Key Points
-
During blood-stage infections, Plasmodium parasites infect erythrocytes and can cause a variety of acute and chronic complications, some of which can be fatal. Although malaria complications are often attributed to sepsis-like systemic inflammation, the parasites in the circulation reach and interact with host tissues locally and specifically.
-
The brain, eye (retina), gastrointestinal tract, bones, lungs, kidneys and placenta are the organs that are specifically affected both during and even long after malaria infection. The unique anatomical structure of the vessels, parenchyma and lymphatics in each organ shapes the interaction with Plasmodium parasites and their products.
-
In the brain, unique areas such as the olfactory bulb, retina and perivascular spaces share similar anatomical and immunological features; Plasmodium parasites and their associated inflammation cause blood–brain barrier disruption in these areas.
-
The gastrointestinal tract microenvironment is a target of Plasmodium parasites and related events. Malaria infection causes the disruption of blood vessels and epithelial barriers in the gut.
-
Plasmodium parasites can reside in the bone marrow. At this site, the parasites and their products, such as haemozoin, interact with bone marrow niches and with cells resident in the bone tissue, including osteoblasts and osteoclasts, causing long-term effects in the host, such as bone loss.
-
The interactions that occur between Plasmodium parasites and the specific host tissues alter the outcome of malaria disease. A better understanding of malaria pathology in the context of host–parasite interactions at the various tissue levels of each organ will allow for better diagnostics and treatments for malaria.
Abstract
Systemic inflammation mediated by Plasmodium parasites is central to malaria disease and its complications. Plasmodium parasites reside in erythrocytes and can theoretically reach all host tissues via the circulation. However, actual interactions between parasitized erythrocytes and host tissues, along with the consequent damage and pathological changes, are limited locally to specific tissue sites. Such tissue specificity of the parasite can alter the outcome of malaria disease, determining whether acute or chronic complications occur. Here, we give an overview of the recent progress that has been made in understanding tissue-specific immunopathology during Plasmodium infection. As knowledge on tissue-specific host–parasite interactions accumulates, better treatment modalities and targets may emerge for intervention in malaria disease.
Similar content being viewed by others
Introduction
In the second decade of the 21st century, humankind still suffers greatly from mosquito-borne diseases, including malaria1,2. Despite advances in combined malaria control and elimination programmes1,3, there were approximately 438,000 deaths due to malaria worldwide in 2015, 90% of them in the African continent and 10% of them in southeast Asia4. These figures place malaria among the top three lethal infectious diseases of humans, together with tuberculosis and HIV1,5.
Malaria is a disease caused by Plasmodium parasites, with acute symptoms ranging from recurrent fever, headache, muscle and joint pain, vomiting, jaundice and anaemia to severe complications such as acidosis, respiratory distress, severe anaemia, kidney failure and cerebral malaria. In humans, it is caused by five Plasmodium species: P. falciparum, P. vivax, P. ovale, P. malariae and P. knowlesi, each of which causes a wide range of clinical symptoms and distinct complications (Table 1). The disease symptoms mainly occur during the blood-stage infection when erythrocytes, the only host cell that parasites can invade and multiply within (with the exception of the pre-erythrocytic hepatocyte stage), are infected. P. falciparum malaria accounts for 80% of malaria cases in sub-Saharan Africa and is considered the deadliest of all malarial species, causing cerebral malaria, respiratory distress and severe anaemia. By contrast, P. vivax malaria accounts for >50% of malaria cases outside of Africa and generally occurs with milder symptoms, but complications such as severe anaemia are not uncommon6,7. Detailed genetic analysis of Plasmodium spp. has also led to the recognition that P. knowlesi, which causes malaria in monkeys, can also be transmitted to humans and might be life threatening, with symptoms such as acute lung and kidney failure8,9.
Why and how malaria infection causes sudden and life-threatening complications has not been fully clarified. For example, the sequestration of parasitized erythrocytes (hereafter referred to as infected red blood cells (iRBCs)) in blood vessels within host tissues is well correlated with disease severity, but the parasite and/or host-mediated factors that contribute to iRBC sequestration have not been fully determined, although P. falciparum erythrocyte membrane protein 1 (PfEMP1) and receptors expressed on activated host endothelial cells are known to contribute10. Such factors may affect not only cerebral malaria, in which P. falciparum parasites are known to be sequestrated in the brain vessels and retina of humans11, but also the pathology in other organs that are characterized by high levels of iRBC sequestration, including the gastrointestinal tract, lungs, kidneys and skin11,12,13. Importantly, these complications could leave survivors with long-term health problems such as cognitive and neurological deficits14,15.
Another important question in malaria research remains: after an initial systemic infection, why do most individuals develop only partial immunity over the years and suffer from only mild symptoms with low parasitaemia16? In other words, why and how does Plasmodium infection exploit host immunity, allowing reinfection of the same individual again and again? The expansion of atypical memory B cell populations and an exhaustion of CD4+ T cell responses have been reported in malaria-endemic regions17,18,19. Hence, growing evidence suggests that the chronic illness caused by incomplete immunity to malaria causes long-term hidden pathologies20. One such pathology is Burkitt lymphoma, a cancer that develops in both childhood and adulthood in Africa and that is closely related to P. falciparum and Epstein–Barr virus co-endemicicity21. The robust and long-lasting expansion of germinal centre B cell populations that occurs during Plasmodium infection may induce increased activation-induced cytidine deaminase (AID) expression, eventually leading to chromosomal translocations22,23,24 that predispose to the development of lymphoma in immune tissues.
An increasing recognition of the association between malaria infection and physical growth retardation in children in Africa, regardless of nutritional status25,26, suggests a detrimental effect of chronic malaria infection on growth, possibly via an effect on the bone tissue environment27. Nevertheless, any Plasmodium spp. causing infection in humans result in varying degrees of complications, which can not only be severe and life threatening but can also have a long-term impact on patients' quality of life even after recovery.
In this Review, we focus on how systemic infection by Plasmodium parasites causes local but tissue-specific immunopathologies during the blood stage of infection, mainly through the manipulation of inter-tissue interactions between the blood and other host tissues that often result in dysfunction of certain, but not all, organs. Acute systemic immune activation, such as pro-inflammatory cytokine production, lymphocyte activation and vessel congestion, is evident; however, how these pathological events affect each tissue or organ is not understood well. Current interventions for malaria are based on the administration of antimalarial drugs aimed at killing parasites and on supportive care to reduce systemic symptoms, such as coma, high fever, severe anaemia and acidosis. In this Review, we emphasize the need to focus on host interactions with Plasmodium parasites at various tissue levels and the importance of targeting local and specific organ failure and/or pathologies during, as well as long after, infection. These pathologies might be critical for determining diagnostic as well as therapeutic targets for the development of novel adjunct therapies to be used in combination with current antimalarials. We describe new evidence and new ways of targeting infected tissues of a few, but not all, unique organs such as the brain, gut and bones. We initially summarize how the blood tissue plays a central role in the initial pathogenesis caused by Plasmodium parasites, following which we explore the interaction of infected blood tissue with specific organs composed of multiple, unique interacting tissue layers. Largely owing to limitations of space, topics regarding the sporozoite stages of infection in the liver and those on the innate immune recognition of Plasmodium parasites28,29 are out of the scope of this Review. In fact, Plasmodium parasites do possess several ligands used to manipulate host cell invasion that could potentially be exploited as host factor targets for anti-malaria therapy30,31, a notion close to the topic of this Review, but we exclude and leave this to an excellent recent article focusing on this topic32.
Pathology within the blood tissue
Blood is a tissue (Box 1) that is formed by the plasma and blood cells (that is, erythrocytes, platelets and leukocytes) and is primarily located in the blood vessels. The infection of erythrocytes by Plasmodium parasites results in extensive erythrocyte remodelling and dysfunction followed by cell lysis, which contribute to the pathology of severe anaemia.
