Abstract
Objective
This study aims to estimate the prevalence of early-onset sarcopenia and sarcopenic obesity in the United States and its relative risk due to obstructive sleep apnea (OSA).
Methods
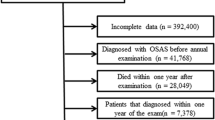
Data in this cross-sectional study were extracted from the National Health and Nutritional Examination Survey (NHANES) 2015-2018. Weighted multistage stratified probability sampling design was considered to estimate the prevalence of early-onset sarcopenia and sarcopenic obesity. Weighted multivariable logistic regression analyses and weighted multivariable mediation models were performed to evaluate the association between OSA and early-onset sarcopenia.
Results
The prevalence of early-onset sarcopenia and early-onset sarcopenic obesity was estimated to be 5.5% and 4.6%, respectively. A higher prevalence of sarcopenia (12% V.S. 5.5%, P < 0.01) and sarcopenic obesity (10.3% V.S. 4.0%, P < 0.01) was observed among participants with OSA than those without OSA. Multivariable logistic regression models suggested that participants with OSA had higher odds ratios of suffering from early-onset sarcopenia [Odds Ratio (OR): 1.5, 95% confidence interval (CI):1.1-2.7] and early-onset sarcopenic obesity [OR: 1.8, 95% CI: 1.1-3.1] after adjusting for potential confounding variables. Mediation analyses suggested serum chronic reaction protein (CRP) mediated 23.7% (P < 0.01) & 26.2% (P < 0.01), homeostasis model assessment insulin resistance index (HOMA-IR) mediated 24.8% (P < 0.01) & 20.7% (P < 0.05), body mass index (BMI) mediated 46.4% (P < 0.05) & 49.9% (P < 0.01), HEI-2015 mediated 23.3% (P < 0.01) & 25.6% (P < 0.01), and Vitamin D mediated 7.5% (P < 0.01) & 8.5% (P < 0.01) of the potential effects of OSA on early-onset sarcopenia and sarcopenic obesity, respectively.
Conclusion
Early-onset sarcopenia and sarcopenic obesity were prevalent among young adults in the US. OSA is a significant independent risk factor and may induce muscle loss by unhealthy diet habits, higher BMI, chronic inflammation, insulin resistance, and Vitamin D. It was essential for clinicians to arrange appropriate screening and interventions for patients with OSA to prevent muscle loss as early as possible.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data generated during and/or analyzed during the current study will be available from the corresponding author on reasonable request.
References
Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393:2636–46.
Jung HN, Jung CH, Hwang YC. Sarcopenia in youth. Metabolism. 2023;144:155557.
Echouffo-Tcheugui JB, Niiranen TJ, McCabe EL, Henglin M, Jain M, Vasan RS, et al. An early-onset subgroup of Type 2 Diabetes: A multigenerational, prospective analysis in the Framingham Heart Study. Diabetes Care. 2020;43:3086–93.
Choi KM. Sarcopenia and sarcopenic obesity. Korean J Intern Med. 2016;31:1054–60.
Barazzoni R, Bischoff S, Boirie Y, Busetto L, Cederholm T, Dicker D, et al. Sarcopenic obesity: time to meet the challenge. Obes Facts. 2018;11:294–305.
Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc. 2004;52:80–5.
Goates S, Du K, Arensberg MB, Gaillard T, Guralnik J, Pereira SL. Economic Impact of Hospitalizations in US Adults with Sarcopenia. J Frailty Aging. 2019;8:93–99.
De Spiegeleer A, Beckwee D, Bautmans I, Petrovic M. Pharmacological interventions to improve muscle mass, muscle strength and physical performance in older people: an umbrella review of systematic reviews and meta-analyses. Drugs Aging. 2018;35:719–34.
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3:310–8.
Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84.
Gottlieb DJ, Yenokyan G, Newman AB, O’Connor GT, Punjabi NM, Quan SF, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–60.
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:203–41.
Kendzerska T, Gershon AS, Hawker G, Tomlinson G, Leung RS. Obstructive sleep apnea and incident diabetes: a historical cohort study. Am J Respir Crit Care Med. 2014;190:218–25.
Bekfani T, Schöbel C, Pietrock C, Valentova M, Ebner N, Döhner W, et al. Heart failure and sleep-disordered breathing: susceptibility to reduced muscle strength and preclinical congestion (SICA-HF cohort). ESC Heart Fail. 2020;7:2063–70.
Fernandes JFR, Barreto Silva MI, Loivos CP, Menna Barreto APM, Meira VDS, Kaiser SE, et al. Obstructive sleep apnea in non-dialyzed chronic kidney disease patients: Association with body adiposity and sarcopenia. Nutrition. 2019;57:282–9.
Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES Dietary Data: Focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr. 2016;7:121–34.
Tahapary DL, Pratisthita LB, Fitri NA, Marcella C, Wafa S, Kurniawan F, et al. Challenges in the diagnosis of insulin resistance: Focusing on the role of HOMA-IR and Tryglyceride/glucose index. Diabetes Metab Syndr. 2022;16:102581.
