Abstract
Some recently introduced vaccines that have excellent efficacy records have been developed without a clear understanding of their mechanism of protection. In fact, successful vaccines have often emerged out of empirical observations and have only rarely been the result of a rational use of the continuously increasing immunological knowledge available to scientists. However, a posteriori deciphering of the biological bases for the efficacy of successful vaccines should be an essential component of research efforts directed at the development of new vaccines for the most challenging infectious diseases.
Similar content being viewed by others
Main
In this review, we make an attempt to 'rediscover' some of the successful vaccines. Would the approaches in vaccine research and development that are presently used have allowed the discovery of some of the most efficient vaccines that are now routinely applied in public health? The early protection conferred by most existing vaccines is primarily based on antibody-dependent mechanisms, and the quality of these responses, including antibody avidity, is a determining factor of efficacy. The duration of protection relies largely on B-cell memory responses, although the persistence of antibody production is often crucial for combating rapidly invasive infections. T-cell responses to existing vaccines are undoubtedly of importance but they have not been extensively analyzed. Antigenic variation and strain diversity are complicating factors that have so far been addressed in a case-by-case manner. Finally, we consider the vaccinees, challenging the postulate that a successful adult vaccine may be used with equal success in an infant or an aging population. Consideration of these issues may help to tackle the challenges posed by those infectious targets that have thus far escaped successful vaccine-mediated opposition.
Selection of vaccine type: convenience or efficacy?
One of the earliest demonstrations of the ability of antibodies to protect against viral disease involved the administration of human immunoglobulin and the observation that most individuals were protected from measles if treated within 6 d of exposure1. Measurement of antibodies induced by immunization has often been used as a gauge of vaccine efficacy, and antibody-mediated protection is an essential component of existing vaccines that are directed against toxins, encapsulated bacteria and many viruses. Lack of immunity has been observed in individuals with immunoglobulin deficiencies. The importance of antibody-mediated mechanisms is also supported by the protection conferred by the materno-fetal transfer of antibody2 and is unequivocally demonstrated by the protective immunity conferred by passive administration of vaccine-induced antibodies (Table 1).
However, the ability of a vaccine antigen to generate protection is a complex challenge that goes beyond the antibody response itself. For viruses that exist in multiple strains or have the ability to mutate under immunologic pressure, either the antibodies must be targeted against a conserved epitope shared between strains and unlikely to mutate, or the vaccine must include antigens from each relevant strain. In addition, immunologic memory must be generated such that upon subsequent exposure to the pathogen, adequate specific antibodies will be rapidly generated and localized to the site of the pathogen. Although the earliest vaccines were based on infecting patients with either related or attenuated strains of a pathogen, later the use of inactivated viruses or viral subunits was developed as a means to increase the potential (or real) safety for certain pathogens or to ameliorate various manufacturing problems.
The two types of poliomyelitis vaccines illustrate some of these issues. Although the inactivated (and thus injected) polio vaccine (IPV) was the first to be developed, the oral polio vaccine (OPV) was pursued because it was presumed to confer the advantage of intestinal immunity from natural infection (as compared to just protection from the paralysis, the clinical disease) and longer-lasting protection. Although serum antibody induced by IPV can suppress pharyngeal viral excretion (which is thought to be the source of transmission in countries with high levels of hygiene), it is less effective at preventing intestinal infection3. A live attenuated vaccine administered by the route of natural infection would potentially protect against exposure to wild-type virus, and thereby decrease intestinal excretion, disrupt person-to-person transmission and, by extension, reduce epidemic spread4. It was also hoped that it could extend benefits through the spread of the vaccine virus to unvaccinated individuals (immunizing them).
Thus one cannot simply compare the level of serum antibodies induced by the inactivated and live polio vaccines (which are as good as or better for IPV than for OPV) and derive conclusions about superior worth. Also of import is the extremely small risk (about one per million doses administered4) of OPV-associated paralytic polio. Another issue, particularly in developing countries, is that infection with other enteroviruses or diarrhea at the time the vaccine is administered may interfere with its ability to attach to or infect the mucosa. These concerns explain why OPV was considered the most appropriate vaccine to use for the elimination of polio on a global basis, whereas moving from OPV to IPV seemed a logical decision in geographic areas where the risk of OPV-associated paralysis became higher than the risk of naturally occurring disease.
The process involved in the choice of vaccine type is equally illustrated by the measles vaccines. The attenuated live measles vaccine (Edmonston strain) that was approved in the early 1960s was used for over a decade despite causing a high incidence (20–40%) of fever unless immunoglobulin was concomitantly administered (reviewed in ref. 5). An inactivated vaccine derived from the Edmonston strain was also used in conjunction with a live vaccine (two doses of inactivated followed by one of the live strain). Although this latter regimen avoided the side effects of the live vaccine series, it also was less effective. Recipients not only had immunity of shorter duration but were at risk for atypical measles infection6. Notably, whereas the live vaccine induces cell-mediated immunity, the inactivated vaccine does not. Thus, live and inactivated viruses can induce immunity of different duration, as well as different types of immune response that may affect vaccine efficacy.