Anaemia. Plasmodium parasites (a merozoite form) are released into the bloodstream from liver hepatocytes within specialized vesicles called merosomes33 and continue a repetitive erythrocyte-invasion cycle in the blood tissue. Merozoites released from the liver enter into erythrocytes through a very dynamic and complex process34,35 (Fig. 1). Once erythrocytic infection is established, continuous destruction of erythrocytes due to schizont rupture contributes to anaemia. A moderate degree of anaemia is caused simply by the naturally occurring life cycle of parasites in erythrocytes. However, studies in both humans and mice have clearly indicated an increased removal of infected and uninfected erythrocytes that plays an essential and major role in severe malarial anaemia36,37,38. Clinical observations and mathematical modelling have suggested that for each infected erythrocyte, approximately 10 uninfected RBCs are removed during malaria infection (34 for P. vivax infection and 8 for P. falciparum infection)39,40 because of a reduced uninfected erythrocyte half-life and increased clearance by the spleen41. Reduced deformability, dyserythropoiesis and alterations in erythropoietic progenitor populations are commonly observed during malaria infection37. Chronic anaemia may also be mediated by the generation of self-reactive anti-phosphatidylserine antibodies42. Phosphatidylserine on infected erythrocytes is thought to be pathologically exposed to the immune system during malaria, leading to the generation of anti-phosphatidylserine antibodies. Under usual circumstances, uninfected erythrocytes, mainly young cells called reticulocytes, express high levels of CD47, a 'do not eat me' signal43,44, which allows them to escape from phagocytosis. However, young erythrocytes generated during malaria expose phosphatidylserine earlier, thus leading anti-phosphatidylserine antibodies to bind to uninfected erythrocytes and facilitate their clearance, contributing to chronic anaemia.
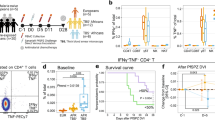
Following the release of Plasmodium merozoites from infected hepatocytes into the bloodstream, repetitive erythrocyte-invasion cycles occur in the blood. This leads to the release of several parasite by-products, such as haemozoin, and the parasites themselves into the bloodstream. The blood-stage cycle of Plasmodium infection causes various pathologies, such as anaemia, toxic haem release, immune cell activation (modulation of platelets, neutrophils, monocytes, macrophages, T cells and B cells) and can cause a cytokine and chemokine storm. In blood tissue, infected red blood cells (iRBCs) and their products may interact with other infected and uninfected RBCs (causing rosetting), or they may interact with immune cell populations (causing a cytokine storm) or with the endothelial cells of blood vessels (causing RBC sequestration and microhaemorrhage). These cell–cell interactions have organ specificity and thus take place in specific tissue environments, resulting in specific immunopathologies.
One of the outcomes of the destruction of high numbers of erythrocytes during malaria is an increase in intravascular haem release45,46, which is an important factor for neutrophil activation47 but in turn could be the reason for increased oxidative damage and thus decreased macrophage function and the neutrophil exhaustion observed during malaria. This implies that not only erythrocytes but also blood tissue components including various leukocytes collectively react to the presence of Plasmodium parasites (covered previously by seminal review articles35,48,49) and their related products in the blood circulation and tissues (Fig. 1).
Sequestration and inflammation. Erythrocytes undergo extensive deformation and remodelling after invasion by Plasmodium parasites. While remodelling allows nutrient acquisition and parasite growth, it leads to changes in erythrocyte structure, with an increase in rigidity50 and rosetting51. Hence, the mature schizont stages easily sequester in the host microvasculature, mostly during P. falciparum and P. knowlesi infection and to a lesser extent during P. vivax infection50, whereas immature ring stages freely circulate in the vessels. Plasmodium berghei ANKA infection in mice shows a similar sequestration phenotype52,53,54,55, and in this instance, sequestration via CD36 may be beneficial for the survival of the parasite56. It is believed that infected erythrocytes, mostly those in the schizont stages of parasite infection, adhere along with activated leukocytes (mainly CD8+ T cells) to the endothelial cells of small blood vessels in the brain via binding to CD36, intercellular adhesion molecule 1 (ICAM1), endothelial protein C receptor (EPCR) and platelet endothelial cell adhesion molecule (PECAM1)57,58,59,60. However, endothelial cell activation can occur without direct adhesion of leukocytes to the endothelial cells, possibly as a result of metabolites produced by leukocytes or parasites61. Indeed, there are unidentified soluble factors released by iRBCs that cause endothelial cell pathology62. In line with this, endothelial cells, iRBCs, platelets, leukocytes and monocytes were shown to increase their release of extracellular vesicles during Plasmodium infection, and this contributed to inflammation and correlated with disease severity63. Extracellular vesicles are mostly released from iRBCs during schizogony and contain RBC components, parasite proteins and various RNAs that can activate innate immune cells64. In addition, endothelial cells have been shown to act as antigen-presenting cells (APCs) through the phagocytosis of merozoites and the presentation of malarial antigens to CD8+ T cells, which leads to IFNγ-mediated and perforin-mediated disruption of the blood–brain barrier (BBB)61.
Most of these models of malaria-induced pathology are still under debate, and more evidence from both humans and animal models is clearly needed. Overall, while the process of sequestration is not completely understood, it is known to cause obstruction of blood flow in small capillaries and post-capillary venules (PCVs), endothelial cell activation and inflammation and severe pathology in many organs including lung, adipose tissue, spleen and brain52,53,65,66 (Fig. 1).
Blood vessels and lymphatics. Blood, including Plasmodium-infected erythrocytes, is transported to organs via blood vessels. Between large arteries and veins, various smaller sized vessels such as arterioles, capillaries and PCVs are present and have a role in controlling blood pressure and velocity in organs (Fig. 2a). The speed of blood flow substantially decreases as the blood enters arterioles, drops dramatically again in the capillaries and then slightly increases in the venules and veins (Fig. 2a). Depending on the size and tissue environment, blood vessel structures vary. Generally, the smaller the diameter of the vessel, the less smooth muscle it contains. Capillaries, which play a major role in exchanging materials in blood, are the smallest vessels and are composed of endothelial cells with firm tight junctions and a basement membrane and do not include a smooth muscle layer (Fig. 2b). Unlike capillaries, PCVs may have a few thin smooth muscle layers (Fig. 2c). Importantly, depending on the organ, capillaries and PCVs interact with additional cells in tissues (Fig. 2d). For instance, brain capillaries and PCVs are additionally surrounded by pericytes, astrocyte end-feet and microglia (Fig. 2d). In particular, PCVs differ from capillaries in that they have leakier tight junctions and thus, may create perivascular spaces that APCs can easily home to67 and that allow for the infiltration of inflammatory cells during inflammatory conditions68. Moreover, the capillary beds in various organs are mostly in close proximity to lymphatic capillaries, into which drain interstitial fluid (ISF; mainly leukocytes) and materials coming from blood vessels. The ISF drained into the lymphatic vessels reaches the lymph nodes and finally returns to the final destination veins (Fig. 2a). Therefore, it is reasonable to think that the type and diameter of a blood vessel in a specific organ in addition to the specific connective tissue and smooth muscle that is present to support vessel integrity may determine the degree of sequestration of Plasmodium parasites and the outcome of disease. The walls of the smallest capillaries and PCVs are presumably more susceptible to internal changes occurring in the vessels. Therefore, in the following sections, we detail the blood vessels within a few organs, such as the brain, gut and bones, and highlight their unique involvement with iRBCs during malaria.
a | Infected red blood cells (iRBCs) circulate in blood vessels, which vary in size from large arteries to veins, with blood flow running from arteries, arterioles, capillaries and post-capillary venules (PCVs) to venules and veins, providing controlled blood pressure and velocity in organs. The speed of blood flow is lowest in capillaries and PCVs. In various organs, these capillary beds are mostly near lymphatic vessels, through which interstitial fluid and materials coming from blood vessels drain the lymph nodes and finally return to veins. iRBCs and iRBC-mediated immune responses, therefore, may have profound effects on these smaller vascular beds in each organ. b | Capillaries have only an endothelial cell wall and no smooth muscle; therefore, they are in close contact with iRBCs. c | Two capillaries fuse and form PCVs, which may have some smooth muscle and where leukocyte rolling can occur. d | Capillaries and PCVs in the brain are additionally surrounded by pericytes, astrocyte end-feet and microglia; iRBC-related events in capillaries are sensed immediately.
Tissue pathology within the brain
The brain is severely affected by P. falciparum infection and to a lesser extent by P. knowlesi and P. vivax infections. This unique brain pathology, known as cerebral malaria, involves convulsions, coma and high fever and develops with the presence of mostly ring-stage infected erythrocytes in the periphery (suggesting a sequestration of late-stage parasites in the organs)69,70,71. Disruption of BBB integrity is an established outcome in cerebral malaria and may cause brain swelling and death in both humans and animals72,73. The activation of blood tissue components and their effect on brain immune cells (microglia, astrocytes) have been addressed53,74,75,76,77,78,79,80, but how an obligate erythrocyte-resident pathogen can cause BBB disruption is not well understood. Although the brain is considered an immune-privileged organ that is protected by the presence of the tight and selective BBB and by the lack of lymphatic drainage (a notion that has been disputed recently81,82), the loss of BBB integrity due to the direct invasion and inflammation of meninges by various extracellular pathogens is well known83.
