Key Points
-
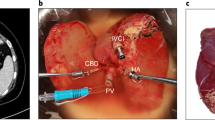
Successful organ yield depends on intrinsic donor characteristics as well as clinical interventions on the potential donor and the explanted liver
-
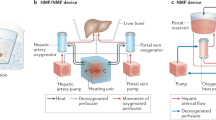
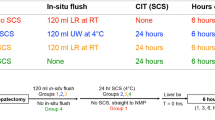
With low costs and simple technical and logistical requirements, static cold storage is still the standard method of preservation in liver transplantation, rather than machine perfusion
-
Dynamic storage systems for liver preservation have not yet realized their potential but might have tremendous consequences for transplant outcome and surgical routines
-
With restrictive donor selection, outcomes of split-liver transplantation can be comparable to full-size liver transplantation and help to expand the donor pool
Abstract
Liver transplantation is the best therapy in end-stage liver disease. Donor organ shortage and efforts to expand the donor organ pool are permanent issues given that advances in perioperative management and immunosuppressive therapy have brought the procedure into widespread clinical use. The management of organ procurement, including donor preconditioning and adequate organ storage, has a key role in transplantation. However, the organ procurement process can differ substantially between transplant centres, depending on local and national preferences. Advances in the field have come from experimental and clinical research on dynamic storage systems, such as machine perfusion devices, as an alternative to static cold storage. Determination of the clinical significance of these new systems is a topic worthy of future investigations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Monbaliu, D., Pirenne, J. & Talbot, D. Liver transplantation using donation after cardiac death donors. J. Hepatol. 56, 474–485 (2012).
Kluger, M. D., Memeo, R., Laurent, A., Tayar, C. & Cherqui, D. Survey of adult liver transplantation techniques (SALT): an international study of current practices in deceased donor liver transplantation. HPB (Oxford) 13, 692–698 (2011).
Starzl, T. E. et al. A flexible procedure for multiple cadaveric organ procurement. Surg. Gynecol. Obstet. 158, 223–230 (1984).
Starzl, T. E., Miller, C., Broznick, B. & Makowka, L. An improved technique for multiple organ harvesting. Surg. Gynecol. Obstet. 165, 343–348 (1987).
Wunderlich, H. et al. DTG procurement guidelines in heart beating donors. Transplant Int. 24, 733–757 (2011).
Casavilla, A. et al. Experience with liver and kidney allografts from non-heart-beating donors. Transplantation 59, 197–203 (1995).
Selck, F. W., Deb, P. & Grossman, E. B. Deceased organ donor characteristics and clinical interventions associated with organ yield. Am. J. Transplant. 8, 965–974 (2008).
Floerchinger, B., Oberhuber, R. & Tullius, S. G. Effects of brain death on organ quality and transplant outcome. Transplant. Rev. (Orlando) 26, 54–59 (2012).
Cittanova, M. L. et al. Effect of hydroxyethylstarch in brain-dead kidney donors on renal function in kidney-transplant recipients. Lancet 348, 1620–1622 (1996).
Christidis, C. et al. Worsening of hepatic dysfunction as a consequence of repeated hydroxyethylstarch infusions. J. Hepatol. 35, 726–732 (2001).
Shah, V. R. Aggressive management of multiorgan donor. Transplant. Proc. 40, 1087–1090 (2008).
Weiss, S. et al. Brain death activates donor organs and is associated with a worse I/R injury after liver transplantation. Am. J. Transplant. 7, 1584–1593 (2007).
Kotsch, K. et al. Methylprednisolone therapy in deceased donors reduces inflammation in the donor liver and improves outcome after liver transplantation: a prospective randomized controlled trial. Ann. Surg. 248, 1042–1050 (2008).
Wood, K. E., Becker, B. N., McCartney, J. G., D'Alessandro, A. M. & Coursin, D. B. Care of the potential organ donor. N. Engl. J. Med. 351, 2730–2739 (2004).
Macdonald, P. S. et al. A systematic review and meta-analysis of clinical trials of thyroid hormone administration to brain dead potential organ donors. Crit. Care Med. 40, 1635–1644 (2012).
