Abstract
Objective
Chemerin has been suggested as a potential link between obesity and associated comorbidities in humans. Therefore, we studied the relationships between chemerin, parameters of fat mass, and Metabolic Syndrome (MetS) in obese children before and after weight reduction.
Methods
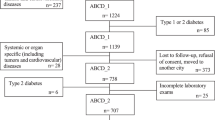
We determined chemerin, bioactive leptin (bioLep), BMI-SDS, waist circumference (WC), body fat based on skinfold measurements and bioimpedance analyses, lipids, transaminases, insulin resistance index HOMA, and blood pressure in 88 obese children participating in a lifestyle intervention at baseline and 1 year later. Furthermore, we determined chemerin concentrations in 23 normal-weight children.
Results
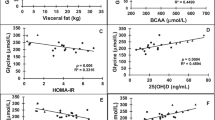
Obese children demonstrated significantly (p < 0.001) higher chemerin concentrations compared to normal-weight children (96.2 ± 23.0 versus 63.1 ± 12.4 ng/ml). The chemerin concentrations were not related to age or gender. Prepubertal children had higher (p = 0.024) chemerin concentrations than pubertal children (71.0 ± 13.4 versus 58.0 ± 8.9 ng/ml). Weight loss was associated with a decrease of chemerin (−14.0 ± 22.0 ng/ml; p < 0.001) and an improvement of all parameters of the MetS. Chemerin was significantly related to BMI-SDS, WC, and bioLep in cross-sectional and longitudinal analyses. Chemerin and its changes were significantly related to insulin, HDL-cholesterol, triglycerides and their changes in multiple linear regression analyses adjusted to age, gender, pubertal stage, leptin and BMI.
Conclusions
Since chemerin was related to parameters of central fat mass and MetS both in cross-sectional and longitudinal analyses these findings suggest an impact of chemerin on factors of the MetS in obese children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Wittamer V, Franssen JD, Vulcano M, Mirjolet JF, Le PE, Migeotte I, et al. Specific recruitment of antigen-presenting cells by chemerin, a novel processed ligand from human inflammatory fluids. J Exp Med. 2003;198:977–85.
Gavrieli A, Mantzoros CS. Novel molecules regulating energy homeostasis: physiology and regulation by macronutrient intake and weight loss. Endocrinol Metab. 2016;31:361–72.
Goralski KB, McCarthy TC, Hanniman EA, Zabel BA, Butcher EC, Parlee SD, et al. Chemerin, a novel adipokine that regulates adipogenesis and adipocyte metabolism. J Biol Chem. 2007;282:28175–88.
Bozaoglu K, Bolton K, McMillan J, Zimmet P, Jowett J, Collier G, et al. Chemerin is a novel adipokine associated with obesity and metabolic syndrome. Endocrinology. 2007;148:4687–94.
Takahashi M, Takahashi Y, Takahashi K, Zolotaryov FN, Hong KS, Kitazawa R, et al. Chemerin enhances insulin signaling and potentiates insulin-stimulated glucose uptake in 3T3-L1 adipocytes. FEBS Lett. 2008;582:573–8.
Weigert J, Neumeier M, Wanninger J, Filarsky M, Bauer S, Wiest R, et al. Systemic chemerin is related to inflammation rather than obesity in type 2 diabetes. Clin Endocrinol. 2010;72:342–8.
Bozaoglu K, Segal D, Shields KA, Cummings N, Curran JE, Comuzzie AG, et al. Chemerin is associated with metabolic syndrome phenotypes in a Mexican-American population. J Clin Endocrinol Metab. 2009;94:3085–8.
Sell H, Divoux A, Poitou C, Basdevant A, Bouillot JL, Bedossa P, et al. Chemerin correlates with markers for fatty liver in morbidly obese patients and strongly decreases after weight loss induced by bariatric surgery. J Clin Endocrinol Metab. 2010;95:2892–6.
Sell H, Laurencikiene J, Taube A, Eckardt K, Cramer A, Horrighs A, et al. Chemerin is a novel adipocyte-derived factor inducing insulin resistance in primary human skeletal muscle cells. Diabetes. 2009;58:2731–40.
Lehrke M, Becker A, Greif M, Stark R, Laubender RP, von ZF, et al. Chemerin is associated with markers of inflammation and components of the metabolic syndrome but does not predict coronary atherosclerosis. Eur J Endocrinol. 2009;161:339–44.