Influenza vaccines also exist in inactivated forms or as live attenuated virus. The inactivated vaccine can be reduced to just the hemagglutinin and neuraminidase proteins, against which the protective antibodies are directed (reviewed in ref. 7), in order to decrease the non-specific inflammatory effects of the vaccine. Antibodies directed against hemagglutinin, in particular, have been shown to be of predominant importance in protection, and serum hemagglutination–inhibiting titers are considered the best correlate of protection. Antibodies are strain specific, however, in contrast to T-cell responses, which are often cross-reactive between influenza subtypes. It is clear that other immune responses (in particular T-cell responses against conserved antigens) are important in influenza immunity and are induced suboptimally by the inactivated vaccines (reviewed in refs. 8,9). These observations spurred long-term efforts to develop a live attenuated influenza vaccine that could both provide broader protection than the inactivated vaccines and eliminate the need for an injection. The recently licensed cold-adapted influenza virus vaccine is administered by intranasal aerosol, and was adapted to grow at cooler temperatures (25 °C), thus reducing its ability to grow at normal body temperature. It proved effective at protecting adults from influenza after a single dose even though the serum hemagglutination–inhibiting antibody response was moderate10. The cold-adapted vaccine induces nasal IgA antibodies, but also T-cell responses and interferon, which may have a role in protection11. These responses, in addition to their longer persistence, may account for the observed ability of cold-adapted influenza vaccines to protect even against strains of influenza that have drifted antigenically (reviewed in ref. 8).
The known ability of both wild-type influenza infection and the cold-adapted vaccine to induce broader heterosubtypic immunity, by inducing not only antibodies but cellular immune response, provides additional rationale for the development of new types of vaccines that promote both responses simultaneously.
Importance of affinity maturation for induced protection
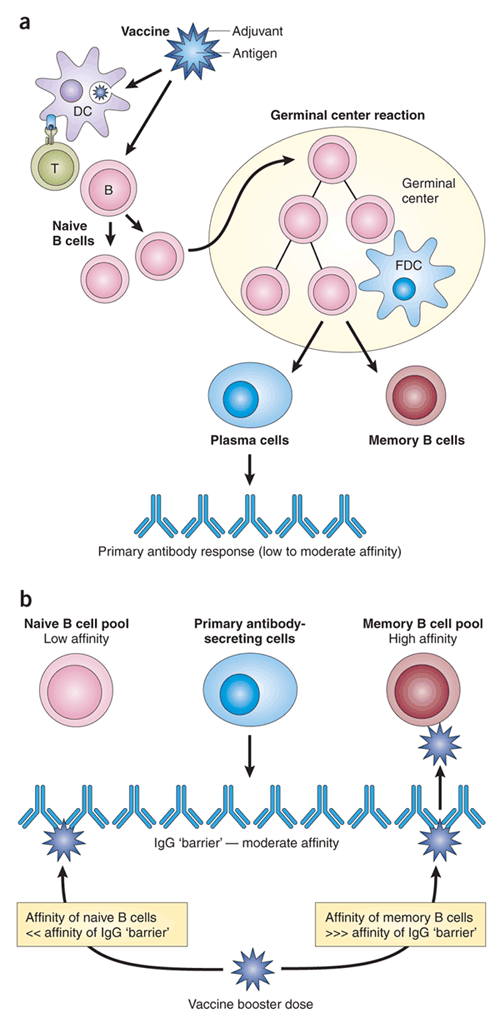
Antigen-specific serum IgG antibodies are produced by B lymphocytes that have differentiated into antibody-producing plasma cells. B-cell activation is initiated in secondary lymphoid organs (lymph nodes, spleen, Peyer patches, mucosal-associated lymphoid tissues) by antigen-presenting cells (mostly dendritic cells), in a CD4+ T cell–dependent (for protein antigens) or –independent (for most polysaccharide antigens) manner. Upon appropriate co-stimulation, activated B cells undergo a massive clonal proliferation generating secondary follicles called germinal centers (Fig. 1a). In these structures, the hypermutation of B-cell immunoglobulin genes results in the diversification of their B-cell receptor and thus the B cells' differentiation into subgroups with either lower or higher affinity for the activating antigen. Affinity-based selection rescues some B cells from apoptosis and triggers their differentiation into memory B cells or short-lived plasma cells secreting immunoglobulins with enhanced antigen-specific affinity12,13.
(a) Vaccine-induced primary B-cell responses usually encompass initial stages of B-cell recognition, antigen presentation and T-cell help, possibly enhanced by co-stimulatory signals provided by vaccine adjuvant or by vaccine-contained microbial products. A germinal center reaction follows, involving follicular dendritic cells (FDC), which allows for the proliferation and selection of B cells of increasing affinity for vaccine antigen epitopes. The final output is the production of antibody-secreting cells and memory B cells. Antibodies produced at this initial stage are usually of modest affinity despite a progressive accumulation of high-affinity memory B cells. (b) At time of boosting with a homologous antigen, high-affinity memory B cells are recruited even in presence of persisting antibodies, and compete for antigen with low-affinity naive B cells. The final result is the production of antibodies of higher affinity.
Sustained antibody-mediated protection is conferred by immune memory, which is mediated by long-lived IgG plasma cells and memory B cells12,14. Immunological memory is clinically defined by the rapid induction of stronger responses, with a higher affinity, after boosting than after primary immunization. Long-lived plasma cells are generated in response to T cell–dependent antigens during the germinal center reaction and are primarily found in the bone marrow, where stromal cells provide specific niches supporting their retention and survival15. The maximal life-span of bone-marrow plasma cells is still debated. It is, however, agreed that it is not lifelong and that the bone-marrow reservoir is replenished by the stimulation of memory B cells and their differentiation into plasma cells16,17. Memory B cells survive in the absence of antigen and can be induced to proliferate and differentiate by exposure to antigens from frequently reoccurring pathogens, or cross-reacting pathogens, or to persisting antigens as in chronic or latent infections. It has been suggested that memory B cells also undergo continuous polyclonal activation18, but whether this contributes to the maintenance of significant antibody levels is unclear.