To understand why and how brain tissue is affected during malaria, we should consider recent advances in the neuroscience field, which could help to expand our understanding of cerebral malaria pathogenesis and development. The central nervous system (CNS) is composed of the brain and spinal cord, which are protected by the meninges (formed by three layers: dura mater, arachnoid mater and pia mater) and are associated with two types of fluids: cerebrospinal fluid (CSF) running through the subarachnoid space and ISF in the brain and spinal cord parenchyma (Box 2). CSF is derived from plasma but has far fewer proteins, no erythrocytes, very few leukocytes and higher sodium, chloride and magnesium contents. ISF fills the basement membranes of brain capillaries, where most of the exchange between blood and the CNS occurs. The selective BBB inside the brain blood vessels, especially capillaries, is composed of uniquely specialized endothelial cells with intracellular tight junctions, pericytes, astrocyte end-feet and microglia in addition to the basement membrane, suggesting that blood vessel structures in the brain differ from those in other organs of the body, with a unique involvement of brain cell astrocytes and microglia in disease processes84 (Fig. 2d). Advancing our understanding of brain physiology (Box 2) clearly has important implications for neurological diseases, such as Alzheimer disease and multiple sclerosis85,86, as well as for cerebral malaria. Indeed, recent preclinical studies using cutting-edge imaging technologies, such as ultra-high-field 11.7 T magnetic resonance imaging (MRI) and multiphoton live imaging microscopy, in experimental cerebral malaria models have expanded our understanding of how cerebral malaria develops. Below, we consider the roles of the retina, olfactory bulb and the perivascular spaces of the brain during cerebral malaria.
Perivascular spaces and cerebral malaria. Arteries supplying blood to the brain divide into smaller arteries on the pial surface and penetrate into the brain parenchyma before further dividing into arterioles. Arterioles (and venules) are surrounded by perivascular space which is filled with ISF drained from the brain parenchyma (Fig. 3a). A newly defined 'glymphatic system' has been proposed in which the glia limitans, a barrier comprising astrocyte end-feet that surrounds small capillaries and veins, creates perivascular spaces via aquaporin 4 (AQP4) channels. The AQP4 channels facilitate the flux of ISF into perivascular spaces to be mixed with CSF87,88, and this eventually contributes to the clearance of particles from the CSF. Interestingly, dilatation at perivascular spaces and astroglia and reduced expression of AQP4 protein have been reported during cerebral malaria in animal models89,90. Furthermore, in the absence of AQP4, mice with cerebral malaria succumbed to death more quickly90, suggesting AQP4 has protective roles during cerebral malaria, perhaps in controlling liquid exchange, oedema and cell transmigration at the BBB.
a | Small arteries on the pial surface of the brain penetrate into the brain parenchyma and further divide into arterioles; these are surrounded by perivascular space (PVS) which is filled with interstitial fluid (ISF) that has drained from the brain parenchyma. Arterioles become capillaries, venules then veins, which finally drain into dural venous sinuses, and each of these areas potentially contain abundant infected red blood cells (iRBCs), as well as lymphocytes such as CD8+ T cells. Lymphatic vessels located in the dura carry immune cells and cerebrospinal fluid (CSF) into deep cervical lymph nodes. b | The retina is rich in photoreceptors (cones, bipolar cells and ganglions), nerve cells and complex blood vessels, especially capillary structures surrounded by Müller cells, a retina-specific astrocyte-like cell. The optic nerve serves as a connector between the retinal nervous tissue and the brain, where meningeal membranes, dura lymphatics and CSF cover the optic nerve up to the retina border. This area may contain abundant iRBCs. c | The olfactory bulb is surrounded by meninges of brain dura and arachnoid and pial layers. CSF similarly runs throughout the bulb and reaches the cribriform plate area. Olfactory nerves originate from the nasal mucosa and terminate in the olfactory bulb through the cribriform plate, which is also the route of the blood vessels surrounding the olfactory nerves. These olfactory nerves project any signal for smell to the olfactory bulb and the brain. Inside the olfactory bulb, very dense blood capillaries are oriented in different directions (radially and tangentially), with thin astrocyte end-feet surrounding the vessels, and sense iRBC-related events and secrete several cytokines and/or chemokines including CC-chemokine ligand 21 (CCL21). Blood capillaries easily bleed during cerebral malaria. PCV, post-capillary venule.
APCs with phagocytic properties such as dendritic cells and macrophages located in the pial surfaces and perivascular spaces have been shown to present antigens to T cells in various CNS diseases91. As visualized by electron microscopy and intravital two-photon microscopy, it seems that leukocytes and CD8+ T cells, and probably iRBCs or their products, increasingly accumulate in perivascular spaces in very deep and branching vessels during cerebral malaria92,93,94,95. These phagocytic APCs and activated endothelial cells in vessels have the capacity to present malarial antigens96,97. Furthermore, all these events that are mediated by IFNγ could be reversed by blocking the adhesion molecules very late antigen 4 (VLA4) and lymphocyte function-associated antigen 1 (LFA1) (ligands for vascular endothelial adhesion protein 1 (VCAM1) and ICAM1, respectively), which are expressed on activated CD8+ T cells during cerebral malaria98. One of the important features of inflammation in perivascular spaces is that the parasite and inflammatory products may directly activate astrocytes53,99, microglia77 and neurons100, and may cause an increase in the levels of protein S100B (a biomarker for astrocytes) and in the levels of the microtubule-associated protein tau (a biomarker for degenerated axons) in CSF80. Nevertheless, future studies are needed to provide direct evidence of this. It would also be interesting to investigate in the future whether there are other types of perivascular spaces found at different locations in the brain101,102, because pia mater also covers the cerebellum and other CNS areas, such as the spinal cord. Therefore, the interaction of perivascular spaces with small blood vessels may vary depending on the anatomical location and unique architecture of the tissue, for example, in the brain cortex, spinal cord, cerebellum or olfactory bulb.
The retina and cerebral malaria. The back of the eye ball is lined by the retina, with the optic nerve in the middle and going through to the brain. The optic nerve serves as a connector between the nervous tissue of the retina and the brain, where brain meninges, dura mater lymphatics and CSF cover up the optic nerve up until the retina border. The retina is rich in photoreceptors, nerve cells and complex blood vessels, especially capillary structures (Fig. 3b). Retinal changes (such as haemorrhages, multiple peripheral and macular patchy whitening areas and papilloedema) have been commonly observed in children and in adults who develop sudden comatose cerebral malaria symptoms after a few days of fever103,104,105. These retinal changes occur in areas that show high sequestration of parasites accompanied by thrombi (composed of fibrin and platelets)106,107, which cause impaired capillary perfusion108,109 and are well correlated with the severity of disease110. Interestingly, other areas in the eye, such as the optic nerve head, ciliary body and iris, are similarly affected by iRBCs110, indicating that specific blood vessel similarities may occur within other parts of the brain. Retinal homeostasis is maintained through neurovascular coupling involving astrocytes, Müller cells (a specific type of glial cell found in the retina) and resident retinal microglia, with Müller cells, pericytes and astrocytes mainly ensheathing the retinal blood capillaries111. The observation that the accumulation of fluid between processes of Müller cells and photoreceptor cells in the macular area produces intra-retinal spaces in human cerebral malaria107 suggests that these areas represent perivascular-space-like areas in the retina that support immunological events similar to those that occur in the perivascular spaces in deep brain areas. Furthermore, high-field MRI studies have identified damage to the optic and trigeminal nerves during experimental cerebral malaria even before the development of oedema, which may cause loss of visual acuity112.
The olfactory bulb and cerebral malaria. The olfactory bulb is situated on the cribriform plate, located on top of the nasal sinus. Although the olfactory bulb has several characteristics that distinguish it from the brain, it is covered by similar meningeal structures and by the CSF and is thus included in the CNS. However, in contrast to other parts of the brain, olfactory nerves initiate from the nasal mucosa and terminate in the olfactory bulb through the cribriform plate, which is also the route of the blood vessels surrounding olfactory nerves. These olfactory nerves project any signals for odour to the olfactory bulb and to the brain. Inside the olfactory bulb, very dense blood capillaries are oriented in different directions (radially and tangentially) with thin astrocyte end-feet surrounding the vessels (Fig. 3c). Owing to complex structural interactions of nerves through the cribriform plate, capillaries, microglia and astrocyte end-feet in this region, the olfactory organ is considered to be the gateway of the otherwise well-protected brain to the outside world. It is known that several molecules, cells and even pathogens can gain access to the brain parenchyma through this route113.