D'Amico, F. et al. Use of N-acetylcysteine during liver procurement: a prospective randomized controlled study. Liver Transplant. 19, 135–144 (2013).
Azoulay, D. et al. Effects of 10 minutes of ischemic preconditioning of the cadaveric liver on the graft's preservation and function: the ying and the yang. Ann. Surg. 242, 133–139 (2005).
Koneru, B. et al. The ischemic preconditioning paradox in deceased donor liver transplantation—evidence from a prospective randomized single blind clinical trial. Am. J. Transplant. 7, 2788–2796 (2007).
Cescon, M. et al. Effect of ischemic preconditioning in whole liver transplantation from deceased donors. A pilot study. Liver Transplant. 12, 628–635 (2006).
Gurusamy, K. S., Kumar, Y., Sharma, D. & Davidson, B. R. Ischaemic preconditioning for liver transplantation. Cochrane Database of Systematic Reviews, Issue 1.Art. No.: CD006315 http://dx.doi.org/10.1002/14651858.CD006315.pub2.
Lehne, K. & Nobiling, R. Metabolic preconditioning with fructose prior to organ recovery attenuates ischemia–reperfusion injury in the isolated perfused rat liver. Scand. J. Gastroenterol. 48, 218–224 (2013).
Rao, J. et al. All-trans retinoic acid preconditioning protects against liver ischemia/reperfusion injury by inhibiting the nuclear factor κB signaling pathway. J. Surg. Res. 180, e99–e106 (2013).
Dulundu, E. et al. Alpha-lipoic acid protects against hepatic ischemia-reperfusion injury in rats. Pharmacology 79, 163–170 (2007).
Song, S. W., Guo, K. J., Shi, R., Cheng, Y. & Liu, Y. F. Pretreatment with calcitonin gene-related peptide attenuates hepatic ischemia/reperfusion injury in rats. Transplant. Proc. 41, 1493–1498 (2009).
Batkai, S. et al. Cannabinoid-2 receptor mediates protection against hepatic ischemia/reperfusion injury. FASEB J. 21, 1788–1800 (2007).
Wu, Q. et al. Diazoxide suppresses hepatic ischemia/reperfusion injury after mouse liver transplantation by a BCL-2-dependent mechanism. J. Surg. Res. 169, e155–e166 (2011).
Schmeding, M., Neumann, U. P., Boas-Knoop, S., Spinelli, A. & Neuhaus, P. Erythropoietin reduces ischemia-reperfusion injury in the rat liver. Eur. Surg. Res. 39, 189–197 (2007).
Bruns, H. et al. Glycine and taurine equally prevent fatty livers from Kupffer cell-dependent injury: an in vivo microscopy study. Microcirculation 18, 205–213 (2011).
Moussavian, M. R. et al. Multidrug donor preconditioning prevents cold liver preservation and reperfusion injury. Langenbecks Arch. Surg. 396, 231–241 (2011).
Zaouali, M. A. et al. Melatonin protects steatotic and nonsteatotic liver grafts against cold ischemia and reperfusion injury. J. Pineal. Res. 50, 213–221 (2011).
von Heesen, M. et al. Multidrug donor preconditioning protects steatotic liver grafts against ischemia–reperfusion injury. Am. J. Surg. 203, 168–176 (2012).
Donckier, V. et al. Preconditioning of donors with interleukin-10 reduces hepatic ischemia–reperfusion injury after liver transplantation in pigs. Transplantation 75, 902–904 (2003).
Izuishi, K. et al. Cutting edge: high-mobility group Box 1 preconditioning protects against liver ischemia–reperfusion injury. J. Immunol. 176, 7154–7158 (2006).
Net, M. et al. Hepatic preconditioning after prolonged warm ischemia by means of S-adenosyl-L-methionine administration in pig liver transplantation from non-heart-beating donors. Transplantation 75, 1970–1977 (2003).
Scherer de Fraga, R. et al. S-nitroso-N-acetylcysteine: a promising drug for early ischemia/reperfusion injury in rat liver. Transplant. Proc. 42, 4491–4495 (2010).
