Abstract
Background
Adolescent overweight and obesity are well documented in high-income countries (HICs). They are also emerging as a global public health concern in low-and middle-income countries (LMICs), yet there is a lack of reliable, national-level data to inform policies and interventions. This study aimed to estimate the prevalence of overweight and obesity and assess associated lifestyle risk factors amongst school-going adolescents in LMICs as well as HICs.
Methods
A total of 282,213 samples were drawn from 89 LMICs and HICs in the ‘latest Global School-based Student Health Survey’ of school children, aged 11–17 years, during 2003 to 2015, in the six World Health Organisation (WHO) regions. The prevalence of adolescent overweight and obesity were estimated using the WHO BMI-for-age growth standards. A multinomial logistic regression model was employed to estimate the adjusted (age and sex) association of food patterns, physical activity, and sedentary behaviours with adolescent overweight and obesity.
Results
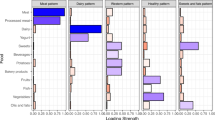
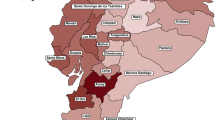
The pooled prevalence of overweight and obesity amongst adolescents was 10.12%, and 4.96%, respectively, ranging from 2.40% in Sri Lanka to 29.08% in Niue for overweight and 0.40% in Sri Lanka to 34.66% in the Cook Islands for obesity. Overweight and obesity were associated with unhealthy dietary intake and lifestyles including respectively fast-food intake (adjusted relative risk ratio, RRR = 1.09; 95% CI: 1.05–1.12 and RRR = 1.32; 95% CI: 1.26–1.38), a high level of carbonated soft drinks consumption (RRR = 1.19; 1.12–1.24 and RRR = 1.28; 1.18–1.38), a low level of physical activity (RRR = 1.11; 1.06–1.17 and 1.20; 1.12–1.28), and high level of sedentary behaviours (RRR = 1.33; 1.27–1.39 and RRR = 1.73; 1.63–1.84). Adolescents who consumed vegetables at least two times per day had a lower risk of overweight (22%) and obesity (17%) than those who did not consume vegetables per day.
Conclusions
Adolescent overweight and obesity represent a global public health problem and can possibly track into adult weight status and morbidity. School-based obesity prevention that promotes environmental and policy changes related to healthy dietary practices and active living are urgently needed to curb the trend.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5:4–104.
Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385:2510–20.
Development Initiatives. Global nutrition report: shining a light to spur action on nutrition. Bristol: Development Initiatives Poverty Research Ltd; 2018. https://globalnutritionreport.org/reports/
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Rankin J, Matthews L, Cobley S, Han A, Sanders R, Wiltshire HD, et al. Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolesc Health Med Ther. 2016;7:125–46.
Quek YH, Tam WWS, Zhang MWB, Ho RCM. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes Rev. 2017;18:742–54.
Randolph C. Being overweight or obese and the development of asthma. Pediatrics. 2019;144:S42–S43.
Schipper HS, Nuboer R, Prop S, Van Den Ham HJ, De Boer FK, Kesmir Ç, et al. Systemic inflammation in childhood obesity: circulating inflammatory mediators and activated CD14++ monocytes. Diabetologia. 2012;55:2800–10.
Biank V, Alemzadeh R. Pediatric non-alcoholic fatty liver disease. Liver Dis Peritonitis Causes Treat Prev. 2017;4:1–9.
Berardis S, Sokal E. Pediatric non-alcoholic fatty liver disease: an increasing public health issue. Eur J Pediatr. 2014;173:131–9.
Smith SM, Sumar B, Dixon KA. Musculoskeletal pain in overweight and obese children. Int J Obes. 2014;38:11–15.
Friedemann C, Heneghan C, Mahtani K, Thompson M, Perera R, Ward AM. Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ. 2012;345:1–16.
Brady TM. Obesity-related hypertension in children. Front Pediatr. 2017;5:1–7.
Cook S, Kavey REW. Dyslipidemia and pediatric obesity stephen. Pediatr Clin North Am. 2011;58:1363–73.
Raj M. Obesity and cardiovascular risk in children and adolescents. Indian J Endocrinol Metab. 2012;16:13.
Krul M, Van Der Wouden JC, Schellevis FG, Van Suijlekom-Smit LWA, Koes BW. Musculoskeletal problems in overweight and obese children. Ann Fam Med. 2009;7:352–6.
Must A, Jacques PF, Dallai GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard growth study of 1922 to 1935. N Engl J Med. 1992;327:1350–5.
Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa heart study. Pediatrics. 2001;108:712–8.
