation of translocator protein binding in human brain with the novel radioligand [18F]-FEPPA and positron emission tomography. J Cereb Blood Flow Metab. 2011;31:1807–16.
Rusjan P, Mamo D, Ginovart N, Hussey D, Vitcu I, Yasuno F, et al. An automated method for the extraction of regional data from PET images. Psychiatry Res. 2006;147:79–89.
Becker EB, Stoodley CJ. Autism spectrum disorder and the cerebellum. Int Rev Neurobiol. 2013;113:1–34.
Cohen J. Statistical power analysis for the behavioral sciences. L. Hillsdale, NJ: Erlbaum Associates; 1988.
Morgan JT, Chana G, Abramson I, Semendeferi S, Courchesne E, Everall IP. Abnormal microglial-neuronal spatial organization in the dorsolateral prefrontal cortex in autism. Brain Res. 2012;1456:72–81.
Tetreault NA, Hakeem A, Jiang S, Williams BA, Allman E, Wold BJ, et al. Microglial in the cerebral cortex in autism. J Autism Dev Disord. 2012;42:2569–84.
Lee AS, Azmitia E, Whitaker-Azmitia PM. Developmental microglial priming in postmortem autism spectrum disorder temporal cortex. Brain Behav Immun. 2017;62:193–202.
Menassa DA, Sloan C, Chance SA. Primary olfactory cortex in autism and epilepsy: increased glial cells in autism. Brain Pathol. 2017;27:437–48.
Edmonson CZM, Rennert OM. Altered glial marker expression in autistic post-mortem prefrontal cortex and cerebellum. Mol Autism. 2014;5:3.
Fiorentino M, Sapone A, Senger S, Camhi SS, Kadzielski SM, Buie TM, et al. Blood-brain barrier and intestinal epithelial barrier alterations in autism spectrum disorders. Mol Autism. 2016;7:49.
Ishizuka K, Fujita Y, Kawabata T, Kimura H, Iwayama Y, Inada T, et al. Rare genetic variants in CX3CR1 and their contribution to the increased risk of schizophrenia and autism spectrum disorders. Transl Psychiatry. 2017;7:e1184.
Patel AB, Tsilioni I, Leeman SE, Theoharides TC. Neurotensin stimulates sortilin and mTOR in human microglia inhibitable by methoxyluteolin, a potential therapeutic target for autism. Proc Natl Acad Sci USA. 2016;113:E7049–E58.
Morgan JT, Barger N, Amaral DG, Schumann CM. Stereological study of amygdala glial populations in adolescents and adults with autism spectrum disorder. PLoS ONE. 2014;9:e110356.
Adorjan I, Ahmed B, Feher V, Torso M, Krug K, Esiri M, et al. Calretinin interneuron density in the caudate nucleus is lower in autism spectrum disorder. Brain. 2017;140:2028–40.
Martin A, Boisgard R, Theze B, Van Camp N, Kuhnast B, Damont A, et al. Evaluation of the PBR/TSPO radioligand [(18)F]DPA-714 in a rat model of focal cerebral ischemia. J Cereb Blood Flow Metab. 2010;30:230–41.
Carson RE, Channing MA, Blasberg RG, Dunn BB, Cohen RM, Rice KC, et al. Comparison of bolus and infusion methods for receptor quantitation: application to [18F]cyclofoxy and positron emission tomography. J Cereb Blood Flow Metab. 1993;13:24–42.
Setiawan E, Wilson AA, Mizrahi R, Rusjan PM, Miler L, Rajkowska G, et al. Role of translocator protein density, a marker of neuroinflammation, in the brain during major depressive episodes. JAMA Psychiatry. 2015;72:268–75.
Li L, Wang W, Zhang LM, Jiang XY, Sun SZ, Sun LJ, et al. Overexpression of the 18 kDa translocator protein (TSPO) in the hippocampal dentate gyrus produced anxiolytic and antidepressant-like behavioural effects. Neuropharmacology. 2017;125:117–28.
Richards EM, Zanotti-Fregonara P, Fujita M, Newman L, Farmer C, Ballard ED, et al. PET radioligand binding to translocator protein (TSPO) is increased in unmedicated depressed subjects. EJNMMI Res. 2018;8:57.
Wohleb ES, Hanke M, Corona AW, Powell ND, Stiner LM, Bailey MT, et al. beta-Adrenergic receptor antagonism prevents anxiety-like behavior and microglial reactivity induced by repeated social defeat. J Neurosci. 2011;31:6277–88.
Sawada A, Niiyama Y, Ataka K, Nagaishi K, Yamakage M, Fujimiya M. Suppression of bone marrow-derived microglia in the amygdala improves anxiety-like behavior induced by chronic partial sciatic nerve ligation in mice. Pain. 2014;155:1762–72.
Setiawan E, Attwells S, Wilson AA, Mizrahi R, Rusjan PM, Miler L, et al. Association of translocator protein total distribution volume with duration of untreated major depressive disorder: a cross-sectional study. Lancet Psychiatry. 2018;5:339–47.
Plavén-Sigray P, Matheson GJ, Collste K, Ashok AH, Coughlin JM, Howes OD, et al. Positron emission tomography studies of the glial cell marker translocator protein in patients with psychosis: a meta-analysis using individual participant data. Biol Psychiatry. 2018;84:433–42.
