Abstract
Background
Obesity is a global pandemic disease whose prevalence is increasing worldwide. The clinical relevance of a polygenic risk score (PRS) for obesity has not been fully elucidated in Asian populations.
Method
We utilized a comprehensive health check-up database from the Korean population in conjunction with genotyping to generate PRS for BMI (PRS-BMI). We conducted a phenome-wide association (PheWAS) analysis and observed the longitudinal association of BMI with PRS-BMI.
Results
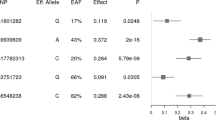
PRS-BMI was generated by PRS-CS. Adding PRS-BMI to a model predicting ten-year BMI based on age, sex, and baseline BMI improved the model’s accuracy (p = 0.003). In a linear mixed model of longitudinal change in BMI with aging, higher deciles of PRS were directly associated with changes in BMI. In the PheWAS, significant associations were observed for metabolic syndrome, bone density, and fatty liver. In the lean body population, those having the top 20% PRS-BMI had higher BMI and body fat mass along with better metabolic trait profiles compared to the bottom 20%. A bottom-20% PRS-BMI was a risk factor for metabolically unhealthy lean body (odds ratio 3.092, 95% confidence interval 1.707–6.018, p < 0.001), with adjustment for age, sex and BMI.
Conclusions
Genetic predisposition to obesity as defined by PRS-BMI was significantly associated with obesity-related disease or trajectory of obesity. Low PRS-BMI might be a risk factor associated with a metabolically unhealthy lean body. Better understanding the mechanisms of these relationships may allow tailored intervention in obesity or early selection of populations at risk of metabolic disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Complete raw data set are not publicly available due to restrictions (institutional policy to protect the privacy of research participants), but are available from the corresponding author on reasonable request. However, all other data are contained in the article and its supplementary information are available upon reasonable request.
References
Jung YS, Kim YE, Go DS, Yoon SJ. Projecting the prevalence of obesity in South Korea through 2040: a microsimulation modelling approach. BMJ Open. 2020;10:e037629.
Aggoun Y. Obesity, metabolic syndrome, and cardiovascular disease. Pediatr Res. 2007;61:653–9.
Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C, American Heart A, et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–8.
Bluher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–98.
Park JM, Park DH, Song Y, Kim JO, Choi JE, Kwon YJ, et al. Understanding the genetic architecture of the metabolically unhealthy normal weight and metabolically healthy obese phenotypes in a Korean population. Sci Rep. 2021;11:2279.
Osadnik K, Osadnik T, Lonnie M, Lejawa M, Regula R, Fronczek M, et al. Metabolically healthy obese and metabolic syndrome of the lean: the importance of diet quality. Analysis of MAGNETIC cohort. Nutr J. 2020;19:19.
Rotar O, Boyarinova M, Orlov A, Solntsev V, Zhernakova Y, Shalnova S, et al. Metabolically healthy obese and metabolically unhealthy non-obese phenotypes in a Russian population. Eur J Epidemiol. 2017;32:251–4.
Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 2020;8:616–27.
Stefan N. Metabolically healthy and unhealthy normal weight and obesity. Endocrinol Metab. 2020;35:487–93.
Stunkard AJ, Foch TT, Hrubec Z. A twin study of human obesity. JAMA. 1986;256:51–4.
Torkamani A, Topol E. Polygenic risk scores expand to obesity. Cell. 2019;177:518–20.
Joo YY, Actkins K, Pacheco JA, Basile AO, Carroll R, Crosslin DR, et al. A polygenic and phenotypic risk prediction for polycystic ovary syndrome evaluated by phenome-wide association studies. J Clin Endocrinol Metab. 2020;105:1918–36.
Khera AV, Chaffin M, Wade KH, Zahid S, Brancale J, Xia R, et al. Polygenic prediction of weight and obesity trajectories from birth to adulthood. Cell. 2019;177:587–96.e9.
Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Shai I, Jiang R, Manson JE, Stampfer MJ, Willett WC, Colditz GA, et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care. 2006;29:1585–90.
Kario K, Chen CH, Park S, Park CG, Hoshide S, Cheng HM, et al. Consensus document on improving hypertension management in asian patients, taking into account asian characteristics. Hypertension. 2018;71:375–82.
Lee C, Choe EK, Choi JM, Hwang Y, Lee Y, Park B, et al. Health and Prevention Enhancement (H-PEACE): a retrospective, population-based cohort study conducted at the Seoul National University Hospital Gangnam Center, Korea. BMJ Open. 2018;8:e019327.
Kanai M, Akiyama M, Takahashi A, Matoba N, Momozawa Y, Ikeda M, et al. Genetic analysis of quantitative traits in the Japanese population links cell types to complex human diseases. Nat Genet. 2018;50:390–400.
Ge T, Chen CY, Ni Y, Feng YA, Smoller JW. Polygenic prediction via Bayesian regression and continuous shrinkage priors. Nat Commun. 2019;10:1776.