A few of the factors controlling the differentiation of vaccine antigen-specific B cells toward short- or long-lived plasma cells or toward memory B cells have been identified. Apart from the requirement of CD4+ T cells to initiate germinal center reactions, these factors include the nature of the antigen19 and its dose: higher doses tend to favor the rapid induction of short-term effectors, whereas lower doses of antigens preferentially support the induction of immune memory20,21,22. Rapid vaccine schedules including several closely spaced vaccine doses preferentially support short-term responses, requiring additional later boosting for sustained immunity23. This is thought to reflect the time needed for affinity maturation and subsequent reactivation of memory B cells with enhanced antigen-specific affinity (Fig. 1b). In experimental models, the in vivo persistence of antigen and its tissue distribution contribute to the duration of immune memory24, probably by extending the period of antigen-specific memory B-cell reactivation. How this applies to humans and whether slow- or intermittent-release formulations could support long-term antibody responses is unknown.
Antitoxin antibody responses to vaccination are of particular value for analyzing the role of antibody maturation. For example, tetanus toxin (TeNT) poisoning occurs as the outcome of three discrete stages25. After the neurotoxin binds to specific membrane receptors located only on nerve terminals (requiring the presence of gangliosides, in particular GD1b26), TeNT is internalized into neurons. Once internalized into acidic compartments, the toxin can no longer be neutralized by antibodies. Therefore, protection requires that neutralizing antibodies be present at the time of toxin exposure (Fig. 2). The affinity of TeNT for GD1b is relatively low (Kd 1.5 × 10−7) as compared to that of tested human monoclonal antibodies against TeNT derived from vaccinated individuals27, and protection, as assessed by in vitro tests, correlates with the recognition of the toxin binding site, with a marked influence of antibody affinity28.
Influencing the antibody affinity-maturation process is an obvious goal of vaccine design efforts, particularly through adjuvant selection. As most existing subunit vaccines are based on the use of aluminum as adjuvant, data on alternative adjuvants are limited. However, it has been recently observed that CpG oligonucleotides could increase the affinity maturation process of antibodies specific for hepatitis B surface antigen (HBsAg) in human volunteers when added to an aluminum-based HBsAg formulation29 (Fig. 3). Studies in mice have shown that CpG oligonucleotides enhance the persistence of plasma cells in the spleen and in consequence markedly increase the bone marrow plasma cell pool30. This indicates that CpG oligonucleotides may exert an anti-apoptotic influence directly or indirectly enhancing B-cell survival. Defining the mechanism underlying this effect may help in explaining the failure of other adjuvants to enhance the affinity-maturation process.
This is shown here 52 weeks after priming in human volunteers. Three doses of vaccine are given intramuscularly at 0, 4 and 24 weeks. HBs is given either alone or mixed with 0.5 or 1 mg of CpG7909. (Derived from ref. 29.) The avidity index reflects the affinity of antibodies against the main B cell epitopes of the vaccine antigen.
So far, successful vaccines against encapsulated bacteria (bacteria with a polysaccharide coat) are all directed at the capsular polysaccharides. Whether induced by polysaccharide vaccines or by conjugated vaccines (in which the polysaccharide is covalently linked to a protein antigen as carrier), complement-binding antibodies that recognize repetitive saccharidic epitopes are key to protective effects. Protection persists as long as actively induced or passively acquired antibodies are present in blood and is mainly due to opsono-phagocytic mechanisms (antibodies binding to bacteria and thus facilitating their phagocytosis and elimination), with some contribution of direct bactericidal effects. The affinity of human anti-pneumococcal antibodies seems to be an essential feature of protection after transfer in an appropriate murine model of pneumococcal infection31. When used at a similar molar concentration, the protection conferred depends on the relative affinity of each antibody for the relevant polysaccharidic epitope. These data explain why an efficient protection can be provided by type b Haemophilus influenzae (Hib) conjugate vaccines in some infants who respond to a primary immunization series by producing a relatively low abundance of antibody (for example, 0.15 μg/ml) of high affinity, as a result of normal priming and affinity maturation. Thus assessments of antibody affinity should be included when defining surrogate serologic tests for the prediction of vaccine efficacy.
The race between memory reactivation and microbial invasion
With the exception of T cell–independent polysaccharide-based vaccines, all existing vaccines induce immunological memory. Yet the magnitude and duration of memory differs considerably between vaccine types and it is essential to understand determinants that enhance or limit the duration of vaccine efficacy.