Tsai AG, Williamson DF, Glick HA. Direct medical cost of overweight and obesity in the United States: a quantitative systematic review. Obes Rev. 2011;12:50–61.
Osei-Assibey G, Dick S, MacDiarmid J, Semple S, Reilly JJ, Ellaway A et al. The influence of the food environment on overweight and obesity in young children: a systematic review. BMJ Open. 2012; 2. https://doi.org/10.1136/bmjopen-2012-001538.
World Health Organization (WHO). Comprehensive Implementation Plan On Maternal, Infant And Young Child Nutrition. Department of Nutrition for Health and Development. Geneva, Switzerland: WHO; 2014.
World Health Organization (WHO). Global school-based student health survey (GSHS). Noncommunicable Diseases their risk factors; 2020. https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/global-school-based-student-health-survey
The Wold Bank. World Bank country and lending groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
World Health Organization (WHO). Growth reference 5–19 years. Body mass index (BMI)-for-age (5–19 years); 2007. https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age
van Draanen J, Prelip M, Upchurch DM. Consumption of fast food, sugar-sweetened beverages, artificially-sweetened beverages and allostatic load among young adults. Prev Med Rep. 2018;10:212–7.
Just DR, Wansink B. Fast food, soft drink and candy intake is unrelated to body mass index for 95% of American adults. Obes Sci Pract. 2015;1:126–30.
Galimov A, Hanewinkel R, Hansen J, Unger JB, Sussman S, Morgenstern M. Association of energy drink consumption with substance-use initiation among adolescents: a 12-month longitudinal study. J Psychopharmacol. 2020;34:221–8.
An R, He L, Shen MSJ. Impact of neighbourhood food environment on diet and obesity in China: a systematic review. Public Health Nutr. 2019;23:457–73.
Shah T, Purohit G, Nair SP, Patel B, Rawal Y, Shah RM. Assessment of obesity, overweight and its association with the fast food consumption in medical students. J Clin Diagn Res. 2014;8:7–9.
Al-Otaibi HH, Basuny AM. Fast food consumption associated with obesity/overweight risk among University female students in Saudi Arabia. Pakistan J Nutr. 2015;14:511–6.
Mohammadbeigi A, Asgarian A, Moshir E, Heidari H, Afrashteh S, Khazaei S, et al. Fast food consumption and overweight/obesity prevalence in students and its association with general and abdominal obesity. J Prev Med Hyg. 2018;59:236–40.
Jéquier E. Is fat intake a risk factor for fat gain in children? J Clin Endocrinol Metab. 2001;86:980–3.
Fumeron F, Lamri A, Khalil CA, Jaziri R, Porchay-Baldérelli I, Lantieri O, et al. Dairy consumption and the incidence of hyperglycemia and the metabolic syndrome: results from a French prospective study, data from the epidemiological study on the insulin resistance syndrome (DESIR). Diabetes Care. 2011;34:813–7.
Tucker LA, Erickson A, Lecheminant JD, Bailey BW. Dairy consumption and insulin resistance: the role of body fat, physical activity, and energy intake. J Diabetes Res. 2015;2015:206959.
Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357:505–8.
McNutt SW, Yuanreng H, Schreiber GB, Crawford PB, Obarzanek E, Mellin L. A longitudinal study of the dietary practices of black and white girls 9 and 10 years old at enrollment: the NHLBI Growth and Health Study. J Adolesc Health. 1997;20:27–37.
Ebbiling CB, Pawluk D, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–82.
French SA, Story M, Neumark-Sztainer D, Fulkerson JA, Hannan P. Fast food restaurant use among adolescents: associations with nutrient intake, food choices and behavioral and psychosocial variables. Int J Obes. 2001;25:1823–33.
Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364:2392–404.
He K, Hu FB, Colditz GA, Manson JE, Willett WC, Liu S. Changes in intake of fruits and vegetables in relation to risk of obesity and weight gain among middle-aged women. Int J Obes. 2004;28:1569–74.
Bertoia ML, Mukamal KJ, Cahill LE, Hou T, Ludwig DS, Mozaffarian D, et al. Changes in intake of fruits and vegetables and weight change in United States men and women followed for up to 24 years: analysis from three prospective cohort studies. PLoS Med. 2015;12:1–20.
Nour M, Lutze SA, Grech A, Allman-Farinelli M The relationship between vegetable intake and weight outcomes: A systematic review of cohort studies. Nutrients 2018; 10. https://doi.org/10.3390/nu10111626.
Ockene IS, Nicolosi R, Hegsted DM, Johnson RK, Black AE, Hu FB, et al. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med. 1998;338:917–9.