Krebs-Smith SM, Pannucci TE, Subar AF, Kirkpatrick SI, Lerman JL, Tooze JA, et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118:1591–602.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–23.
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69:547–58.
Bianchi L, Maietti E, Abete P, Bellelli G, Bo M, Cherubini A, et al. Comparing EWGSOP2 and FNIH Sarcopenia definitions: agreement and 3-year survival prognostic value in older hospitalized adults: The GLISTEN Study. J Gerontol A Biol Sci Med Sci. 2020;75:1331–7.
Donini LM, Busetto L, Bischoff SC, Cederholm T, Ballesteros-Pomar MD, Batsis JA, et al. Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO consensus statement. Clin Nutr. 2022;41:990–1000.
Arslanian S, Bacha F, Grey M, Marcus MD, White NH, Zeitler P. Evaluation and management of youth-onset type 2 diabetes: a position statement by the American Diabetes Association. Diabetes Care. 2018;41:2648–68.
Scinicariello F, Buser MC, Feroe AG, Attanasio R. Antimony and sleep-related disorders: NHANES 2005-2008. Environ Res. 2017;156:247–52.
Palmer MK, Toth PP. Trends in lipids, obesity, metabolic syndrome, and diabetes mellitus in the United States: An NHANES Analysis (2003-2004 to 2013-2014). Obesity. 2019;27:309–14.
Petermann-Rocha F, Ferguson LD, Gray SR, Rodríguez-Gómez I, Sattar N, Siebert S, et al. Association of sarcopenia with incident osteoporosis: a prospective study of 168,682 UK biobank participants. J Cachexia Sarcopenia Muscle. 2021;12:1179–88.
Cleasby ME, Jamieson PM, Atherton PJ. Insulin resistance and sarcopenia: mechanistic links between common co-morbidities. J Endocrinol. 2016;229:R67–81.
Han E, Lee YH, Kim YD, Kim BK, Park JY, Kim DY, et al. Nonalcoholic fatty liver disease and sarcopenia are independently associated with cardiovascular risk. Am J Gastroenterol. 2020;115:584–95.
Bauer J, Morley JE, Schols AMWJ, Ferrucci L, Cruz-Jentoft AJ, Dent E, et al. Sarcopenia: A time for action. An SCWD Position Paper. J Cachexia Sarcopenia Muscle. 2019;10:956–61.
Sayer AA, Syddall H, Martin H, Patel H, Baylis D, Cooper C. The developmental origins of sarcopenia. J Nutr Health Aging. 2008;12:427–32.
Roubenoff R. Sarcopenic obesity: the confluence of two epidemics. Obes Res. 2004;12:887–8.
Shibuki T, Iida M, Harada S, Kato S, Kuwabara K, Hirata A, et al. The association between sleep parameters and sarcopenia in Japanese community-dwelling older adults. Arch Gerontol Geriatr. 2023;109:104948.
Zhang Z, Wang J, Wang J, Ma B, Jia Y, Chen O. Sleep duration affects the sequential change of body mass index and muscle strength: a contribution to dynapenic obesity. BMC Geriatr. 2023;23:288.
Piovezan RD, Hirotsu C, Moizinho R, de Sá Souza H, D’Almeida V, Tufik S, et al. Associations between sleep conditions and body composition states: results of the EPISONO study. J Cachexia Sarcopenia Muscle. 2019;10:962–73.
Wolfe RR. The underappreciated role of muscle in health and disease. Am J Clin Nutr. 2006;84:475–82.
Nanduri J, Wang N, Yuan G, Khan SA, Souvannakitti D, Peng YJ, et al. Intermittent hypoxia degrades HIF-2alpha via calpains resulting in oxidative stress: implications for recurrent apnea-induced morbidities. Proc Natl Acad Sci USA. 2009;106:1199–204.
DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009;32:S157–63.
Prabhakar NR, Peng YJ, Nanduri J. Hypoxia-inducible factors and obstructive sleep apnea. J Clin Invest. 2020;130:5042–51.
Lévy P, Pépin JL, Arnaud C, Tamisier R, Borel JC, Dematteis M, et al. Intermittent hypoxia and sleep-disordered breathing: current concepts and perspectives. Eur Respir J. 2008;32:1082–95.
Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy-Westphal A, et al. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr. 2014;33:929–36.
Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res. 1999;8:175–83.
Acknowledgements
We are grateful to all the subjects for their participation.
Funding
CL was funded by the Natural Science Foundation of China (NO. 82270928), the Fujian Provincial Health Science and Technology Project (No. 2022CXB016), and High-quality development Funds of The First Affiliated Hospital of Xiamen University (NO. YN81870611).
Author information
Authors and Affiliations
Contributions
The study concept and design were framed by XS and CL. XT conducted the statistical data analysis and drafted the manuscript. WL, RN, and WL contributed to the discussion. XS and CL contributed to the discussion and revision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The proposed study does not involve the collection of primary data. Accordingly, no ethical approval is required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tao, X., Niu, R., Lu, W. et al. Obstructive sleep apnea (OSA) is associated with increased risk of early-onset sarcopenia and sarcopenic obesity: Results from NHANES 2015-2018. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01493-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41366-024-01493-8