As mentioned above, protection by toxoid-based vaccines requires the persistence of antitoxin antibodies at the time of toxin exposure. For example, the high proportion of adult cases during a large diphtheria outbreak in the former Soviet Union indicated that in the context of a short incubation period (1–5 d), pathogen-induced reactivation of immune memory was not sufficient to protect against diphtheria. In this setting, the development of protective antibody titers after a single boost indicated that most adults, although immunized in childhood, had lost immunity over time32. Conversely, memory seems to be quite efficient for ensuring long-lived protection against hepatitis B. After acute infection, unless immediately neutralized by a sufficient level (>10 International Units/L) of circulating antibodies, hepatitis B virus reaches the liver and initiates its replication within hepatocytes. In naive subjects, this leads to the production of viral antigens, which slowly trigger immune responses that may, or may not, result in viral clearance. In vaccinated subjects, viral replication rapidly drives the activation of vaccine-induced memory cells into effector cells capable of interrupting viral replication before the onset of chronic liver disease. The sustained efficacy of hepatitis B immunization thus relies on a rather long viral incubation period (4–12 weeks between exposure and hepatitis) that exceeds the few days required for the reactivation of HBsAg-specific memory cells. Because the initial stages of infection remain asymptomatic, immunocompetent vaccinated subjects do not require booster doses of hepatitis B vaccine to remain protected, despite the disappearance of anti-HBsAg antibodies33. The role of T-cell responses in this prolonged vaccine-induced protection remains to be determined.
Vaccines against encapsulated bacteria such as Hib, Streptococcus pneumoniae or Neisseria meningitidis illustrate both the importance of immune memory and its limitations. The short-term efficacy of polysaccharide vaccines is attributed to their failure to induce T cell–dependent germinal center reactions, long-term high-affinity plasma cells and immune memory. Waning of antibodies and lack of immunological memory limit vaccine efficacy to a few years and may even be associated with a decreased responsiveness to certain polysaccharides upon re-exposure. In contrast, glycol-conjugate vaccines, in which polysaccharides are covalently linked to a carrier protein, are T cell–dependent antigens that elicit germinal center reactions and hence immune memory. This is reflected by a relatively rapid (4–7-d) induction of high titers of high-affinity antibodies upon administration of plain polysaccharide to previously primed individuals34. Memory is readily demonstrated in children in whom vaccine-induced Hib antibody titers have fallen to undetectable levels35. However, immune memory is also evidenced in children with invasive Hib disease, indicating that it may not be sufficient to protect against severe disease36. This discrepancy between the demonstration of immune memory and actual protection may reflect the time required for production of sufficient levels of circulating antibodies after memory B-cell reactivation and differentiation, which may limit the ability to interrupt bacterial invasion. However, such secondary Hib vaccine failures have been relatively rare and primarily observed in countries where the selected priming strategies (use of vaccines of lower immunogenicity or early accelerated schedule of primary infant immunization without a second-year booster) have been less efficient than expected37. Similar considerations may apply to conjugate vaccines against group C meningococcal diseases. Such vaccines seem to be highly efficacious during the first year after priming but less so during the following 3 years38. This correlates with a relatively rapid decline of vaccine-induced meningococcus C antibodies. Given the prolonged risk period of group C meningococcus, which affects young children and adolescents, the number and timing of booster doses needed to confer sustained protection is of critical concern.
The role of recurrent antigen exposure
Viral attenuated vaccines such as measles, mumps, rubella, varicella, polio or yellow fever vaccines are considered to be inducers of life-long immunity. However, natural antigen exposure due to continued viral circulation is likely to play an essential role in the duration of vaccine efficacy. In the absence of recurrent exposure to measles, mumps or rubella, antibody titers tend to slowly decline39, and this results into a growing proportion of seronegative vaccinated young adults, including women of childbearing age. Might that result in the resurgence of rubella infections during pregnancy, of mumps in young men or of measles in young adults? Although reactivation of immune memory could in theory curtail the replication process and confer some protection against disease severity, careful surveillance is required to assess whether an additional vaccine dose might become necessary for young adults primed in early childhood. The same questions apply to varicella zoster virus (VZV). The lower risk of zoster in adults frequently exposed to chickenpox40 indicates that recurrent exposure to VZV may play a role in maintaining immunity in the adult population. On that basis, it has been suggested that the risk of zoster may increase in previously infected adults if universal varicella vaccination interrupts viral circulation and may therefore necessitate the administration of booster doses.
Relative contribution of effector T-cell responses
Vaccine-induced T-cell responses have been demonstrated for most protein or live vaccines that are routinely used. T helper (TH) and occasionally cytolytic T lymphocyte (CTL) responses can be measured after immunization with inactivated vaccines, such as hepatitis B, pertussis, diphtheria, tetanus and influenza vaccines, as well as with a number of live vaccines, including measles, mumps, rubella, varicella, vaccinia and bacille Calmette-Guerin (BCG). However, the relative importance of T cell–mediated effector mechanisms in the protection achieved with these vaccines is often unknown (Table 2).
BCG, the only licensed tuberculosis vaccine, is the prototype of vaccines relying on T cell–dependent mechanisms to protect vaccinees. A number of studies (see the accompanying review by Kaufmann in this supplement41) have shown that BCG does not significantly induce antibodies but generates CD4+ T-cell responses in human infants. Clinical trials that have examined the ability of neonatal BCG vaccination to protect against primary tuberculosis in children have consistently shown efficacy in the range of 50–70% protection. More discordant results are obtained in trials involving older age groups. For example, whereas vaccination of 12–14-year-olds in the United Kingdom demonstrated 75% protective efficacy, a large trial in South India did not show any protection. The major arm of BCG-induced mycobacterial immunity seems to be the delivery of macrophage activation signals—predominantly interferon (IFN)-γ—by antigen-specific CD4+ T cells. Immunized children have been shown to rapidly develop a high level of specific IFN-γ–producing CD4+ T cells. However, although IFN- γ is clearly an essential element of the protective response, the total amount of IFN-γ produced does not necessarily reflect the effectiveness of the immune response. Other immune mechanisms, particularly CD8+ T-cells, may also contribute to this protective process either by providing a supplementary source of IFN-γ, by triggering apoptotic pathways that can promote killing of intracellular mycobacteria, or through the destruction of infected macrophages. T cells that recognize non-protein antigens presented by CD1 molecules on dendritic cells and activated macrophages may also make an important contribution to the human immune response to BCG. The main lessons from the successes and failures of BCG are that (i) protection against disease can be obtained with a vaccine that induces only T cell–mediated responses (ii) such protection does not last forever, and (iii) pre-exposure to cross-reacting mycobacteria may interfere with vaccine efficacy.