Landgraf K, Friebe D, Ullrich T, Kratzsch J, Dittrich K, Herberth G, et al. Chemerin as a mediator between obesity and vascular inflammation in children. J Clin Endocrinol Metab. 2012;97:E556–E564.
Sledzinska M, Szlagatys-Sidorkiewicz A, Brzezinski M, Kazmierska K, Sledzinski T, Kaminska B. Serum chemerin in children with excess body weight may be associated with ongoing metabolic complications - a pilot study. Adv Med Sci. 2017;62:383–6.
Hamza RT, Elkabbany ZA, Shedid AM, Hamed AI, Ebrahim AO. Serum chemerin in obese children and adolescents before and after L-carnitine therapy: relation to nonalcoholic fatty liver disease and other features of Metabolic Syndrome. Arch Med Res. 2016;47:541–9.
Redondo MJ, Rodriguez LM, Haymond MW, Hampe CS, Smith EO, Balasubramanyam A, et al. Serum adiposity-induced biomarkers in obese and lean children with recently diagnosed autoimmune type 1 diabetes. Pediatr Diabetes. 2014;15:543–9.
Daxer J, Herttrich T, Zhao YY, Vogel M, Hiemisch A, Scheuermann K, et al. Nocturnal levels of chemerin and progranulin in adolescents: influence of sex, body mass index, glucose metabolism and sleep. J Pediatr Endocrinol Metab. 2017;30:57–61.
Maghsoudi Z, Kelishadi R, Hosseinzadeh-Attar MJ. Association of chemerin levels with anthropometric indexes and C-reactive protein in obese and non-obese adolescents. ARYA Atheroscler. 2015;11:102–8.
Terra X, Auguet T, Guiu-Jurado E, Berlanga A, Orellana-Gavalda JM, Hernandez M, et al. Long-term changes in leptin, chemerin and ghrelin levels following different bariatric surgery procedures: Roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg. 2013;23:1790–8.
Ress C, Tschoner A, Engl J, Klaus A, Tilg H, Ebenbichler CF, et al. Effect of bariatric surgery on circulating chemerin levels. Eur J Clin Invest. 2010;40:277–80.
Chakaroun R, Raschpichler M, Kloting N, Oberbach A, Flehmig G, Kern M, et al. Effects of weight loss and exercise on chemerin serum concentrations and adipose tissue expression in human obesity. Metabolism. 2012;61:706–14.
Hron BM, Ebbeling CB, Feldman HA, Ludwig DS. Hepatic, adipocyte, enteric and pancreatic hormones: response to dietary macronutrient composition and relationship with metabolism. Nutr Metab. 2017;14:44.
Bluher M, Rudich A, Kloting N, Golan R, Henkin Y, Rubin E, et al. Two patterns of adipokine and other biomarker dynamics in a long-term weight loss intervention. Diabetes Care. 2012;35:342–9.
Khoo J, Dhamodaran S, Chen DD, Yap SY, Chen RY, Tian RH. Exercise-induced weight loss is more effective than dieting for improving adipokine profile, insulin resistance, and inflammation in obese men. Int J Sport Nutr Exerc Metab. 2015;25:566–75.
Maghsoudi Z, Kelishadi R, Hosseinzadeh-Attar MJ. The comparison of chemerin, adiponectin and lipid profile indices in obese and non-obese adolescents. Diabetes Metab Syndr. 2016;10:S43–S46.
Ye Z, Wang S, Yang Z, He M, Zhang S, Zhang W, et al. Serum lipocalin-2, cathepsin S and chemerin levels and nonalcoholic fatty liver disease. Mol Biol Rep. 2014;41:1317–23.
Reinehr T, Hinney A, de SG, Austrup F, Hebebrand J, Andler W. Definable somatic disorders in overweight children and adolescents. J Pediatr. 2007;150:618–22.
Reinehr T, de Sousa G, Toschke AM, Andler W. Long-term follow-up of cardiovascular disease risk factors in children after an obesity intervention. Am J Clin Nutr. 2006;84:490–6.
Guidelines of the German Society of Pediatric Endocrinology and Diabetes. http://www.awmf.org/leitlinien/aktuelle-leitlinien/ll-liste/deutsche-gesellschaft-fuer-kinderendokrinologie-und-diabetologie-dgked.html (Accessed January 2018).
Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7:284–94.
Kromeyer-Hauschild K, Wabitsch M, Geller F, Ziegler A, Geiss HC, Hesse V, et al. Percentiles of body mass index in children and adolescents evaluated from different regional German studies. Mon Kinderheilkd. 2001;149:807–18.