Huser, N. et al. Graft preconditioning with low-dose tacrolimus (FK506) and nitric oxide inhibitor aminoguanidine (AGH) reduces ischemia/reperfusion injury after liver transplantation in the rat. Arch. Pharm. Res. 32, 215–220 (2009).
Pratschke, S. et al. Tacrolimus preconditioning of rat liver allografts impacts glutathione homeostasis and early reperfusion injury. J. Surg. Res. 176, 309–316 (2012).
Pratschke, S. et al. Protocol TOP-Study (tacrolimus organ perfusion): a prospective randomized multicenter trial to reduce ischemia reperfusion injury in transplantation of marginal liver grafts with an ex vivo tacrolimus perfusion. Transplant. Res. 2, 3 (2013).
Ozaki, M., Ozasa, H., Fuchinoue, S., Teraoka, S. & Ota, K. Protective effects of glycine and esterified gamma-glutamylcysteine on ischemia/reoxygenation injury of rat liver. Transplantation 58, 753–755 (1994).
Bachmann, S., Peng, X. X., Currin, R. T., Thurman, R. G. & Lemasters, J. J. Glycine in Carolina rinse solution reduces reperfusion injury, improves graft function, and increases graft survival after rat liver transplantation. Transplant. Proc. 27, 741–742 (1995).
Schemmer, P. et al. Extended experience with glycine for prevention of reperfusion injury after human liver transplantation. Transplant. Proc. 34, 2307–2309 (2002).
Luntz, S. P. et al. HEGPOL: randomized, placebo controlled, multicenter, double-blind clinical trial to investigate hepatoprotective effects of glycine in the postoperative phase of liver transplantation [ISRCTN69350312]. BMC Surg. 5, 18 (2005).
von Frankenberg, M. et al. Donor pretreatment with gadolinium chloride improves early graft function and survival after porcine liver transplantation. Transplant. Int. 16, 806–813 (2003).
Pirenne, J. et al. Biliary strictures after liver transplantation: risk factors and prevention by donor treatment with epoprostenol. Transplant. Proc. 41, 3399–3402 (2009).
Farkas, S. et al. Conditioning of liver grafts with prostaglandins improves bile acid transport. Transplant. Proc. 37, 435–438 (2005).
Nagrath, D. et al. Metabolic preconditioning of donor organs: defatting fatty livers by normothermic perfusion ex vivo. Metab. Eng. 11, 274–283 (2009).
Wang, C. F. et al. Preconditioning donor liver with Nodosin perfusion lessens rat ischemia reperfusion injury via heme oxygenase-1 upregulation. J. Gastroenterol. Hepatol. 27, 832–840 (2012).
Sano, T. et al. Hepatic preconditioning using lipopolysaccharide: association with specific negative regulators of the Toll-like receptor 4 signaling pathway. Transplantation 91, 1082–1089 (2011).
Kong, R. et al. The strategy of combined ischemia preconditioning and salvianolic acid-B pretreatment to prevent hepatic ischemia-reperfusion injury in rats. Dig. Dis. Sci. 54, 2568–2576 (2009).
Sehirli, O. et al. Grape seed extract treatment reduces hepatic ischemia-reperfusion injury in rats. Phytother. Res. 22, 43–48 (2008).
Sener, G. et al. Aqueous garlic extract alleviates ischaemia–reperfusion-induced oxidative hepatic injury in rats. J. Pharm. Pharmacol. 57, 145–150 (2005).
Beck-Schimmer, B. et al. A randomized controlled trial on pharmacological preconditioning in liver surgery using a volatile anesthetic. Ann. Surg. 248, 909–918 (2008).
Minou, A. F., Dzyadzko, A. M., Shcherba, A. E. & Rummo, O. O. The influence of pharmacological preconditioning with sevoflurane on incidence of early allograft dysfunction in liver transplant recipients. Anesthesiol. Res. Pract. 2012, 930487 (2012).
Bedirli, N. et al. Hepatic energy metabolism and the differential protective effects of sevoflurane and isoflurane anesthesia in a rat hepatic ischemia–reperfusion injury model. Anesth. Analg. 106, 830–837 (2008).