Although BCG is the only vaccine currently used for which there is evidence that T cells are the main effectors, there is indirect evidence that T cells contribute to the protection conferred by some other vaccines through accelerated bacterial or viral clearance. Such mechanisms have been suggested to explain the persistence of protection against clinical pertussis in children primed in infancy and who have largely lost vaccine-induced antibodies42,43. Effector T-cell responses have also been demonstrated in 6-month-old infants who fail to raise antibody responses to measles vaccine because antibodies of maternal origin are present. These children are likely to be susceptible to infection but protected against severe disease43,44.
Although no successful malaria vaccine has been licensed so far, recent progress have been made indicating that immunization with RTSS, a recombinant vaccine derived from Plasmodium falciparum circumsporozoite protein, can prevent severe disease in up to 58% of children45. The experience obtained through efforts toward developing this candidate vaccine has been quite informative. In the presence of two different adjuvant formulations, the same protein construct was shown to protect, or not protect, human volunteers against a malaria challenge while similar levels of antibodies were induced against the parasite antigen46. In agreement with experimental data demonstrating the importance of T-cell responses (including CD8+ effector T cells), results of human studies indicate that T cell–mediated mechanisms may participate in vaccine-induced protection. Other malaria vaccines are now at an advanced development stage46.
Vaccine boosting and the original antigenic sin
It is often difficult to further increase antibody levels, specificity and the quality of the immune response in individuals who have been repeatedly immunized through either vaccination or recurrent exposure to infectious agents or cross-reacting microbial antigens. This has been a particular concern for aging adults in the context of the antigenic drift of influenza virus, in view of their annual exposure to antigens of new but related influenza variants through either infection or vaccination. After exposure to a new but cross-reacting antigenic variant, such individuals may respond by producing antibodies that are primarily directed at antigens characterizing influenza viruses encountered during earlier epidemics. This is the phenomenon of so-called 'original antigenic sin'47. Individuals that were exposed 50 years earlier to a given H1N1 influenza virus strain have been shown to respond differently from first-time adult vaccinees to a recent influenza H1N1 vaccine antigen with partial epitope similarities with the 'old' H1N1 influenza strain. There was a preferential induction of antibodies specific for hemagglutinin epitopes of the 'old' H1N1 strain rather than cross-reacting epitopes of the new strain48. On the basis of such observations, it was proposed that variations in the efficacy of repeat vaccines might be due to differences in antigenic distances between vaccine strains and the epidemic strains responsible for influenza outbreaks49. Accordingly, the closeness of the antigenic match between the vaccine strain and the epidemic virus would be important for vaccine efficacy in first-time vaccinees, whereas the closeness of the vaccine and epidemic strains to previously encountered vaccine strains would determine how vaccine efficacy might be modulated by prior vaccination. First-time vaccinees would be expected to develop a better response to cross-reacting strains than would previously exposed individuals. Original antigenic sin largely reflects the fact that cross-reactive epitopes preferentially reactivate previously induced high-affinity memory B cells rather than recruiting lower-affinity naive B cells in the presence of persisting cross-reacting antibodies (Fig. 4). Until now, original antigenic sin has been largely regarded as an antibody-related phenomenon.
Exposure to a highly cross-reacting influenza epitope ('strain 2') is more likely to recruit primarily memory B cells that have been induced against the originally priming influenza antigen ('strain 1') rather than naive B cells specific for the cross-reacting epitope. The latter are more likely to be inhibited by persisting anti–strain 1 antibodies. ASC, antibody-secreting cell.
Although such 'deviating' immunological effects are likely to occur, their impact on protection is far from established. The effect of annual influenza revaccination on mortality was recently investigated in a population-based cohort study in the Netherlands that included community-dwelling individuals aged 65 years or older50. Overall, during a 5-year period (1996–2002), annual revaccination was associated with a significantly reduced mortality risk of 24%, whereas the annual reduction of mortality risk was only 10% in first-time vaccinees. Thus original antigenic sin does not seem to be a major practical obstacle in the race against antigenic changes that characterizes anti-influenza vaccination and it may not require specific strategies for overcoming resulting limitations of immune responses in vaccinees.
Antigenic diversity: a challenge that can be met
At its simplest, the solution to the problem of strain diversity has been the inclusion of multiple different strains of a pathogen in each vaccine. For polio, all three antigenic types are included in the vaccine51. For the pneumococcal vaccines, a 23-valent polysaccharide vaccine and a 7-valent polysaccharide-protein conjugate vaccine are used. In these cases, the differing immunogenicity of the various polysaccharide antigens is accommodated by adjusting the amount of each antigen in the final combination to induce an optimal antibody response. Another multistrain disease agent is rotavirus, which is characterized by over 90 serotypes. However, 96% of the strains contain four particular combinations of two outer capsid proteins, thus vastly reducing the number of theoretical antigen combinations from 90 to a more feasible number for a multivalent vaccine (reviewed in ref. 52).