By use of 11.7 T MRI in mice, it was discovered that the olfactory bulb is the first region during experimental cerebral malaria to show vascular leakage and bleeding53, a phenomenon possibly related to the unique small capillary trabecular structure of the olfactory bulb. This was also directly visualized and confirmed by intravital two-photon microscopy during cerebral malaria53. These dense and directionally structured olfactory blood capillaries114, which are thought to be leakier than those in the brain cortex or pons115, are a suitable scaffold for iRBCs53. Sequestration of iRBCs in the olfactory bulb capillaries results in astrocyte and microglia activation53,76,98 and in the loss of tight junction integrity, and these parasite-mediated events lead to olfactory dysfunction and loss of smell, which could be a valuable early diagnostic marker for cerebral malaria. Moreover, astrocytes surrounding small trabecular capillaries in the olfactory bulb were found to sense changes in the vessels and secrete cytokines and chemokines, such as CC-chemokine ligand 21 (CCL21), which are involved in the accumulation of pathological CXCR3+CD8+ T cells in the olfactory bulb53. Expression of CC-chemokine receptor 7 (CCR7), which is the canonical receptor for CCL21 and CCL19, was shown to be essential for antigen cross-presentation by CD8α+ dendritic cells and for the activation of CXCR3+CD8+ T cells in the spleen during cerebral malaria53. By contrast, CCL21 secreted from astrocytes played a role in the recruitment of pathological CXCR3+CD8+ T cells in the olfactory bulb via its non-canonical receptor CXCR3 (Ref. 53). A pathological role for several chemokines and chemokine receptors (including CXC-chemokine ligand 4 (CXCL4), CXCL10 and CXCR3) is well recognized in experimental cerebral malaria116, but the study discussed above53 highlights how the specific role for chemokines in cerebral malaria might differ depending on the tissue and organ environment. Extended MRI studies using sensitive contrast reagents have further confirmed these findings and have shown that micro-haemorrhages originate in the olfactory bulb together with oedema, but that the oedema further spreads along the rostral migratory stream, similar to the migration route of immune cells and neuroblasts76, and may reach the brainstem98. Moreover, the glymphatic system may play a key role in the rapid inflammatory spread of cerebral malaria from the olfactory bulb and rostral migratory stream axis to deeper brain areas such as perivascular spaces76. It is also possible that these events that occur in the olfactory bulb during cerebral malaria may block the drainage of CSF into nasal lymphatics and aggravate brain oedema (Fig. 3c). Clearly, the role of the olfactory bulb in cerebral malaria in humans warrants further research.
Tissue pathology within the gut
Gastrointestinal symptoms such as abdominal pain, vomiting and diarrhoea are common symptoms during malaria infection. Autopsies of human patients who died from severe malaria have shown that sequestration of iRBCs occurs in the gastrointestinal tract (including in the colon, jejunum, ileum and stomach)13, suggesting that gastrointestinal bleeding occurs during malaria. The presence of Plasmodium DNA in faeces additionally supports the occurrence of intestinal bleeding during infection117; however, how parasites interact with other cells in gut tissue is a research area that has only recently gained attention.
Recent studies have confirmed that pathological changes (including detachment of epithelia and shortening of villi and the colon) occur in the intestinal tract during malaria118; such changes may cause increased intestinal permeability, ruptures and leakage of infected erythrocytes into the lumen, causing dysbiosis of the intestinal microbiota, which may also contribute to disease severity118. Moreover, there is a close correlation between malaria infection and increased rates of infection with other gut pathogens (for example, non-typhoidal Salmonella and helminths), possibly owing to an impairment of intestinal barrier function during malaria119,120,121. Several factors may have a role in this, such as increased histamine release from mast cells in the gut122 or the modulation of intestinal inflammation and immune responses via an increase in the number of exhausted neutrophils45 or an increase in the levels of IL-10 family cytokines, including IL-10 and IL-22, in the intestinal tissues during malaria infection, as these factors may ameliorate responses to secondary bacterial infections123,124,125. However, it should be kept in mind that the composition of the gut microbiota has a clear impact on the severity of malaria disease126,127,128, suggesting that there is a bidirectional relation between the gut and Plasmodium parasites that is not well understood and requires further investigation.
Nevertheless, a close look at the intestinal tissues may give some clues for understanding gut–Plasmodium interactions (Fig. 4a). The blood capillaries carrying iRBCs reach the lamina propria of the intestinal mucosa and possibly come into close proximity with lacteals, which are specialized lymphatic vessels of intestinal villi that play a key role in nutrient absorption and in gut immune responses, such as the transport of microbial antigens and APCs to the mesenteric lymph nodes, where antigen presentation by APCs promotes the induction of T cells with gut-homing properties129. There is a gut–vascular barrier comprising endothelial cells, enteric pericytes and enteric glial cells that is very similar to the barriers found in other parts of the body (such as the BBB) and that actively blocks bacterial dissemination from the gut epithelium to the blood130. Therefore, it is reasonable to hypothesize that intestinal bleeding may occur as a result of malaria-mediated immune responses that directly affect lacteals. It is possible that lacteals with disturbed remodelling have impaired survival and villi length118, and this may have knock-on effects on immune cell composition and on the microbiota of the gut tissue.
a | The intestinal tract is made up of several tissue layers. The villous mucosa is covered by mucus that is secreted by the goblet cells of the epithelium. It lies on a connective tissue, the lamina propria, which is an environment rich in blood vessels, lymphatics, nerves and immune cells. It also contains Peyer's patches and is lined by smooth muscle tissue (muscularis mucosa). Blood capillaries that are carrying infected red blood cells (iRBCs) reach the lamina propria of the intestinal tract and can come into close proximity with lacteals at this location. b | Bone tissue supports the whole body and is home to bone cells, blood vessels, nerves and endothelium, as well as containing the bone marrow niches. The bone marrow is composed of haematopoetic and mesenchymal stem cells that are involved in both haematopoiesis and bone remodelling, such as osteoclasts and osteoblasts. Cells and iRBCs pass through the circulation and bone marrow via specialized venules called bone marrow sinusoids. Plasmodium parasites can invade erythroblasts, the erythrocyte precursors, and preferentially form gametocytes in the bone marrow erythroblastic niche. Released Plasmodium products including haemozoin can be engulfed by osteoclasts and activate osteoblasts and osteoclast precursors. HSC, haematopoietic stem cell; MSC, mesenchymal stem cell; OSB, osteoblast.
Tissue pathology within bone
Bone tissue is a mineralized connective tissue supporting the whole body and it houses the bone marrow, which comprises specialized niches that maintain and regulate haematopoiesis, erythropoiesis and bone remodelling (Fig. 4b). Arteries in the bone marrow unite and become specialized vessels called bone marrow sinusoids, which allow cells to pass between the circulation and bone marrow131. Without any cytoadherence, Plasmodium parasites can invade and multiply in nucleated erythroblasts located in extravascular spaces of the bone marrow132,133,134. The parasites can survive and hide in these erythroid precursors and develop into gametocyte stages135,136,137, likely assisting in the continuous success of malaria transmission to mosquitoes. However, it is still not known why Plasmodium parasites preferentially differentiate into gametocytes in the bone marrow and whether a specific bone marrow niche is required to support the development of gametocytes. Unlike haematopoietic niches, which are located adjacent to sinusoids, erythroid niches are found throughout the bone marrow and are generally located away from the sinusoids, although they move closer to the sinusoids as they mature138. This may suggest a major role for the erythroid niche in Plasmodium gametocyte development. From an immunological point of view, it has recently been shown that CD8+ T cells produce IFNγ in response to infected MHC class I-expressing erythroblasts residing in the bone marrow; by contrast, mature erythrocytes residing in the blood circulation lack any MHC molecules and cannot present antigens to CD8+ T cells132,139. Activated CD8+ T cells promote the exposure of phosphatidylserine on infected erythroblasts, and this enhances the susceptibility of the infected cells to phagocytosis by macrophages132, suggesting a protective role of CD8+ T cells against malaria. However, whether bone marrow erythroid cells contribute to the expansion of pathological populations of CD8+ T cells that can drive cerebral malaria has not been investigated.
Despite the growing body of information on how bone marrow niches are manipulated by Plasmodium parasites, very little is known about the potential outcomes of interactions between Plasmodium parasites and bone tissue. In bone marrow, haematopoietic stem cells give rise to blood cells and bone-resident osteoclasts, whereas mesenchymal stem cells give rise to osteoblasts, adipocytes and stromal cells. A very recent study has suggested that during Plasmodium infection, parasites and their products — mainly haemozoin — continuously accumulate in bone marrow and cause acute as well as chronic bone loss27. Although it is not precisely known how Plasmodium products are retained long term in the bone marrow, it is possible that engulfment by macrophages or other phagocytic cells, such as bone-resident osteoclasts, or trapping by extracellular matrix in the bone marrow contributes to this phenomenon27. Chronic bone loss during malaria infection is mediated by over-activation of osteoclast resorption activity. The osteoclasts are activated by the key osteoclastogenic cytokine RANKL (also known as TNFSF11), which is upregulated in osteoblasts through MYD88-dependent signalling triggered by the persistence of parasite products in the bone marrow27. These findings highlight how, not only during acute malaria infection but also after recovery from infection, Plasmodium products continue to interact with tissue-resident cells, including bone cells, osteoclasts and osteoblasts, and how they can cause long-term effects in the host, such as bone loss and growth problems. The molecular and immunological pathways underlying the interaction between Plasmodium spp. and the niches of various bone marrow cells and the effect of these interactions on the immune system140,141 need to be addressed in the future.