World Health Organization (WHO). WHO launches plan to eliminate industrially-produced trans-fatty acids from global food supply; 2018. https://www.world-heart-federation.org/news/launches-plan-eliminate-industrially-produced-trans-fatty-acids-global-food-supply/#:~:text=The World Heart Federation welcomes, from the global food supply.
Tremblay MS, Willms JD. Is the Canadian childhood obesity epidemic related to physical inactivity? Int J Obes. 2003;27:1100–5.
Hernández B, Gortmaker SL, Colditz GA, Peterson KE, Laird NM, Parra-Cabrera S. Association of obesity with physical activity, television programs and other forms of video viewing among children in Mexico City. Int J Obes. 1999;23:845–54.
Ortega FB, Ruiz JR, Castillo MJ, Sjöström M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes. 2008;32:1–11.
Hills AP, Andersen LB, Byrne NM. Physical activity and obesity in children. Br J Sports Med. 2011;45:866–70.
Zhang X, Zhang F, Yang J, Yang W, Liu W, Gao L, et al. Prevalence of overweight and obesity among primary school-aged children in Jiangsu Province, China, 2014–2017. PLoS ONE. 2018;13:2014–7.
Abarca-Gómez L, Abedeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Karki A, Shrestha A, Subedi N. Prevalence and associated factors of childhood overweight/obesity among primary school children in urban Nepal. BMC Public Health. 2019;19:1–12.
Cesare DM, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. 2019;17:1–20.
Strong WB, Malina RM, Blimkie CJR, Daniels SR, Dishman RK, Gutin B, et al. Evidence based physical activity for school-age youth. J Pediatr. 2005;146:732–7.
Barnett LM, Morgan PJ, van Beurden E, Beard JR. Perceived sports competence mediates the relationship between childhood motor skill proficiency and adolescent physical activity and fitness: a longitudinal assessment. Int J Behav Nutr Phys Act. 2008;5:1–12.
Johnson MS, Figueroa-colon R, Herd SL, Fields DA, Sun M, Hunter GR, et al. Aerobic fitness, not energy expenditure, influences subsequent increase in adiposity in black and white children. Pediatrics. 2000;106:1–6.
Elgar FJ, Roberts C, Tudor-Smith C, Moore L. Validity of self-reported height and weight and predictors of bias in adolescents. J Adolesc Health. 2005;37:371–5.
Stommel M, Schoenborn CA. Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001-2006. BMC Public Health. 2009;9:1–10.
Sherry B, Jefferds ME, Grummer-Strawn LM. Accuracy of adolescent self-report of height and weight in assessing overweight status: a literature review. Arch Pediatr Adolesc Med. 2007;161:1154–61.
Matias TS, Silva KS, Da Silva JA, De Mello GT, Salmon J. Clustering of diet, physical activity and sedentary behavior among Brazilian adolescents in the national school-based health survey (PeNSE 2015). BMC Public Health. 2018;18:1–9.
Leech RM, McNaughton SA, Timperio A. The clustering of diet, physical activity and sedentary behavior in children and adolescents: a review. Int J Behav Nutr Phys Act. 2014;11:1–9.
Khan A, Dix C, Burton NW, Khan SR, Uddin R. Association of carbonated soft drink and fast food intake with stress-related sleep disturbance among adolescents: a global perspective from 64 countries. EClinicalMedicine. 2020;000:100681.
Acknowledgements
This research paper was drafted and completed during the first author’s postdoctoral-1 research works under the School of Social Science, Western Sydney University, Australia. The revision of this manuscript was performed during the first author’s postdoctoral-2 (health economics) research works under NHMRC Clinical Trials Centre, the School of Medicine and Health, the University of Sydney, Australia. We would also like to thank the global school-based student health survey for providing access to the data utilised in the research. Finally, we would like to gratefully acknowledge the study’s participants, reviewers, and the academic editors of our manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualised the study: RAM; Contributed data extraction and analyses: RAM under the guidance of RLM and AMNR. Result interpretation: RAM, under the guidance of RLM and AMNR. Prepared the first draft: RAM, BWS, EOA, WC and AMNR. Contributed during the conceptualisation and interpretation of results and substantial revision: RAM, AMNR and RLM. Revised and finalised the final manuscript: RAM, BWS, EOA, WC, RLM and AMNR. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahumud, R.A., Sahle, B.W., Owusu-Addo, E. et al. Association of dietary intake, physical activity, and sedentary behaviours with overweight and obesity among 282,213 adolescents in 89 low and middle income to high-income countries. Int J Obes 45, 2404–2418 (2021). https://doi.org/10.1038/s41366-021-00908-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00908-0