For the influenza vaccine, three different strains are included each year—one each of the A H1N1, A H3N2 and B viral strains. But this trivalent vaccine must be reformulated each year because each subtype also evolves through mutation and reassortment. To complicate matters, additional subtypes of influenza seem to have crossed the species barrier to cause human disease, necessitating the development of vaccines that will protect against what have, until recently, been considered avian strains of influenza. Influenza thus provides an example of the additional complexity engendered when the virus can mutate or reassort rapidly enough to require that the vaccine either be frequently reformulated or be capable of inducing broad, cross-strain immune responses. HIV may provide the most extreme example of this sort of evolutionary capability.
Pneumococcal vaccines illustrate other issues that are relevant to vaccine development. First, even if all of the relevant strains of a pathogen are not included in the vaccine, the vaccine can still be useful if it includes enough of the strains that are responsible for the majority of disease. For example, the 23-valent pneumococcal vaccine includes the strains that account for around 90% of invasive pneumoccocal disease and the 7-valent conjugate vaccines protects against 80% of invasive pneumococcal disease in the young pediatric population in the United States (reviewed in refs. 53,54). Similarly, in the development of vaccines for human papilloma virus (HPV), although there are dozens of strains of HPV, four strains account for the majority (80%) of infections associated with the subsequent development of cervical cancer55. Thus both prophylactic and therapeutic vaccine efforts are focusing on a limited number of strains to maximize the impact and feasibility of an HPV vaccine. In addition to the realities of selective immune pressure driving the development of new strains of a pathogen (as is seen with influenza), immunization with selected strains of a pathogen raises the possibility of changing its ecological niche. For example, an increase in non-vaccine pneumococcal strains colonizing the nasopharynx has been observed after immunization (reviewed in ref. 53). There is now preliminary evidence that a pneumococcal strain replacement can occur, including the emergence of invasive strains56.
As a last point, in various regions of the world, the prevalence of strains differs. Because of this, vaccines may need to be customized for different areas. This is a complicated process made even more difficult by the fact that for some diseases the necessary epidemiologic information does not exist. Additionally, the process of producing, testing and licensing different vaccines is expensive and holds little appeal for vaccine manufacturers, particularly for vaccines that are in themselves difficult and costly to produce, such as polysaccharide protein conjugate vaccines for meningococcus and pneumococcus and recombinant virus-like particles for HPV.
Vaccines 'tailored' to the targeted population
Vaccines for protection in early life. Immunization promptly after birth is required to induce active immunity against diseases that may occur very early in life, such as tuberculosis, hepatitis B, polio, pertussis or invasive diseases involving encapsulated bacteria. It also confers considerable logistic advantage, because access to vaccination services is much better early in infancy than later in life. Unfortunately, this strategy is limited by the relative immaturity of the neonatal and infant immune system, which may interfere with the induction of protective vaccine responses early in life.
Vaccine antibody responses to infant bacterial and viral vaccines increase with age in a stepwise manner57. Infant B-cell responses to most T cell–independent polysaccharide antigens are poor. Implicated factors include limited switch from IgM to IgG2 antibodies, impaired complement-mediated reactions and deficient organization of the splenic marginal zone. However, immaturity also affects responses to glycol conjugates and to most T cell–dependent vaccines, such that only the most immunogenic vaccines show significant protective efficacy after a single infant dose. This limitation of IgG antibody responses extends throughout the first year of life, and it partly affects responses to measles vaccine at 6 or 9 months of age58 and to varicella immunization at 12 months of age59. Murine models assessing neonatal responses to human infant vaccines indicate that limited germinal center reactions probably result from the delayed development of follicular dendritic cells and limit plasma cell differentiation60. Whether this applies to human infants is as yet unknown.
Vaccine antibody responses elicited in the first year of life also decline rapidly. This affects even the most immunogenic vaccines, such as toxoids or glyco-conjugate vaccines: three infant doses of serogroup C meningococcal vaccines confer 93% efficacy for 1 year, but efficacy declines to undetectable levels as antibodies disappear38. Work in mouse models has shown that the neonatal bone marrow has a limited capacity to support the establishment of long-lived antibody-secreting plasmocytes61. Whether the induction of long-lived plasma cells is similarly limited in human infants is unknown, but short-lived antibody responses are a hallmark of early-life immunization with most although not all vaccines (an exception being hepatitis B). Importantly, factors limiting the magnitude and duration of infant responses do not prevent efficient priming, such that neonatally triggered immune memory may be readily recalled later in life. Few studies have yet compared the affinity maturation process of vaccine responses in infants and adults; this also seems to be functional very early in life (P.H.L. and C.-A.S., unpublished observations). Thus, immunization schedules including neonatal priming and infant boosting may be effective even when pathogen exposure occurs very early in life. Unfortunately, however, immune memory is not sufficient to confer full protection against pathogens that require neutralizing antibodies either at the site of infection (respiratory syncytial virus, influenza) or rapidly after exposure (encapsulated bacteria), and these remain major threats to young infants.