Kang, K. et al. Role of hydrogen sulfide in hepatic ischemia-reperfusion-induced injury in rats. Liver Transplant. 15, 1306–1314 (2009).
Canelo, R., Hakim, N. S. & Ringe, B. Experience with hystidine tryptophan ketoglutarate versus University Wisconsin preservation solutions in transplantation. Int. Surg. 88, 145–151 (2003).
Erhard, J. et al. Comparison of histidine-tryptophan-ketoglutarate (HTK) solution versus University of Wisconsin (UW) solution for organ preservation in human liver transplantation. A prospective, randomized study. Transplant. Int. 7, 177–181 (1994).
Chan, S. C., Liu, C. L., Lo, C. M. & Fan, S. T. Applicability of histidine-tryptophan-ketoglutarate solution in right lobe adult-to-adult live donor liver transplantation. Liver Transplant. 10, 1415–1421 (2004).
Welling, T. H. et al. Biliary complications following liver transplantation in the model for end-stage liver disease era: effect of donor, recipient, and technical factors. Liver Transplant. 14, 73–80 (2008).
Mangus, R. S. et al. Comparison of histidine-tryptophan-ketoglutarate solution and University of Wisconsin solution in extended criteria liver donors. Liver Transplant. 14, 365–373 (2008).
Moench, C. & Otto, G. Ischemic type biliary lesions in histidine-tryptophan-ketoglutarate (HTK) preserved liver grafts. Int. J. Artif. Organs 29, 329–334 (2006).
Stewart, Z. A., Cameron, A. M., Singer, A. L., Montgomery, R. A. & Segev, D. L. Histidine-Tryptophan-Ketoglutarate (HTK) is associated with reduced graft survival in deceased donor livers, especially those donated after cardiac death. Am. J. Transplant. 9, 286–293 (2009).
Mangus, R. S. et al. Comparison of histidine-tryptophan-ketoglutarate solution (HTK) and University of Wisconsin solution (UW) in adult liver transplantation. Liver Transplant. 12, 226–230 (2006).
Testa, G. et al. Histidine-tryptophan-ketoglutarate versus University of Wisconsin solution in living≈donor liver transplantation: results of a prospective study. Liver Transplant. 9, 822–826 (2003).
Belzer, F. O., Ashby, B. S., Gulyassy, P. F. & Powell, M. Successful seventeen-hour preservation and transplantation of human-cadaver kidney. N. Engl. J. Med. 278, 608–610 (1968).
Belzer, F. O., May, R., Berry, M. N. & Lee, J. C. Short term preservation of porcine livers. J. Surg. Res. 10, 55–61 (1970).
Lindbergh, C. A., Perry, V. P., Malinin, T. I. & Mouer, G. H. An apparatus for the pulsating perfusion of whole organs. Cryobiology 3, 252–260 (1966).
Slapak, M., Wigmore, R. A. & MacLean, L. D. Twenty-four hour liver preservation by the use of continuous pulsatile perfusion and hyperbaric oxygen. Transplantation 5 (Suppl.), 1154–1158 (1967).
Starzl, T. E. et al. Extended survival in 3 cases of orthotopic homotransplantation of the human liver. Surgery 63, 549–563 (1968).
Brockmann, J. et al. Normothermic perfusion: a new paradigm for organ preservation. Ann. Surg. 250, 1–6 (2009).
Guarrera, J. V. et al. Hypothermic machine preservation in human liver transplantation: the first clinical series. Am. J. Transplant. 10, 372–381 (2010).
Berendsen, T. A. et al. A simplified subnormothermic machine perfusion system restores ischemically damaged liver grafts in a rat model of orthotopic liver transplantation. Transplant. Res. 1, 6 (2012).
Dutkowski, P., Graf, R. & Clavien, P. A. Rescue of the cold preserved rat liver by hypothermic oxygenated machine perfusion. Am. J. Transplant. 6, 903–912 (2006).
Monbaliu, D. & Brassil, J. Machine perfusion of the liver: past, present and future. Curr. Opin. Organ Transplant. 15, 160–166 (2010).
