Abstract
Background
The Financial Incentives for Weight Reduction (FIReWoRk) clinical trial showed that financial incentive weight-loss strategies designed using behavioral economics were more effective than provision of weight-management resources only. We now evaluate cost-effectiveness.
Methods
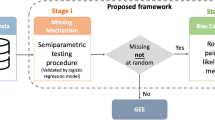
Cost-effectiveness analysis of a multisite randomized trial enrolling 668 participants with obesity living in low-income neighborhoods. Participants were randomized to (1) goal-directed incentives (targeting behavioral goals), (2) outcome-based incentives (targeting weight-loss), and (3) resources only, which were provided to all participants and included a 1-year commercial weight-loss program membership, wearable activity monitor, food journal, and digital scale. We assessed program costs, time costs, quality of life, weight, and incremental cost-effectiveness in dollars-per-kilogram lost.
Results
Mean program costs at 12 months, based on weight loss program attendance, physical activity participation, food diary use, self-monitoring of weight, and incentive payments was $1271 in the goal-directed group, $1194 in the outcome-based group, and $834 in the resources-only group (difference, $437 [95% CI, 398 to 462] and $360 [95% CI, 341–363] for goal-directed or outcome-based vs resources-only, respectively; difference, $77 [95% CI, 58–130] for goal-directed vs outcome-based group). Quality of life did not differ significantly between the groups, but weight loss was substantially greater in the incentive groups (difference, 2.34 kg [95% CI, 0.53–4.14] and 1.79 kg [95% CI, −0.14 to 3.72] for goal-directed or outcome-based vs resources only, respectively; difference, 0.54 kg [95% CI, −1.29 to 2.38] for goal-directed vs outcome-based). Cost-effectiveness of incentive strategies based on program costs was $189/kg lost in the goal-directed group (95% CI, $124/kg to $383/kg) and $186/kg lost in the outcome-based group (95% CI, $113/kg to $530/kg).
Conclusions
Goal-directed and outcome-based financial incentives were cost-effective strategies for helping low-income individuals with obesity lose weight. Their incremental cost per kilogram lost were comparable to other weight loss interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Individual participant data and data dictionary will be made available upon request, following approval of an analysis proposal by principal investigators. Statistical analysis code will be made available upon request.
References
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. NCHS Data Brief. 2020:1–8.
Dai H, Alsalhe TA, Chalghaf N, Ricco M, Bragazzi NL, Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: An analysis of the Global Burden of Disease Study. PLoS Med. 2020;17:e1003198.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129:S102–38.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Inc. G. Americans’ Effort to Lose Weight Still Trails Desire. Gallup.com (2014).
Kahwati LC, Lance TX, Jones KR, Kinsinger LS. RE-AIM evaluation of the Veterans Health Administration’s MOVE! Weight Management Program. Transl Behav Med. 2011;1:551–60.
Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;82:123–9.
Ladapo JA, Prochaska JJ. Paying Smokers to Quit: Does It Work? Should We Do It? J Am Coll Cardiol. 2016;68:786–8.
Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA. 2008;300:2631–7.
Kullgren JT, Troxel AB, Loewenstein G, Asch DA, Norton LA, Wesby L, et al. Individual- versus group-based financial incentives for weight loss: a randomized, controlled trial. Ann Intern Med. 2013;158:505–14.
Glanz K, Shaw PA, Kwong PL, Choi JR, Chung A, Zhu J, et al. Effect of Financial Incentives and Environmental Strategies on Weight Loss in the Healthy Weigh Study: A Randomized Clinical Trial. JAMA Netw Open. 2021;4:e2124132.
Yancy WS Jr, Shaw PA, Reale C, Hilbert V, Yan J, Zhu J, et al. Effect of Escalating Financial Incentive Rewards on Maintenance of Weight Loss: A Randomized Clinical Trial. JAMA Netw Open. 2019;2:e1914393.
Yancy WS Jr, Shaw PA, Wesby L, Hilbert V, Yang L, Zhu J, et al. Financial incentive strategies for maintenance of weight loss: results from an internet-based randomized controlled trial. Nutr Diabetes. 2018;8:33.
Patel MS, Asch DA, Troxel AB, Fletcher M, Osman-Koss R, Brady J, et al. Premium-Based Financial Incentives Did Not Promote Workplace Weight Loss In A 2013-15 Study. Health Aff (Millwood). 2016;35:71–9.
VanEpps EM, Troxel AB, Villamil E, Saulsgiver KA, Zhu J, Chin JY, et al. Effect of Process- and Outcome-Based Financial Incentives on Weight Loss Among Prediabetic New York Medicaid Patients: A Randomized Clinical Trial. Am J Health Promot. 2019;33:372–80.
Ries NM. Financial incentives for weight loss and healthy behaviours. Health Policy. 2012;7:23–8.
Jay M, Orstad SL, Wali S, Wylie-Rosett J, Tseng CH, Sweat V, et al. Goal-directed versus outcome-based financial incentives for weight loss among low-income patients with obesity: rationale and design of the Financial Incentives foR Weight Reduction (FIReWoRk) randomised controlled trial. BMJ open. 2019;9:e025278.