World Health Organization. Regional Office for the Western Pacific. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia, 2000. https://apps.who.int/iris/handle/10665/206936.
Meyer-Lindenberg A, Weinberger DR. Intermediate phenotypes and genetic mechanisms of psychiatric disorders. Nat Rev Neurosci. 2006;7:818–27.
Flint J, Munafo MR. The endophenotype concept in psychiatric genetics. Psychol Med. 2007;37:163–80.
Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206.
Chatterjee N, Shi J, Garcia-Closas M. Developing and evaluating polygenic risk prediction models for stratified disease prevention. Nat Rev Genet. 2016;17:392–406.
Khera AV, Chaffin M, Aragam KG, Haas ME, Roselli C, Choi SH, et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat Genet. 2018;50:1219–24.
Dashti HS, Hivert MF, Levy DE, McCurley JL, Saxena R, Thorndike AN. Polygenic risk score for obesity and the quality, quantity, and timing of workplace food purchases: A secondary analysis from the ChooseWell 365 randomized trial. PLoS Med. 2020;17:e1003219.
Loos RJF, Janssens A. Predicting polygenic obesity using genetic information. Cell Metab. 2017;25:535–43.
Jung CH, Lee WY, Kim BY, Park SE, Rhee EJ, Park CY, et al. The risk of metabolic syndrome according to the white blood cell count in apparently healthy Korean adults. Yonsei Med J. 2013;54:615–20.
Kannel WB, Anderson K, Wilson PW. White blood cell count and cardiovascular disease. Insights from the Framingham Study. JAMA. 1992;267:1253–6.
Babio N, Ibarrola-Jurado N, Bullo M, Martinez-Gonzalez MA, Warnberg J, Salaverria I, et al. White blood cell counts as risk markers of developing metabolic syndrome and its components in the PREDIMED study. PLoS One. 2013;8:e58354.
Wu S, Lin H, Zhang C, Zhang Q, Zhang D, Zhang Y, et al. Association between erythrocyte parameters and metabolic syndrome in urban Han Chinese: a longitudinal cohort study. BMC Public Health. 2013;13:989.
Chang CC, Wu CH, Liu LK, Chou RH, Kuo CS, Huang PH, et al. Association between serum uric acid and cardiovascular risk in nonhypertensive and nondiabetic individuals: The Taiwan I-Lan Longitudinal Aging Study. Sci Rep. 2018;8:5234.
Shuster A, Patlas M, Pinthus JH, Mourtzakis M. The clinical importance of visceral adiposity: a critical review of methods for visceral adipose tissue analysis. Br J Radiol. 2012;85:1–10.
Chait A, den Hartigh LJ. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease. Front Cardiovasc Med. 2020;7:22.
Shah RV, Murthy VL, Abbasi SA, Blankstein R, Kwong RY, Goldfine AB, et al. Visceral adiposity and the risk of metabolic syndrome across body mass index: the MESA Study. JACC Cardiovasc Imaging. 2014;7:1221–35.
Tatsumi Y, Nakao YM, Masuda I, Higashiyama A, Takegami M, Nishimura K, et al. Risk for metabolic diseases in normal weight individuals with visceral fat accumulation: a cross-sectional study in Japan. BMJ Open. 2017;7:e013831.
Tchkonia T, Thomou T, Zhu Y, Karagiannides I, Pothoulakis C, Jensen MD, et al. Mechanisms and metabolic implications of regional differences among fat depots. Cell Metab. 2013;17:644–56.
Park J, Kim S. Validity of muscle-to-fat ratio as a predictor of adult metabolic syndrome. J Phys Ther Sci. 2016;28:1036–45.
Liu CC, Ko HJ, Liu WS, Hung CL, Hu KC, Yu LY, et al. Neutrophil-to-lymphocyte ratio as a predictive marker of metabolic syndrome. Medicine (Baltimore). 2019;98:e17537.
Sostaric A, Jenko B, Kozjek NR, Ovijac D, Suput D, Milisav I, et al. Detection of metabolic syndrome burden in healthy young adults may enable timely introduction of disease prevention. Arch Med Sci. 2019;15:1184–94.
Acknowledgements
We acknowledge Jong-Eun Lee of DNA Link for the collaborative support to establish the GENIE Cohort. This work has been supported by the NIGMS R01 GM138597.
Author information
Authors and Affiliations
Contributions
EKC, MS, SML, AV, and DK made contribution for conceptualization; EKC and MS curated the clinical and genomic data; EKC, MS, AV, and DK designed the study framework for methodology. EKC, MS, AV and DK analyzed and interpreted the results. EKC, MS were the major contributor in writing the manuscript. All authors read, provided critical feedback, helped shape the research, analysis, manuscript and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Choe, E.K., Shivakumar, M., Lee, S.M. et al. Dissecting the clinical relevance of polygenic risk score for obesity—a cross-sectional, longitudinal analysis. Int J Obes 46, 1686–1693 (2022). https://doi.org/10.1038/s41366-022-01168-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01168-2