Conclusions and perspective
Malaria is a serious disease with acute life-threatening and long-term complications, all of which can be attributed to local but specific organs in which Plasmodium parasites and their products or iRBCs interact with the tissue, causing an imbalance in the specific tissue environment. Here, we have attempted to summarize the recent progress of research focusing on the tissue environment in a few example organs, such as the brain, gut and bone, where Plasmodium parasites reach the tissue via the blood. However, the lungs142, kidneys143 and placenta144 represent other organs that are seriously affected during malaria infection, and these tissues should also be examined more closely in future studies. Here, our aim has been to show that the influence of malarial parasites reaches beyond erythrocytes and may vary depending on, and be tightly regulated by, the vessel-specific and/or tissue-specific microenvironment. On the basis of the available data, we suggest that the brain pathology caused by Plasmodium parasites is not homogeneously controlled by parasite sequestration but is rather controlled by the local, specific and unique anatomical structure of vessels, parenchyma and lymphatics, which closely interact with each other during both homeostasis and infection. This concept is in accordance with the recent understanding that the vascular and epithelial barriers do cooperate in an organ-specific manner in homeostatic and diseased conditions130. We additionally emphasize that parasite-derived products can continue to stay in the body, interact with tissues and cause chronic pathologies even long after recovery from infection, particularly in the case of bone tissue. The gut pathology caused by malaria, which has recently been recognized, was summarized, and the possible anatomical interaction between blood tissues and special gut lymphatics has been introduced.
There are multiple benefits of understanding malaria-related pathologies in various tissues. For instance, understanding the reaction of microglia and astrocytes to iRBCs will be beneficial for generating intervention strategies that block these interactions to prevent cerebral malaria and/or related long-term sequelae. Supporting the gut microbiota during and after Plasmodium infection might help to protect against and promote recovery from secondary infections. Similarly, additional therapies like vitamin D3 supplementation to support the bone environment affected during and after malaria might help the growth of children or support bone health in elderly people.
The search for a full understanding of malaria-related pathologies is important for ensuring that malaria is one day a curable and/or preventable disease. Towards this goal, novel approaches should be investigated to analyse unknown or overlooked anatomical — as well as immunological — host–parasite interactions at various tissue levels of each organ, not only during infection but also long after clearance of the initial infection by the parasite. By doing so, we will be able to prevent the disease, diagnose and treat patients, predict prognoses and allow patients to receive appropriate medical care through the use of effective vaccines, diagnostic tools, adjunct therapies and antimalarials in a cost-effective and timely manner in the near future.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Murray, C. J. L. et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 1005–1070 (2014).
Hempelmann, E. & Krafts, K. Bad air, amulets and mosquitoes: 2,000 years of changing perspectives on malaria. Malar. J. 12, 232 (2013).
Gething, P. W. et al. Mapping Plasmodium falciparum mortality in Africa between 1990 and 2015. N. Engl. J. Med. 375, 2435–2445 (2016).
World Health Organization. World Malaria Report 2015 (WHO, 2015).
Pigott, D. M. et al. Prioritising infectious disease mapping. PLoS Negl. Trop. Dis. 9, e0003756 (2015).
Naing, C., Whittaker, M. A., Nyunt Wai, V. & Mak, J. W. Is Plasmodium vivax malaria a severe malaria?: a systematic review and meta-analysis. PLoS Negl. Trop. Dis. 8, e3071 (2014).
Arévalo-Herrera, M. et al. Clinical profile of Plasmodium falciparum and Plasmodium vivax infections in low and unstable malaria transmission settings of Colombia. Malar. J. 14, 154 (2015).
Millar, S. B. & Cox-Singh, J. Human infections with Plasmodium knowlesi — zoonotic malaria. Clin. Microbiol. Infect. 21, 640–648 (2015).
Seilmaier, M. et al. Severe Plasmodium knowlesi infection with multi-organ failure imported to Germany from Thailand/Myanmar. Malar. J. 13, 422 (2014).
Storm, J. & Craig, A. G. Pathogenesis of cerebral malaria — inflammation and cytoadherence. Front. Cell. Infect. Microbiol. 4, 100 (2014).
Milner, D. A. et al. The systemic pathology of cerebral malaria in African children. Front. Cell. Infect. Microbiol. 4, 104 (2014). This is an important human study that systematically identifies the sequestration of parasites in not only the brain, but also many other parts of the human body during cerebral malaria.
Milner, D. et al. Pulmonary pathology in pediatric cerebral malaria. Hum. Pathol. 44, 2719–2726 (2013).
Milner, D. A. et al. Quantitative assessment of multiorgan sequestration of parasites in fatal pediatric cerebral malaria. J. Infect. Dis. 212, 1317–1321 (2015). This is an important study that quantifies multi-organ sequestration of parasites in fatal human malaria.
Boivin, M. J. et al. Cognitive impairment after cerebral malaria in children: a prospective study. Pediatrics 119, e360–e366 (2007).
Roze, E. et al. Neurologic sequelae after severe falciparum malaria in adult travelers. Eur. Neurol. 46, 192–197 (2001).
Marsh, K. & Kinyanjui, S. Immune effector mechanisms in malaria. Parasite Immunol. 28, 51–60 (2006).
Illingworth, J. et al. Chronic exposure to Plasmodium falciparum is associated with phenotypic evidence of B and T cell exhaustion. J. Immunol. 190, 1038–1047 (2013).
Portugal, S. et al. Malaria-associated atypical memory B cells exhibit markedly reduced B cell receptor signaling and effector function. eLife 4, e07218 (2015).
Portugal, S., Pierce, S. K. & Crompton, P. D. Young lives lost as B cells falter: what we are learning about antibody responses in malaria. J. Immunol. 190, 3039–3046 (2013).
Chen, I. et al. “Asymptomatic” malaria: a chronic and debilitating infection that should be treated. PLoS Med. 13, e1001942 (2016).
Magrath, I. Epidemiology: clues to the pathogenesis of Burkitt lymphoma. Br. J. Haematol. 156, 744–756 (2012).
Thorley-Lawson, D., Deitsch, K. W., Duca, K. a. & Torgbor, C. The link between Plasmodium falciparum malaria and endemic Burkitt'slymphoma — new insight into a 50-year-old enigma. PLoS Pathog. 12, 12–16 (2016).
Torgbor, C. et al. A multifactorial role for P. falciparum malaria in endemic Burkitt's lymphoma pathogenesis. PLoS Pathog. 10, e1004170 (2014).
Robbiani, D. F. et al. Plasmodium infection promotes genomic instability and AID-dependent B cell lymphoma. Cell 162, 727–737 (2015). This study shows that murine Plasmodium infections can promote the development of mature B cell lymphoma by inducing AID expression in lymphoid tissues.
Lewis, C. P., Lavy, C. B. D. & Harrison, W. J. Delay in skeletal maturity in Malawian children. J. Bone Joint Surg. Br. 84, 732–734 (2002).
LaBeaud, A. D. et al. Parasitism in children aged three years and under: relationship between infection and growth in rural coastal Kenya. PLoS Negl. Trop. Dis. 9, e0003721 (2015).
Lee, M. S. J. et al. Plasmodium products persist in the bone marrow and promote chronic bone loss. Sci. Immunol. 2, eaam8093 (2017). This study shows experimentally for the first time that Plasmodium metabolic products, including haemozoin, cause chronic bone loss.
Liehl, P. & Mota, M. M. Innate recognition of malarial parasites by mammalian hosts. Int. J. Parasitol. 42, 557–566 (2012).
Gazzinelli, R. T., Kalantari, P., Fitzgerald, K. A. & Golenbock, D. T. Innate sensing of malaria parasites. Nat. Rev. Immunol. 14, 744–757 (2014).
Egan, E. S. et al. A forward genetic screen identifies erythrocyte CD55 as essential for Plasmodium falciparum invasion. Science 348, 711–714 (2015).
Zenonos, Z. A. et al. Basigin is a druggable target for host-oriented antimalarial interventions. J. Exp. Med. 212, 1145–1151 (2015).
Langhorne, J. & Duffy, P. E. Expanding the antimalarial toolkit: targeting host-parasite interactions. J. Exp. Med. 213, 143–153 (2016).