Reinehr T, Lass N, Toschke C, Rothermel J, Lanzinger S, Holl RW. Which amount of BMI-SDS reduction is necessary to improve cardiovascular risk factors in overweight children? J Clin Endocrinol Metab. 2016;101:3171–9.
Slaughter M, Lohmann T, Boileau R, Horswill C, Stillmann R, Bemben D. Skinfold equations for estimation of body fatness in children and youth. Hum Biol. 1998;60:709–23.
Haroun D, Croker H, Viner RM, Williams JE, Darch TS, Fewtrell MS, et al. Validation of BIA in obese children and adolescents and re-evaluation in a longitudinal study. Obesity. 2009;17:2245–50.
Kromeyer- Hausschild K, Gläßer N, Zellner K. Waist circumference percentile in Jena children (Germany) 6 to 18 years of age. Aktuel Ernaehr Med. 2008;33:116–22.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76.
Niklowitz P, Rothermel J, Lass N, Barth A, Reinehr T. Bioactive leptin is stronger related to parameters of fat mass and distribution than conventionally measured leptin: findings from a longitudinal study in obese children participating in a lifestyle intervention. Clin Chim Acta. 2018;480:225–9.
Wabitsch M, Pridzun L, Ranke M, von SJ, Moss A, Brandt S, et al. Measurement of immunofunctional leptin to detect and monitor patients with functional leptin deficiency. Eur J Endocrinol. 2017;176:315–22.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
American Diabetes Association: 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018 Jan; 41(Suppl 1):S13–S27.
American Gastroenterological Association. American Gastroenterological Association medical position statement: nonalcoholic fatty liver disease. Gastroenterology. 2002;123:1702–4.
Reinehr T, Elfers C, Lass N, Roth CL. Irisin and its relation to insulin resistance and puberty in obese children: a longitudinal analysis. J Clin Endocrinol Metab. 2015;100:2123–30.
Reinehr T, Roth CL. Fetuin-A and its relation to metabolic syndrome and fatty liver disease in obese children before and after weight loss. J Clin Endocrinol Metab. 2008;93:4479–85.
Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr. 1990;44:45–60.
Rosario AS, Schienkiewitz A, Neuhauser H. German height references for children aged 0 to under 18 years compared to WHO and CDC growth charts. Ann Hum Biol. 2011;38:121–30.
Neuheuser H, Schienkiewitz A, Schaffrath Rosario A, Dortschy R, Kurth B. Referenzperzentile für anthropometrische Maßzahlen und Blutdruck aus der Studie zurGesundheit von Kindern und Jugendlichen in Deutschland (KiGGS). www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GBEDownloadsB/KiGGS_Referenzperzentilepdf?__blob=publicationFile (accessed January 2018).
Oswiecimska JM, Ziora KT, Suwala A, Swietochowska E, Gorczyca P, Ziora-Jakutowicz K, et al. Chemerin serum levels in girls with anorexia nervosa. Neuro Endocrinol Lett. 2014;35:490–6.
Shin HY, Lee DC, Chu SH, Jeon JY, Lee MK, Im JA, et al. Chemerin levels are positively correlated with abdominal visceral fat accumulation. Clin Endocrinol. 2012;77:47–50.
Bozaoglu K, Curran JE, Stocker CJ, Zaibi MS, Segal D, Konstantopoulos N, et al. Chemerin, a novel adipokine in the regulation of angiogenesis. J Clin Endocrinol Metab. 2010;95:2476–85.
Kolonin MG, Saha PK, Chan L, Pasqualini R, Arap W. Reversal of obesity by targeted ablation of adipose tissue. Nat Med. 2004;10:625–32.
Rupnick MA, Panigrahy D, Zhang CY, Dallabrida SM, Lowell BB, Langer R, et al. Adipose tissue mass can be regulated through the vasculature. Proc Natl Acad Sci USA. 2002;99:10730–5.
Becker M, Rabe K, Lebherz C, Zugwurst J, Goke B, Parhofer KG, et al. Expression of human chemerin induces insulin resistance in the skeletal muscle but does not affect weight, lipid levels, and atherosclerosis in LDL receptor knockout mice on high-fat diet. Diabetes. 2010;59:2898–903.
Lee MK, Chu SH, Lee DC, An KY, Park JH, Kim DI, et al. The association between chemerin and homeostasis assessment of insulin resistance at baseline and after weight reduction via lifestyle modifications in young obese adults. Clin Chim Acta. 2013;421:109–15.