Fondevila, C. et al. Superior preservation of DCD livers with continuous normothermic perfusion. Ann. Surg. 254, 1000–1007 (2011).
Fondevila, C. et al. Liver transplant using donors after unexpected cardiac death: novel preservation protocol and acceptance criteria. Am. J. Transplant. 7, 1849–1855 (2007).
Moers, C. et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N. Engl. J. Med. 360, 7–19 (2009).
Opelz, G. & Dohler, B. Multicenter analysis of kidney preservation. Transplantation 83, 247–253 (2007).
Dutkowski, P. et al. First results on end-ischemic hypothermic oxygenated machine perfusion (HOPE) of human liver grafts donated after cardiac arrest [abstract #O-75]. Liver Transplant. 19 (Suppl. 1), S31 (2013).
Dutkowski, P., Furrer, K., Tian, Y., Graf, R. & Clavien, P. A. Novel short-term hypothermic oxygenated perfusion (HOPE) system prevents injury in rat liver graft from non-heart beating donor. Ann. Surg. 244, 968–976 (2006).
Minor, T., Akbar, S., Tolba, R. & Dombrowski, F. Cold preservation of fatty liver grafts: prevention of functional and ultrastructural impairments by venous oxygen persufflation. J. Hepatol. 32, 105–111 (2000).
Minor, T., Saad, S., Kotting, M., Nagelschmidt, M. & Paul, A. Endischemic oxygen persufflation to improve viability of marginally preserved donor livers. Transplant. Int. 11 (Suppl. 1), S400–S403 (1998).
Suszynski, T. M. et al. Persufflation (or gaseous oxygen perfusion) as a method of organ preservation. Cryobiology 64, 125–143 (2012).
Minor, T. et al. Oxygen persufflation as adjunct in liver preservation (OPAL): study protocol for a randomized controlled trial. Trials 12, 234 (2011).
Butler, A. J. et al. Successful extracorporeal porcine liver perfusion for 72 hr. Transplantation 73, 1212–1218 (2002).
Op den Dries, S. et al. Successful ex-vivo normothermic machine perfusion and viability testing of discarded human donor livers [abstract #O-91]. Liver Transplant. 19 (Suppl. 1), S34 (2013).
Liu, Q. et al. Release of AST and LFABP from ischemically damaged livers during machine perfusion: a new tool to predict viability and primary non-function. Transplant. Int. 22, 55 (2009).
van der Plaats, A. et al. The Groningen hypothermic liver perfusion pump: functional evaluation of a new machine perfusion system. Ann. Biomed. Eng. 34, 1924–1934 (2006).
Liu, Q. et al. Discriminate liver warm ischemic injury during hypothermic machine perfusion by proton magnetic resonance spectroscopy: a study in a porcine model. Transplant. Proc. 41, 3383–3386 (2009).
St Peter, S. D. et al. Beta-galactosidase as a marker of ischemic injury and a mechanism for viability assessment in porcine liver transplantation. Liver Transplant. 8, 21–26 (2002).
Chouker, A. et al. Alpha-gluthathione S-transferase as an early marker of hepatic ischemia/reperfusion injury after liver resection. World J. Surg. 29, 528–534 (2005).
Itasaka, H. et al. Significance of hyaluronic acid for evaluation of hepatic endothelial cell damage after cold preservation/reperfusion. J. Surg. Res. 59, 589–595 (1995).
Golling, M. et al. Reduced glutathione in the liver as a potential viability marker in non-heart-beating donors. Liver Transplant. 14, 1637–1647 (2008).
Habib, M. M. et al. A comparison of bile composition from heart-beating and non-heart-beating rabbit organ donors during normothermic extracorporeal liver perfusion: experimental evaluation using proton magnetic resonance spectroscopy. Transplant. Proc. 36, 2914–2916 (2004).
Lam, C. M., Fan, S. T., Lo, C. M. & Wong, J. Major hepatectomy for hepatocellular carcinoma in patients with an unsatisfactory indocyanine green clearance test. Br. J. Surg. 86, 1012–1017 (1999).