Ladapo JA, Orstad SL, Wali S, Wylie-Rosett J, Tseng CH, Chung UYR, et al. Effectiveness of goal-directed and outcome-based financial incentives for weight loss in primary care patients with obesity living in socioeconomically disadvantaged neighborhoods: A randomized clinical trial. JAMA Intern Med. 2023;183:61–9.
Kim TJ, von dem Knesebeck O. Income and obesity: what is the direction of the relationship? A systematic review and meta-analysis. BMJ Open. 2018;8:e019862.
Haff N, Patel MS, Lim R, Zhu J, Troxel AB, Asch DA, et al. The role of behavioral economic incentive design and demographic characteristics in financial incentive-based approaches to changing health behaviors: a meta-analysis. Am J Health Promot. 2015;29:314–23.
Finkelstein EA, Kruger E. Meta- and cost-effectiveness analysis of commercial weight loss strategies. Obesity (Silver Spring). 2014;22:1942–51.
Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG. Cost effectiveness in health and medicine, Second edition. edn Oxford University Press: Oxford ; New York, (2017).
Drummond MF. Methods for the economic evaluation of health care programmes, 3rd edn Oxford University Press: Oxford; New York, (2005).
Orstad SL, Gerchow L, Patel NR, Reddy M, Hernandez C, Wilson DK, et al. Defining Valid Activity Monitor Data: A Multimethod Analysis of Weight-Loss Intervention Participants’ Barriers to Wear and First 100 Days of Physical Activity. Informatics (MDPI). 2021;8:39.
U.S. Bureau of Labor Statistics. Employer Costs for Employee Compensation News Release - September 2022. In, (2022).
Hatziandreu EI, Koplan JP, Weinstein MC, Caspersen CJ, Warner KE. A cost-effectiveness analysis of exercise as a health promotion activity. Am J Public Health. 1988;78:1417–21.
Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63:1179–94.
Hanmer J. PROPr. In: https://github.com/janelhanmer/PROPr, (ed): janelhanmer, (2023).
Dewitt B, Jalal H, Hanmer J. Computing PROPr Utility Scores for PROMIS(R) Profile Instruments. Value Health. 2020;23:370–8.
Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ. 1997;6:327–40.
Efron B. Better bootstrap confidence intervals. J Am Stat Assoc. 1987;82:171–200.
Campbell MK, Torgerson DJ. Bootstrapping: estimating confidence intervals for cost-effectiveness ratios. QJM: Monthly J Assoc Physicians. 1999;92:177–82.
Chaudhary MA, Stearns SC. Estimating confidence intervals for cost-effectiveness ratios: an example from a randomized trial. Stat Med. 1996;15:1447–58.
Direito A, Carraca E, Rawstorn J, Whittaker R, Maddison R. mHealth Technologies to Influence Physical Activity and Sedentary Behaviors: Behavior Change Techniques, Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ann Behav Med. 2017;51:226–39.
Bodner TE. What Improves with Increased Missing Data Imputations? Struct Equ Modeling: A Multidisciplinary J. 2008;15:651–75.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30:377–99.
Kolotkin RL, Meter K, Williams GR. Quality of life and obesity. Obes Rev: Official J Int Assoc Stud Obes. 2001;2:219–29.
Rumsfeld JS, Alexander KP, Goff DC Jr, Graham MM, Ho PM, Masoudi FA, et al. Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation. 2013;127:2233–49.
Zhang P, Atkinson KM, Bray GA, Chen H, Clark JM, Coday M, et al. Within-Trial Cost-Effectiveness of a Structured Lifestyle Intervention in Adults With Overweight/Obesity and Type 2 Diabetes: Results From the Action for Health in Diabetes (Look AHEAD) Study. Diabetes Care. 2021;44:67–74.
Pollitz K. Trends in Workplace Wellness Programs and Evolving Federal Standards - Issue Brief. In: KFF, (2020).
Acknowledgements
This study was supported by the National Institutes of Health (NIH), National Institute on Minority Health and Health Disparities (NIMHD) through Grant Award Number R01MD011544 and National Center for Advancing Translational Sciences (NCATS) through Grant Award Number UL1TR001445. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Drs. Ladapo and Tseng had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author contributors
JAL and MJ were multiple principal investigators and SWa was a site principal investigator and were involved in all aspects of the study design, implementation, data interpretation, and writing. JAL, MJ, SLO, NRP, C-HT, SWi, JW-R, SBS and NJG developed data collection tools. JAL developed the analysis plan and JAL, C-HT and UYRC and C-HT analyzed and verified the data. JAL, C-HT, UYRC, MJ, SLO, NRP, SWa, JW-R, SBS, and NJG were involved in data interpretation. JAL drafted the paper. All coauthors critically reviewed and approved the final manuscript.
Funding
National Institutes of Health, R01MD011544 and National Center for Advancing Translational Sciences (NCATS), UL1TR001445.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ladapo, J.A., Orstad, S.L., Wylie-Rosett, J. et al. Cost-effectiveness of goal-directed and outcome-based financial incentives for weight loss in low-income populations: the FIReWoRk randomized clinical trial. Int J Obes 48, 231–239 (2024). https://doi.org/10.1038/s41366-023-01404-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01404-3