Yin C, Chu H, Li H, Xiao Y. Plasma Sfrp5 and adiponectin levels in relation to blood pressure among obese children. J Hum Hypertens. 2017;31:284–91.
Kralisch S, Weise S, Sommer G, Lipfert J, Lossner U, Bluher M, et al. Interleukin-1beta induces the novel adipokine chemerin in adipocytes in vitro. Regul Pept. 2009;154:102–6.
Tan BK, Chen J, Farhatullah S, Adya R, Kaur J, Heutling D, et al. Insulin and metformin regulate circulating and adipose tissue chemerin. Diabetes. 2009;58:1971–7.
Ernst MC, Issa M, Goralski KB, Sinal CJ. Chemerin exacerbates glucose intolerance in mouse models of obesity and diabetes. Endocrinology. 2010;151:1998–2007.
Catalan V, Gomez-Ambrosi J, Rodriguez A, Ramirez B, Rotellar F, Valenti V, et al. Increased levels of chemerin and its receptor, chemokine-like receptor-1, in obesity are related to inflammation: tumor necrosis factor-alpha stimulates mRNA levels of chemerin in visceral adipocytes from obese patients. Surg Obes Relat Dis. 2013;9:306–14.
Imai K, Takai K, Hanai T, Shiraki M, Suzuki Y, Hayashi H, et al. Impact of serum chemerin levels on liver functional reserves and platelet counts in patients with hepatocellular carcinoma. Int J Mol Sci. 2014;15:11294–306.
Yilmaz Y, Yonal O, Kurt R, Alahdab YO, Eren F, Ozdogan O, et al. Serum levels of omentin, chemerin and adipsin in patients with biopsy-proven nonalcoholic fatty liver disease. Scand J Gastroenterol. 2011;46:91–97.
Chen HY, Lin CC, Chiu YL, Hsu SP, Pai MF, Yang JY, et al. Serum fetuin A and chemerin levels correlate with hepatic steatosis and regional adiposity in maintenance hemodialysis patients. PLoS ONE. 2012;7:e38415.
Klusek-Oksiuta M, Bialokoz-Kalinowska I, Tarasow E, Wojtkowska M, Werpachowska I, Lebensztejn DM. Chemerin as a novel non-invasive serum marker of intrahepatic lipid content in obese children. Ital J Pediatr. 2014;40:84.
Mohamed AA, Sabry S, Abdallah AM, Elazeem NAA, Refaey D, Algebaly HAF, et al. Circulating adipokines in children with nonalcoholic fatty liver disease: possible noninvasive diagnostic markers. Ann Gastroenterol. 2017;30:457–63.
Koerner A, Kratzsch J, Kiess W. Adipocytokines: leptin--the classical, resistin--the controversical, adiponectin--the promising, and more to come. Best Pract Res Clin Endocrinol Metab. 2005;19:525–46.
Uysal Y, Wolters B, Knop C, Reinehr T. Components of the metabolic syndrome are negative predictors of weight loss in obese children with lifestyle intervention. Clin Nutr. 2014;33:620–5.
Reinehr T. Metabolic Syndrome in children and adolescents: a critical approach considering the interaction between pubertal stage and insulin resistance. Curr Diab Rep. 2016;16:8.
Magge SN, Goodman E, Armstrong SC The Metabolic Syndrome in children and adolescents: shifting the focus to cardiometabolic risk factor clustering. Pediatrics 2017. Jul 24. pii: e20171603. https://doi.org/10.1542/peds.2017-1603. [Epub ahead of print]
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Niklowitz, P., Rothermel, J., Lass, N. et al. Link between chemerin, central obesity, and parameters of the Metabolic Syndrome: findings from a longitudinal study in obese children participating in a lifestyle intervention. Int J Obes 42, 1743–1752 (2018). https://doi.org/10.1038/s41366-018-0157-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0157-3
This article is cited by
-
Alternative splicing is not a key source of chemerin isoforms diversity
Molecular Biology Reports (2023)
-
The dietary inflammatory index is associated with anti- and pro-inflammatory adipokines in Brazilian schoolchildren
European Journal of Nutrition (2021)
-
Pro- and anti-inflammatory adipokines are associated with cardiometabolic risk markers in Brazilian schoolchildren
European Journal of Pediatrics (2021)
-
Special Issue: 2019 Consortium for Trans-Pyrenean Investigations on Obesity and Diabetes
Journal of Physiology and Biochemistry (2021)
-
Chemerin enhances the adhesion and migration of human endothelial progenitor cells and increases lipid accumulation in mice with atherosclerosis
Lipids in Health and Disease (2020)