Stockmann, M. et al. The LiMAx test: a new liver function test for predicting postoperative outcome in liver surgery. HPB (Oxford) 12, 139–146 (2010).
Obara, H. et al. Pretransplant screening and evaluation of liver graft viability using machine perfusion preservation in porcine transplantation. Transplant. Proc. 44, 959–961 (2012).
Hara, Y. et al. In vivo effect of bone marrow-derived mesenchymal stem cells in a rat kidney transplantation model with prolonged cold ischemia. Transplant. Int. 24, 1112–1123 (2011).
Pan, G. Z. et al. Bone marrow mesenchymal stem cells ameliorate hepatic ischemia/reperfusion injuries via inactivation of the MEK/ERK signaling pathway in rats. J. Surg. Res. 178, 935–948 (2012).
Popp, F. C. et al. Safety and feasibility of third-party multipotent adult progenitor cells for immunomodulation therapy after liver transplantation—a phase I study (MISOT-I). J. Transl. Med. 9, 124 (2011).
Bessems, M. et al. Preservation of steatotic livers: a comparison between cold storage and machine perfusion preservation. Liver Transplant. 13, 497–504 (2007).
Lu, S., Yu, Y., Gao, Y., Li, G. Q. & Wang, X. H. Immunological inhibition of transplanted liver allografts by adeno-associated virus vector encoding CTLA4Ig in rats. Hepatobiliary Pancreat. Dis. Int. 7, 258–263 (2008).
Arav, A. & Natan, Y. Directional freezing: a solution to the methodological challenges to preserve large organs. Semin. Reprod. Med. 27, 438–442 (2009).
Gavish, Z., Ben-Haim, M. & Arav, A. Cryopreservation of whole murine and porcine livers. Rejuvenation Res. 11, 765–772 (2008).
Arav, A. et al. Oocyte recovery, embryo development and ovarian function after cryopreservation and transplantation of whole sheep ovary. Hum. Reprod. 20, 3554–3559 (2005).
Fahy, G. M. et al. Physical and biological aspects of renal vitrification. Organogenesis 5, 167–175 (2009).
Bismuth, H. & Houssin, D. Reduced-sized orthotopic liver graft in hepatic transplantation in children. Surgery 95, 367–370 (1984).
Bismuth, H. et al. Emergency orthotopic liver transplantation in two patients using one donor liver. Br. J. Surg. 76, 722–724 (1989).
Pichlmayr, R., Ringe, B., Gubernatis, G., Hauss, J. & Bunzendahl, H. Transplantation of a donor liver to 2 recipients (splitting transplantation)—a new method in the further development of segmental liver transplantation [German]. Langenbecks Arch. Chir. 373, 127–130 (1988).
Azoulay, D. et al. Split-liver transplantation. The Paul Brousse policy. Ann. Surg. 224, 737–746 (1996).
Adam, R. et al. Split liver transplantation in Europe: a European Liver Transplant Registry (ELTR) study on evolution and outcomes [abstract #O-142]. Liver Transplant. 19 (Suppl. 1), S40 (2013).
Cauley, R. P. et al. Deceased-donor split-liver transplantation in adult recipients: is the learning curve over? J. Am. Coll. Surg. 217, 672–684 (2013).
Doyle, M. B. et al. Outcomes with split liver transplantation are equivalent to those with whole organ transplantation. J. Am. Coll. Surg. 217, 102–112 (2013).
Lee, W.-C. et al. Feasibility of split liver transplantation for 2 adults in the model of end-stage liver disease era. Ann. Surg. 258, 306–311 (2013).
Azoulay, D. et al. Split-liver transplantation for two adult recipients: feasibility and long-term outcomes. Ann. Surg. 233, 565–574 (2001).
Zambelli, M. et al. Full-right-full-left split liver transplantation: the retrospective analysis of an early multicenter experience including graft sharing. Am J Transplant. 12, 2198–2210 (2012).
Broering, D. C. et al. Technical refinements and results in full-right full-left splitting of the deceased donor liver. Ann. Surg. 242, 802–812 (2005).