Sturm, A. et al. Manipulation of host hepatocytes by the malaria parasite for delivery into liver sinusoids. Science 313, 1287–1290 (2006).
Haldar, K. & Mohandas, N. Malaria, erythrocytic infection, and anemia. Hematology Am. Soc. Hematol. Educ. Program 2009, 87–93 (2009).
Miller, L. H., Ackerman, H. C., Su, X.-Z. & Wellems, T. E. Malaria biology and disease pathogenesis: insights for new treatments. Nat. Med. 19, 156–167 (2013).
Evans, K. J., Hansen, D. S., Van Rooijen, N., Buckingham, L. A. & Schofield, L. Severe malarial anemia of low parasite burden in rodent models results from accelerated clearance of uninfected erythrocytes. Blood 107, 1192–1199 (2006).
Lamikanra, A. A. et al. Malarial anemia: of mice and men. Blood 110, 18–28 (2007).
Lamb, T. J., Brown, D. E., Potocnik, A. J. & Langhorne, J. Insights into the immunopathogenesis of malaria using mouse models. Expert Rev. Mol. Med. 8, 1–22 (2006).
Collins, W. E., Jeffery, G. M. & Roberts, J. M. A retrospective examination of anemia during infection of humans with Plasmodium vivax. Am. J. Trop. Med. Hyg. 68, 410–412 (2003).
Jakeman, G. N., Saul, A., Hogarth, W. L. & Collins, W. E. Anaemia of acute malaria infections in non-immune patients primarily results from destruction of uninfected erythrocytes. Parasitology 119, 127–133 (1999).
White, N. J. Malaria parasite clearance. Malar. J. 16, 88 (2017).
Fernandez-Arias, C. et al. Anti-self phosphatidylserine antibodies recognize uninfected erythrocytes promoting malarial anemia. Cell Host Microbe 19, 194–203 (2016).
Sosale, N. G., Spinler, K. R., Alvey, C. & Discher, D. E. Macrophage engulfment of a cell or nanoparticle is regulated by unavoidable opsonization, a species-specific 'Marker of Self' CD47, and target physical properties. Curr. Opin. Immunol. 35, 107–112 (2015).
Segawa, K. & Nagata, S. An apoptotic 'eat me' signal: phosphatidylserine exposure. Trends Cell Biol. 25, 639–650 (2015).
Cunnington, A. J. A., de Souza, J. B., Walther, M. & Riley, E. E. M. Malaria impairs resistance to Salmonella through heme- and heme oxygenase–dependent dysfunctional granulocyte mobilization. Nat. Med. 18, 120–127 (2011).
Ferreira, A., Balla, J., Jeney, V., Balla, G. & Soares, M. P. A central role for free heme in the pathogenesis of severe malaria: the missing link? J. Mol. Med. 86, 1097–1111 (2008).
Zhao, H. et al. Lipocalin 2 bolsters innate and adaptive immune responses to blood-stage malaria infection by reinforcing host iron metabolism. Cell Host Microbe 12, 705–716 (2012).
Langhorne, J., Ndungu, F. M. M., Sponaas, A.-M. & Marsh, K. Immunity to malaria: more questions than answers. Nat. Immunol. 9, 725–732 (2008).
Riley, E. M. & Stewart, V. A. Immune mechanisms in malaria: new insights in vaccine development. Nat. Med. 19, 168–178 (2013).
Tiburcio, M., Sauerwein, R., Lavazec, C. & Alano, P. Erythrocyte remodeling by Plasmodium falciparum gametocytes in the human host interplay. Trends Parasitol. 31, 270–278 (2015).
Goel, S. et al. RIFINs are adhesins implicated in severe Plasmodium falciparum malaria. Nat. Med. 21, 314–317 (2015).
Franke-Fayard, B., Fonager, J., Braks, A., Khan, S. M. & Janse, C. J. Sequestration and tissue accumulation of human malaria parasites: can we learn anything from rodent models of malaria? PLoS Pathog. 6, e1001032 (2010).
Zhao, H. et al. Olfactory plays a key role in spatiotemporal pathogenesis of cerebral malaria. Cell Host Microbe 15, 551–563 (2014). This is the first study to show that the blood–brain barrier is disrupted at the olfactory bulb during experimental cerebral malaria.
Claser, C. et al. CD8+ T cells and IFN-γ mediate the time-dependent accumulation of infected red blood cells in deep organs during experimental cerebral malaria. PLoS ONE 6, e18720 (2011).
Rénia, L. & Howland, S. W. Targeting the olfactory bulb during experimental cerebral malaria. Trends Parasitol. 30, 375–376 (2014).
Fonager, J. et al. Reduced CD36-dependent tissue sequestration of Plasmodium-infected erythrocytes is detrimental to malaria parasite growth in vivo. J. Exp. Med. 209, 93–107 (2012).
Dorovini-Zis, K. et al. The neuropathology of fatal cerebral malaria in Malawian children. Am. J. Pathol. 178, 2146–2158 (2011).
Turner, L. et al. Severe malaria is associated with parasite binding to endothelial protein C receptor. Nature 498, 502–505 (2013).
Wassmer, S. C. et al. Investigating the pathogenesis of severe malaria: a multidisciplinary and cross-geographical approach. Am. J. Trop. Med. Hyg. 93, 42–56 (2015).
Lennartz, F. et al. Structure-guided identification of a family of dual receptor-binding PfEMP1 that is associated with cerebral malaria. Cell Host Microbe 21, 403–414 (2017).
Howland, S. W. et al. Brain microvessel cross-presentation is a hallmark of experimental cerebral malaria. EMBO Mol. Med. 5, 916–931 (2013).
Jambou, R. et al. Plasmodium falciparum adhesion on human brain microvascular endothelial cells involves transmigration-like cup formation and induces opening of intercellular junctions. PLoS Pathog. 6, e1001021 (2010).
Mantel, P. Y. & Marti, M. The role of extracellular vesicles in Plasmodium and other protozoan parasites. Cell. Microbiol. 16, 344–354 (2014).
Mantel, P. Y. et al. Malaria-infected erythrocyte-derived microvesicles mediate cellular communication within the parasite population and with the host immune system. Cell Host Microbe 13, 521–534 (2013).
van der Heyde, H. C., Nolan, J., Combes, V., Gramaglia, I. & Grau, G. E. A unified hypothesis for the genesis of cerebral malaria: sequestration, inflammation and hemostasis leading to microcirculatory dysfunction. Trends Parasitol. 22, 503–508 (2006).
Frevert, U. & Nacer, A. Immunobiology of Plasmodium in liver and brain. Parasite Immunol. 35, 267–282 (2013).
Owens, T., Bechmann, I. & Engelhardt, B. Perivascular spaces and the two steps to neuroinflammation. J. Neuropathol. Exp. Neurol. 67, 1113–1121 (2008).
Abbott, N. J., Patabendige, A. A. K., Dolman, D. E. M., Yusof, S. R. & Begley, D. J. Structure and function of the blood–brain barrier. Neurobiol. Dis. 37, 13–25 (2010).
Taylor, T. E. et al. Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat. Med. 10, 143–145 (2004).
Idro, R., Jenkins, N. E. & Newton, C. R. J. C. Pathogenesis, clinical features, and neurological outcome of cerebral malaria. Lancet Neurol. 4, 827–840 (2005).
Newton, C. R., Hien, T. T. & White, N. Cerebral malaria. J. Neurol. Neurosurg. Psychiatry 69, 433–441 (2000).
Seydel, K. B. et al. Brain swelling and death in children with cerebral malaria. N. Engl. J. Med. 372, 1126–1137 (2015). This study shows that death occurs in humans during cerebral malaria owing to brain swelling and oedema.
Penet, M. F. et al. Imaging experimental cerebral malaria in vivo: significant role of ischemic brain edema. J. Neurosci. 25, 7352–7358 (2005).
Medana, I. M., Hunt, N. H. & Chan-Ling, T. Early activation of microglia in the pathogenesis of fatal murine cerebral malaria. Glia 19, 91–103 (1997).
Coban, C. et al. Pathological role of Toll-like receptor signaling in cerebral malaria. Int. Immunol. 19, 67–79 (2007).
Hoffman, A. et al. Experimental cerebral malaria spreads along the rostral migratory stream. PLoS Pathog. 12, e1005470 (2016).
Shrivastava, S. K. et al. Uptake of parasite-derived vesicles by astrocytes and microglial phagocytosis of infected erythrocytes may drive neuroinflammation in cerebral malaria. Glia 65, 75–92 (2017).
Medana, I. M., Chan-Ling, T. & Hunt, N. H. Redistribution and degeneration of retinal astrocytes in experimental murine cerebral malaria: relationship to disruption of the blood-retinal barrier. Glia 16, 51–64 (1996).