Another characteristic of neonatal responses is a relative impairment of IFN-γ production by CD4+ TH1 cells. This seems to reflect, at least in part, the limited IL-12 and IFN-α responses of neonatal dendritic cells upon Toll-like receptor (TLR) ligation62,63. Notably, the addition of INF-γ is sufficient to circumvent the IL-12 defect64 and recent clinical observations have unambiguously established the possibility of inducing efficient T-cell vaccine responses in infants if sufficient co-stimulation is provided (reviewed in ref. 57). Although human newborns generate lower IFN-γ responses to HBsAg than adults65, similar responses to BCG are obtained in both age groups66. A better understanding of the molecular and cellular determinants of neonatal T-cell responses will be required to develop vaccine formulations or adjuvants capable of circumventing the limitations of early-life responses. Notably, the effect of adjuvants in neonates may not be predictable from observations in adults. As a case in point, the neonatal administration of the TH1-inducing BCG vaccine was shown to markedly enhance TH1, TH2 and antibody responses to a simultaneously administered hepatitis B vaccine67.
Vaccination in the context of maternal antibodies. The inhibitory influence of maternal antibodies (MatAb) on infant antibody responses has been demonstrated in all species and its mechanisms reviewed elsewhere57. It is generally epitope specific and primarily affects B-cell responses. It does not merely result from the neutralization of in vivo viral vaccine replication or FcR-mediated inhibition of infant B-cell activation, but primarily depends on specific epitope neutralization and competition with relevant antigen-specific receptors on naive B cells (Fig. 5). The ratio of MatAb to vaccine antigen at the time of immunization thus plays a crucial role, whether for live attenuated (for example, measles) or subunit vaccines. A twofold increase in hepatitis A vaccine dose was sufficient to circumvent the MatAb-mediated inhibition of infant responses68. Most importantly, MatAb do not interfere with the induction of infant T-cell responses44. Thus, carrier-specific MatAb can occasionally enhance antibody responses to the polysaccharide moiety of glycol conjugates, whereas MatAb-mediated inhibition of primary antibody responses does not generally prevent secondary responses to booster immunization.
Vaccines for the elderly. Aging may result in reduced levels of vaccine-induced protection, but this does not usually occur until very late in life. Some vaccine are more sensitive to such 'immunosenescence'; an example is antibody responses to pneumococcal polysaccharides69, whereas responses to a boosting dose of tetanus vaccine are scarcely affected by age70. Immunosenescence is characterized by a rapid waning of antibody responses and a relative restriction of the T-cell repertoire. With age, there is a progressive accumulation of a major subgroup of CD8+ T cells at a terminal stage of differentiation, which seem to be specific for cytomegalovirus (CMV) epitopes, and this is an important part of what has been described as an 'immune risk phenotype' in the elderly71. However, the CD4+ T cell responses of healthy elderly individuals to 'neo-antigens', such as rabies or tick-borne encephalitis vaccines, seem to be largely unaltered, and vaccination leads to a rapid induction of effector T cells72. Influenza vaccination also results in a significant enhancement of influenza cross-reactive CTLs73 and may be an important determinant of vaccine-induced protection against serious illness in this age group.
In general, vaccination in the elderly may be less efficacious than in younger adults and it may require a more aggressive vaccine design, including ad hoc formulations, and frequent boosters. Research on optimal vaccination strategies in this age group is still very limited and should be strongly encouraged. However, most successful adult vaccines have proven sufficiently efficacious in this targeted population to have a favorable benefit/risk ratio and to be cost effective.
Concluding remarks
Short-term protection conferred by most successful existing vaccines seems to be antibody mediated, and the quality of antibody responses, particularly affinity maturation, is often crucial to vaccine efficacy. Although it may be reassuring to rely on memory responses for long-term protection, one should be aware of the limitations of recall responses when microbial invasion can be faster than B-cell reactivation. Although T-cell effector mechanisms are not primarily involved in the short-term protection induced by most existing vaccines, they are likely to have a role in long-term effects and it would be unreasonable to ignore this arm of vaccine responses, including regulatory T cells, in the development of new vaccines. Vaccine design or formulation, the selection of appropriate vaccination strategies, and consideration of the immunological profile of the target population at initial steps of vaccine design are critical to achieve optimal efficacy. Therefore, deciphering the biological bases for the efficacy of existing vaccines may give us some clues regarding optimal development strategies. It also pinpoints reasons for observed failures. Such information should help to pave the way toward some of the most challenging new vaccines.
References
Janeway, C.A. Use of concentrated human serum γ-globulin in the prevention and attenuation of measles. Bull. N. Y. Acad. Med. 21, 202–222 (1945).
Keller, M.A. & Stiehm, E.R. Passive immunity in prevention and treatment of infectious diseases. Clin. Microbiol. Rev. 13, 602–614 (2000).
Fox, J.P. Modes of action of poliovirus vaccines and relation to resulting immunity. Rev. Infect. Dis. 6 (Suppl. 2), S352–S355 (1984).
De Quadros, C.A. Polio. in The Vaccine Book (eds. Bloom, B.R. & Lambert, P.H.) 189–196 (Academic Press, Amsterdam, 2003).
Strebel, P.M., Papania, M.J. & Halsey, N.A. Measles vaccine. in Vaccines (eds. Plotkin, S.A. & Orenstein, W.A.) 389–440 (Elsevier, Philadelphia, 2004).
Lampe, R.M., Weir, M.R., Scott, R.M. & Weeks, J.L. Measles reimmunization in children immunized before 1 year of age. Am. J. Dis. Child. 139, 33–35 (1985).
Fukuda, K., Levandowski, R.A., Bridges, C.B. & Cox, N.J. Inactivated influenza vaccines. in Vaccines (eds. Plotkin, S.A. & Orenstein, W.A.) 339–370 (Elsevier, Philadelphia, 2004).