Lee, W. C. et al. Split liver transplantation in adults: preoperative estimation of the weight of right and left hemiliver grafts. Liver Transplant. 17, 93–94 (2011).
Fan, S. T., Lo, C. M., Liu, C. L., Yong, B. H. & Chan, J. K. Split liver transplantation for two adult recipients. Hepatogastroenterology 50, 231–234 (2003).
Doyle, M. B. M. et al. Outcomes with split liver transplantation are equivalent to those with whole organ transplantation. J. Am. Coll. Surg. 217, 102–112 (2013).
Little, D. M., Farrell, J. G., Cunningham, P. M. & Hickey, D. P. Donor sepsis is not a contraindication to cadaveric organ donation. QJM 90, 641–642 (1997).
Lumbreras, C. et al. Clinical significance of donor-unrecognized bacteremia in the outcome of solid-organ transplant recipients. Clin. Infect. Dis. 33, 722–726 (2001).
Freeman, R. B. et al. Outcome of transplantation of organs procured from bacteremic donors. Transplantation 68, 1107–1111 (1999).
Goldberg, E., Bishara, J., Lev, S., Singer, P. & Cohen, J. Organ transplantation from a donor colonized with a multidrug-resistant organism: a case report. Transplant Infect. Dis. 14, 296–299 (2012).
Ariza-Heredia, E. J. et al. Outcomes of transplantation using organs from a donor infected with Klebsiella pneumoniae carbapenemase (KPC)-producing K. pneumoniae. Transplant Infect. Dis. 14, 229–236 (2012).
Geenen, I. L. et al. Usage and outcomes of deceased donor liver allografts with preprocurement injury from blunt trauma. Liver Transplant. 15, 321–325 (2009).
Mehrabi, A. et al. Transplantation of a severely lacerated liver—a case report with review of the literature. Clin. Transplant. 23, 321–328 (2009).
Tucker, O. N., Girlanda, R., Rela, M., Heaton, N. D. & Muiesan, P. Successful outcome following transplantation of an injured liver from a nonheart beating donor. Transplant. Int. 18, 724–726 (2005).
Avolio, A. W. et al. Successful transplantation of an injured liver. Transplant. Proc. 32, 131–133 (2000).
Di Benedetto, F. et al. Successful liver transplantation using a severely injured graft. J. Trauma 63, 217–220 (2007).
World Medical Association. The World Medical Association Resolution on Euthanasia. World Medical Association [online], (2013).
Ysebaert, D. et al. Organ procurement after euthanasia: Belgian experience. Transplant. Proc. 41, 585–586 (2009).
Detry, O. et al. Organ donation after physician-assisted death. Transplant. Int. 21, 915 (2008).
Opelz, G. & Terasaki, P. I. Advantage of cold storage over machine perfusion for preservation of cadaver kidneys. Transplantation 33, 64–68 (1982).
Moers, C., Pirenne, J., Paul, A. & Ploeg, R. J. Machine perfusion or cold storage in deceased-donor kidney transplantation. N. Engl. J. Med. 366, 770–771 (2012).
Watson, C. J. et al. Cold machine perfusion versus static cold storage of kidneys donated after cardiac death: a UK multicenter randomized controlled trial. Am. J. Transplant. 10, 1991–1999 (2010).
Bond, M. et al. The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model. Health Technol. Assess 13, 1–156 (2009).
Author information
Authors and Affiliations
Contributions
M.N. and A.P. contributed to all aspects of this manuscript. P.N. reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Nebrig, M., Neuhaus, P. & Pascher, A. Advances in the management of the explanted donor liver. Nat Rev Gastroenterol Hepatol 11, 489–496 (2014). https://doi.org/10.1038/nrgastro.2014.58
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2014.58
This article is cited by
-
Machine perfusion of the liver: applications in transplantation and beyond
Nature Reviews Gastroenterology & Hepatology (2022)
-
Evaluation of the ex vivo liver viability using a nuclear magnetic resonance relaxation time-based assay in a porcine machine perfusion model
Scientific Reports (2021)
-
Normothermic Machine Preservation of the Liver: State of the Art
Current Transplantation Reports (2018)