Medana, I. M. et al. Axonal Injury in cerebral malaria. Am. J. Pathol. 160, 655–666 (2002).
Medana, I. M., Idro, R. & Newton, C. R. J. C. Axonal and astrocyte injury markers in the cerebrospinal fluid of Kenyan children with severe malaria. J. Neurol. Sci. 258, 93–98 (2007).
Aspelund, a. et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. J. Exp. Med. 212, 991–999 (2015).
Louveau, A. et al. Structural and functional features of central nervous system lymphatic vessels. Nature 523, 337–341 (2015). References 81 and 82 describe the presence of dural lymphatics.
Coureuil, M., Lécuyer, H., Bourdoulous, S. & Nassif, X. A journey into the brain: insight into how bacterial pathogens cross blood–brain barriers. Nat. Rev. Microbiol. 15, 149–159 (2017).
Zhao, Z., Nelson, A. R., Betsholtz, C. & Zlokovic, B. V. Establishment and dysfunction of the blood-brain barrier. Cell 163, 1064–1078 (2015).
Louveau, A., Harris, T. H. & Kipnis, J. Revisiting the mechanisms of CNS immune privilege. Trends Immunol. 36, 569–577 (2015).
Ransohoff, R. M. & Engelhardt, B. The anatomical and cellular basis of immune surveillance in the central nervous system. Nat. Rev. Immunol. 12, 623–635 (2012).
Iliff, J. J., Goldman, S. a. & Nedergaard, M. Implications of the discovery of brain lymphatic pathways. Lancet Neurol. 14, 977–979 (2015).
Iliff, J. J. et al. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J. Clin. Invest. 123, 1299–1309 (2013).
Ampawong, S. et al. Electron microscopic features of brain edema in rodent cerebral malaria in relation to glial fibrillary acidic protein expression. Int. J. Clin. Exp. Pathol. 7, 2056–2067 (2014).
Promeneur, D., Lunde, L. K., Amiry-Moghaddam, M. & Agre, P. Protective role of brain water channel AQP4 in murine cerebral malaria. Proc. Natl Acad. Sci. USA 110, 1035–1040 (2013).
Bartholomäus, I. et al. Effector T cell interactions with meningeal vascular structures in nascent autoimmune CNS lesions. Nature 462, 94–98 (2009).
Shaw, T. N. et al. Perivascular arrest of CD8+ T cells is a signature of experimental cerebral malaria. PLoS Pathog. 11, e1005210 (2015).
Lackner, P. et al. Scanning electron microscopy of the neuropathology of murine cerebral malaria. Malar. J. 5, 116 (2006).
Ampawong, S. et al. Quantitation of brain edema and localisation of aquaporin 4 expression in relation to susceptibility to experimental cerebral malaria. Int. J. Clin. Exp. Pathol. 4, 566–574 (2011).
Nacer, A. et al. Experimental cerebral malaria pathogenesis — hemodynamics at the blood brain barrier. PLoS Pathog. 10, e1004528 (2014).
Howland, S. W., Poh, C. M. & Rénia, L. Activated brain endothelial cells cross-present malaria antigen. PLoS Pathog. 11, e1004963 (2015).
Howland, S. W., Gun, S. Y., Claser, C., Poh, C. M. & Rénia, L. Measuring antigen presentation in mouse brain endothelial cells ex vivo and in vitro. Nat. Protoc. 10, 2016–2026 (2015).
Swanson, P. a. et al. CD8+ T cells induce fatal brainstem pathology during cerebral malaria via luminal antigen-specific engagement of brain vasculature. PLoS Pathog. 12, e1006022 (2016).
Combes, V., Guillemin, G. J., Chan-Ling, T., Hunt, N. H. & Grau, G. E. R. The crossroads of neuroinflammation in infectious diseases: endothelial cells and astrocytes. Trends Parasitol. 28, 311–319 (2012).
Greiner, J. et al. Correlation of hemorrhage, axonal damage, and blood-tissue barrier disruption in brain and retina of Malawian children with fatal cerebral malaria. Front. Cell. Infect. Microbiol. 5, 18 (2015).
Saeki, N. et al. Histologic characteristics of normal perivascular spaces along the optic tract: new pathogenetic mechanism for edema in tumors in the pituitary region. Am. J. Neuroradiol. 25, 1218–1222 (2004).
Kwee, R. M. & Kwee, T. C. Virchow–Robin spaces at MR imaging. Radiographics 27, 1071–1086 (2007).
Beare, N. A. V., Taylor, T. E., Harding, S. P., Lewallen, S. & Molyneux, M. E. Malarial retinopathy: a newly established diagnostic sign in severe malaria. Am. J. Trop. Med. Hyg. 75, 790–797 (2006). This is the first study to describe malarial retinopathy in human cerebral malaria.
Idro, R., Marsh, K., John, C. C. & Newton, C. R. J. Cerebral malaria: mechanisms of brain injury and strategies for improved neurocognitive outcome. Pediatr. Res. 68, 267–274 (2010).
Maude, R. J. et al. Magnetic resonance imaging of the brain in adults with severe falciparum malaria. Malar. J. 13, 177 (2014).
Grau, G. E. et al. Platelet accumulation in brain microvessels in fatal pediatric cerebral malaria. J. Infect. Dis. 187, 461–466 (2003).
White, V. A., Lewallen, S., Beare, N. A. V., Molyneux, M. E. & Taylor, T. E. Retinal pathology of pediatric cerebral malaria in Malawi. PLoS ONE 4, e4317 (2009).
Beare, N. A., Lewallen, S., Taylor, T. E. & Molyneux, M. E. Redefining cerebral malaria by including malaria retinopathy. Future Microbiol. 6, 349–355 (2011).
Maccormick, I. J. C. et al. Cerebral malaria in children: using the retina to study the brain. Brain 137, 2119–2142 (2014).
Barrera, V. et al. Severity of retinopathy parallels the degree of parasite sequestration in the eyes and brains of Malawian children with fatal cerebral malaria. J. Infect. Dis. 211, 1977–1986 (2015).
Vecino, E., Rodriguez, F. D., Ruzafa, N., Pereiro, X. & Sharma, S. C. Glia–neuron interactions in the mammalian retina. Prog. Retin. Eye Res. 51, 1–40 (2016).
Saggu, R., Faille, D., Grau, G. E., Cozzone, P. J. & Viola, A. In the eye of experimental cerebral malaria. Am. J. Pathol. 179, 1104–1109 (2011).
Danielyan, L. et al. Intranasal delivery of cells to the brain. Eur. J. Cell Biol. 88, 315–324 (2009).
Chaigneau, E. et al. Two-photon imaging of capillary blood flow in olfactory bulb glomeruli. Proc. Natl Acad. Sci. USA 100, 13081–13086 (2003).
Ueno, M. & Dobrogowska, D. H. & Vorbrodt, A. W. Immunocytochemical evaluation of the blood-brain barrier to endogenous albumin in the olfactory bulb and pons of senescence-accelerated mice (SAM). Histochem. Cell Biol. 105, 203–212 (1996).
Ioannidis, L. J., Nie, C. Q. & Hansen, D. S. The role of chemokines in severe malaria: more than meets the eye. Parasitology 141, 602–613 (2014).
Abkallo, H. M. et al. DNA from pre-erythrocytic stage malaria parasites is detectable by PCR in the faeces and blood of hosts. Int. J. Parasitol. 44, 467–473 (2014).
Taniguchi, T. et al. Plasmodium berghei ANKA causes intestinal malaria associated with dysbiosis. Sci. Rep. 5, 15699 (2015). This study shows that P. berghei parasites may promote gut pathology and dysbiosis of the intestinal microbiota.
Feasey, N. A., Dougan, G., Kingsley, R. A., Heyderman, R. S. & Gordon, M. A. Invasive non-typhoidal salmonella disease: an emerging and neglected tropical disease in Africa. Lancet 379, 2489–2499 (2012).
Chau, J. Y. et al. Malaria-associated L-arginine deficiency induces mast cell-associated disruption to intestinal barrier defenses against nontyphoidal salmonella bacteremia. Infect. Immun. 81, 3515–3526 (2013).
Adegnika, A. a & Kremsner, P. G. Epidemiology of malaria and helminth interaction: a review from 2001 to 2011. Curr. Opin. HIV AIDS 7, 221–224 (2012).
Potts, R. A. et al. Mast cells and histamine alter intestinal permeability during malaria parasite infection. Immunobiology 221, 468–474 (2015).
Mastelic, B. et al. IL-22 protects against liver pathology and lethality of an experimental blood-stage malaria infection. Front. Immunol. 3, 85 (2012).