Collste K, Plavén-Sigray P, Fatouros-Bergman H, Victorsson P, Schain M, Forsberg A, et al. Lower levels of the glial cell marker TSPO in drug-naive first-episode psychosis patients as measured using PET and [(11)C]PBR28. Mol Psychiatry. 2017;22:850–56.
Notter T, Coughlin JM, Gschwind T, Weber-Stadlbauer U, Wang Y, Kassiou M, et al. Translational evaluation of translocator protein as a marker of neuroinflammation in schizophrenia. Mol Psychiatry. 2018;23:323–34.
Daniels AM, Mandell DS. Explaining differences in age at autism spectrum disorder diagnosis: a critical review. Autism: Int J Res Pract. 2014;18:583–97.
Hallmayer J, Cleveland S, Torres A, Phillips J, Cohen B, Torigoe T, et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch Gen Psychiatry. 2011;68:1095–102.
Williams PG, Hersh JH. A male with fetal valproate syndrome and autism. Developmental Med Child Neurol. 1997;39:632–4.
Williams G, King J, Cunningham M, Stephan M, Kerr B, Hersh JH. Fetal valproate syndrome and autism: additional evidence of an association. Dev Med Child Neurol. 2001;43:202–6.
Tuisku J, Plavén-Sigray P, Gaiser EC, Airas L, Al-Abdulrasul H, Brück A, et al. Effects of age, BMI and sex on the glial cell marker TSPO - a multicentre [(11)C]PBR28 HRRT PET study. Eur J Nucl Med Mol Imaging. 2019;46:2329–38.
Danovich L, Veenman L, Leschiner S, Lahav M, Shuster V, Weizman A, et al. The influence of clozapine treatment and other antipsychotics on the 18 kDa translocator protein, formerly named the peripheral-type benzodiazepine receptor, and steroid production. Eur Neuropsychopharmacol. 2008;18:24–33.
Berroterán-Infante N, Balber T, Fürlinger P, Bergmann M, Lanzenberger R, Hacker M, et al. [(18)F]FEPPA: improved automated radiosynthesis, binding affinity, and preliminary in vitro evaluation in colorectal cancer. ACS Med Chem Lett. 2018;9:177–81.
Cumming P. Absolute abundances and affinity states of dopamine receptors in mammalian brain: a review. Synapse. 2011;65:892–909.
Rusjan P, Sabioni P, Di Ciano P, Mansouri E, Boileau I, Laveillé A, et al. Exploring occupancy of the histamine H3 receptor by pitolisant in humans using PET. Br J Pharmacol. 2020;177:3464–72.
Hines CS, Fujita M, Zoghbi SS, Kim JS, Quezado Z, Herscovitch P, et al. Propofol decreases in vivo binding of 11C-PBR28 to translocator protein (18 kDa) in the human brain. J Nucl Med. 2013;54:64–9.
Acknowledgements
The authors would like to thank Dr. Sylvain Houle for leadership and general administrative support; Dr. Stephanie H. Ameis for recruitment of participants with ASD, determination of eligibility criteria, partial contributions to the design of the work; and medical coverage; June Parkes, Irina Vitcu, Laura Miler, Ivana Prce, Dr. Sina Hafizi, Dr. Jeremy Watts, Dr. Nancy Lobaugh NJ, Tina McCluskey, Armando Garcia, and Alvina Ng from the CAMH PET Centre for technical support and advice, Caroline Kassee for uploading the CRFs to the REDCap, Marcos Sanchez for biostatistical support, Dr. Pushpal Desarkar, Dr. Meng-Chuan Lai and Dr. Nathan Kolla for medical support.
Author contributions
All the authors revised critically for important intellectual content and approved the final version of this manuscript. RM, PR and AW conceived and designed the study. PR contributed to the acquisition, analysis, and interpretation of data. AG and TDS contributed to the acquisition and analysis of the data. CLC contributed to the analysis of the data. DS wrote the initial version of the manuscript and contributed in the statistical analysis of the data. JM contributed to the interpretation of data.
Funding
This work was supported by the Operating Grant from the Canadian Institutes of Health Research (CIHR MOP-142376).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
RM has given talks with travel support from Janssen. JHM has been a consultant to Lundbeck and Takeda, in the past 5 years. JHM has applied for a patent for blood markers as indicators of brain inflammation, has patented blood markers as biomarkers of depression, and has patented/developing a dietary supplement to prevent postpartum depression. JHM is received operating grant funding from Sanofi for a neuroinflammation PET imaging study in multiple sclerosis. JHM is arranging collaborations with nutraceutical companies for dietary supplement to prevent postpartum depression. All other authors declare no conflicts of interest
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Simpson, D., Gharehgazlou, A., Da Silva, T. et al. In vivo imaging translocator protein (TSPO) in autism spectrum disorder. Neuropsychopharmacol. 47, 1421–1427 (2022). https://doi.org/10.1038/s41386-022-01306-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-022-01306-4
This article is cited by
-
In vivo translocator protein in females with autism spectrum disorder: a pilot study
Neuropsychopharmacology (2024)
-
Microglial contribution to the pathology of neurodevelopmental disorders in humans
Acta Neuropathologica (2023)
-
Neuroinflammation in autism spectrum disorders: potential target for mesenchymal stem cell-based therapy
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2022)