Mooney, J. P. et al. The mucosal inflammatory response to non-typhoidal Salmonella in the intestine is blunted by IL-10 during concurrent malaria parasite infection. Mucosal Immunol. 7, 1302–1311 (2014).
Sellau, J., Alvarado, C., Hoenow, S. & Mackroth, M. IL-22 dampens the T cell response in experimental malaria. Sci. Rep. 6, 28058 (2016).
Yilmaz, B. et al. Gut microbiota elicits a protective immune response against malaria transmission. Cell 159, 1277–1289 (2014).
Villarino, N. F. et al. Composition of the gut microbiota modulates the severity of malaria. Proc. Natl Acad. Sci. USA 113, 2235–2240 (2016). This study shows that the gut microbiota modulates the severity of malaria.
Yooseph, S. et al. Stool microbiota composition is associated with the prospective risk of Plasmodium falciparum infection. BMC Genomics 16, 631 (2015).
Bernier-Latmani, J. et al. DLL4 promotes continuous adult intestinal lacteal regeneration and dietary fat transport. J. Clin. Invest. 125, 4572–4586 (2015).
Spadoni, I., Fornasa, G. & Rescigno, M. Organ-specific protection mediated by cooperation between vascular and epithelial barriers. Nat. Rev. Immunol. 17, 761–773 (2017).
Morrison, S. J. & Scadden, D. T. The bone marrow niche for haematopoietic stem cells. Nature 505, 327–334 (2014).
Imai, T. et al. Cytotoxic activities of CD8+ T cells collaborate with macrophages to protect against blood-stage murine malaria. eLife 2015, e04232 (2015).
Panichakul, T. et al. Production of erythropoietic cells in vitro for continuous culture of Plasmodium vivax. Int. J. Parasitol. 37, 1551–1557 (2007).
Tamez, P. A., Liu, H., Fernandez-Pol, S., Haldar, K. & Wickrema, A. Stage-specific susceptibility of human erythroblasts to Plasmodium falciparum malaria infection. Blood 114, 3652–3655 (2009).
Farfour, E., Charlotte, F., Settegrana, C., Miyara, M. & Buffet, P. The extravascular compartment of the bone marrow: a niche for Plasmodium falciparum gametocyte maturation? Malar. J. 11, 285 (2012).
Joice, R. et al. Plasmodium falciparum transmission stages accumulate in the human bone marrow. Sci. Transl Med. 6, 244re5 (2014).
Aguilar, R. et al. Molecular evidence for the localization of Plasmodium falciparum immature gametocytes in bone marrow. Blood 123, 959–966 (2014).
Chasis, J. A. & Mohandas, N. Erythroblastic islands: niches for erythropoiesis. Blood 112, 470–478 (2008).
Imai, T. et al. CD8+ T cell activation by murine erythroblasts infected with malaria parasites. Sci. Rep. 3, 1572 (2013).
Mercier, F. E., Ragu, C. & Scadden, D. T. The bone marrow at the crossroads of blood and immunity. Nat. Rev. Immunol. 12, 49–60 (2011).
Omatsu, Y. & Nagasawa, T. The critical and specific transcriptional regulator of the microenvironmental niche for hematopoietic stem and progenitor cells. Curr. Opin. Hematol. 22, 330–336 (2015).
Taylor, W. R. J., Hanson, J., Turner, G. D. H., White, N. J. & Dondorp, A. M. Respiratory manifestations of malaria. Chest 142, 492–505 (2012).
Ehrich, J. H. H. & Eke, F. U. Malaria-induced renal damage: facts and myths. Pediatr. Nephrol. 22, 626–637 (2007).
Brabin, B. J. et al. The sick placenta — the role of malaria. Placenta 25, 359–378 (2004).
Shechter, R., London, A. & Schwartz, M. Orchestrated leukocyte recruitment to immune-privileged sites: absolute barriers versus educational gates. Nat. Rev. Immunol. 13, 206–218 (2013).
Aspelund, A. et al. The Schlemm's canal is a VEGF-C/VEGFR-3-responsive lymphatic-like vessel. J. Clin. Invest. 124, 3975–3986 (2014).
Maitland, K. & Marsh, K. Pathophysiology of severe malaria in children. Acta Trop. 90, 131–140 (2004).
Wilairatana, P., Meddings, J. B., Ho, M., Vannaphan, S. & Looareesuwan, S. Increased gastrointestinal permeability in patients with Plasmodium falciparum malaria. Clin. Infect. Dis. 24, 430–435 (1997).
Romero, A. et al. Changes in gastric mucosa in acute malaria [Spanish]. Gen 47, 123–128 (1993).
Anstey, N. M., Douglas, N. M., Poespoprodjo, J. R. & Price, R. N. Plasmodium vivax: clinical spectrum, risk factors and pathogenesis. Adv. Parasitol. 80, 151–201 (2012).
Collins, W. E. & Jeffery, G. M. Plasmodium ovale: parasite and disease. Clin. Microbiol. Rev. 18, 570–581 (2005).
Strydom, K.-A., Ismail, F. & Frean, J. Plasmodium ovale: a case of not-so-benign tertian malaria. Malar. J. 13, 85 (2014).
Collins, W. E. & Jeffery, G. M. Plasmodium malariae: parasite and disease. Clin. Microbiol. Rev. 20, 579–592 (2007).
Singh, B. & Daneshvar, C. Human infections and detection of Plasmodium knowlesi. Clin. Microbiol. Rev. 26, 165–184 (2013).
Acknowledgements
The authors are supported by Grants-in-Aid for Scientific Research (B grant no. 16H05181 to C.C.) and by the Japan Agency for Medical Research and Development (AMED J-PRIDE 17fm0208021h0001 to C.C.).
Author information
Authors and Affiliations
Contributions
C.C. wrote the manuscript; all authors contributed to researching data, discussing the content and reviewing and editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Malaria
-
A disease caused by Plasmodium parasites belonging to the Apicomplexa phylum, which consists of several obligate intracellular parasites. The term was originally used in Italian folk medicine to mean poisonous or bad air.
- Activation-induced cytidine deaminase
-
(AID). An enzyme that is required for two crucial B cell events in the germinal centre: somatic hypermutation and class-switch recombination.
- Connective tissue
-
A connecting and supporting tissue composed of collagen and/or elastin fibres and interstitial fluid. Blood, bone and adipose tissue are some of the connective tissue components.
- Perivascular spaces
-
Also known as Virchow–Robin spaces. Spaces located between brain-penetrating pial vessels and the brain tissue grey matter.
- Interstitial fluid
-
(ISF). The solution present extracellularly, that fills the spaces between cells and tissues.
- Cerebrospinal fluid
-
(CSF). The solution surrounding the brain and spinal cord, which mainly serves to protect these two important organs.
- Olfactory bulb
-
An organ located on the cribriform plate, which functions in smell. The bulb surface is surrounded by complex olfactory nerve structures that originate from the nasal cavity and project to the brain. Small trabecular capillary structures are the main vessel structures inside the bulb.
- Cribriform plate
-
A small, perforated bone structure that lies on top of the nasal cavity and supports the olfactory bulb. Olfactory nerves running from the nasal cavity to the olfactory bulb pass thorough cribriform plate.
- Neurovascular coupling
-
A mechanism explaining the relationship between neuronal activity and the cerebral blood vessels and the blood flow.
- Lacteals
-
Small lymphatic capillaries located in the villi of the small intestine.
- Sinusoids
-
Vessels with a structure similar to capillaries but that have larger diameters and porous endothelial cells, which allow for permeability and exchange of materials; they are located in bone marrow, liver and spleen.
- Haemozoin
-
A unique by-product of Plasmodium parasites that accumulates in several organs, including spleen, liver and bone marrow, even after the infection resolves.
Rights and permissions
About this article
Cite this article
Coban, C., Lee, M. & Ishii, K. Tissue-specific immunopathology during malaria infection. Nat Rev Immunol 18, 266–278 (2018). https://doi.org/10.1038/nri.2017.138
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri.2017.138
This article is cited by
-
Genome-wide liver transcriptomic profiling of a malaria mouse model reveals disturbed immune and metabolic responses
Parasites & Vectors (2023)
-
Xylopic acid-amodiaquine and xylopic acid-artesunate combinations are effective in managing malaria in Plasmodium berghei-infected mice
Malaria Journal (2021)
-
Constitutive immune mechanisms: mediators of host defence and immune regulation
Nature Reviews Immunology (2021)
-
Immunoprofiles associated with controlled human malaria infection and naturally acquired immunity identify a shared IgA pre-erythrocytic immunoproteome
npj Vaccines (2021)
-
Multiplexed quantitative proteomics provides mechanistic cues for malaria severity and complexity
Communications Biology (2020)