Belshe, R., Maassab, H.G. & Mendelman, P.M. Influenza vaccine—live. in Vaccines (eds. Plotkin, S.A. & Orenstein, W.A.) 371–388 (Elsevier, Philadelphia, 2004).
Davies, J.R. & Grilli, E.A. Natural or vaccine-induced antibody as a predictor of immunity in the face of natural challenge with influenza viruses. Epidemiol. Infect. 102, 325–333 (1989).
Treanor, J.J. et al. Evaluation of trivalent, live, cold-adapted (CAIV-T) and inactivated (TIV) influenza vaccines in prevention of virus infection and illness following challenge of adults with wild-type influenza A (H1N1), A (H3N2), and B viruses. Vaccine 18, 899–906 (1999).
Belshe, R.B. et al. Correlates of immune protection induced by live, attenuated, cold-adapted, trivalent, intranasal influenza virus vaccine. J. Infect. Dis. 181, 1133–1137 (2000).
Manz, R.A., Hauser, A.E., Hiepe, F. & Radbruch, A. Maintenance of serum antibody levels. Annu. Rev. Immunol. (in the press).
McHeyzer-Williams, L.J. & McHeyzer-Williams, M. Antigen-specific memory B cell development. Annu. Rev. Immunol. (in the press).
Gourley, T.S., Wherry, E.J., Masopust, D. & Ahmed, R. Generation and maintenance of immunological memory. Semin. Immunol. 16, 323–333 (2004).
Tokoyoda, K., Egawa, T., Sugiyama, T., Choi, B.I. & Nagasawa, T. Cellular niches controlling B lymphocyte behavior within bone marrow during development. Immunity 20, 707–718 (2004).
Ochsenbein, A.F. et al. Protective long-term antibody memory by antigen-driven and T help-dependent differentiation of long-lived memory B cells to short-lived plasma cells independent of secondary lymphoid organs. Proc. Natl. Acad. Sci. USA 97, 13263–13268 (2000).
Zinkernagel, R.M. On differences between immunity and immunological memory. Curr. Opin. Immunol. 14, 523–536 (2002).
Bernasconi, N.L., Traggiai, E. & Lanzavecchia, A. Maintenance of serological memory by polyclonal activation of human memory B cells. Science 298, 2199–2202 (2002).
Pinschewer, D.D. et al. Kinetics of protective antibodies are determined by the viral surface antigen. J. Clin. Invest. 114, 988–993 (2004).
Nicol, M. et al. Haemophilus influenzae type b conjugate vaccine diluted tenfold in diphtheria-tetanus-whole cell pertussis vaccine: a randomized trial. Pediatr. Infect. Dis. J. 21, 138–141 (2002).
Cassidy, W.M. et al. A randomized trial of alternative two- and three-dose hepatitis B vaccination regimens in adolescents: antibody responses, safety, and immunologic memory. Pediatrics 107, 626–631 (2001).
Ahman, H., Kayhty, H., Vuorela, A., Leroy, O. & Eskola, J. Dose dependency of antibody response in infants and children to pneumococcal polysaccharides conjugated to tetanus toxoid. Vaccine 17, 2726–2732 (1999).
Bosnak, M., Dikici, B., Bosnak, V. & Haspolat, K. Accelerated hepatitis B vaccination schedule in childhood. Pediatr. Int. 44, 663–665 (2002).
Zinkernagel, R.M. et al. Antigen localisation regulates immune responses in a dose- and time-dependent fashion: a geographical view of immune reactivity. Immunol. Rev. 156, 199–209 (1997).
Deloye, F., Doussau, F. & Poulain, B. Action mechanisms of botulinum neurotoxins and tetanus neurotoxins. C.R. Seances Soc. Biol. Fil. 191, 433–450 (1997).
Turton, K., Chaddock, J.A. & Acharya, K.R. Botulinum and tetanus neurotoxins: structure, function and therapeutic utility. Trends Biochem. Sci. 27, 552–558 (2002).
Matsuda, M., Kamei, M., Sugimoto, N., Ma, Y. & Hashizume, S. Characteristics of toxin-neutralization by anti-tetanus human monoclonal antibodies directed against the three functional domains [A], [B] and [C] of the tetanus toxin molecule and a reliable method for evaluating the protective effects of monoclonal antibodies. Eur. J. Epidemiol. 8, 1–8 (1992).
Gupta, R.K. & Siber, G.R. Comparative analysis of tetanus antitoxin titers of sera from immunized mice and guinea pigs determined by toxin neutralization test and enzyme-linked immunosorbent assay. Biologicals 22, 215–219 (1994).
Siegrist, C.A. et al. Co-administration of CpG oligonucleotides enhances the late affinity maturation process of human anti-hepatitis B vaccine response. Vaccine 23, 615–622 (2004).
Pihlgren, M. et al. CpG-motifs enhance initial and sustained primary tetanus-specific antibody secreting cell responses in spleen and bone marrow, but are more effective in adult than in neonatal mice. Vaccine 21, 2492–2499 (2003).
Usinger, W.R. & Lucas, A.H. Avidity as a determinant of the protective efficacy of human antibodies to pneumococcal capsular polysaccharides. Infect. Immun. 67, 2366–2370 (1999).
Golaz, A. et al. Evaluation of a single dose of diphtheria-tetanus toxoids among adults in Odessa, Ukraine, 1995: immunogenicity and adverse reactions. J. Infect. Dis. 181 Suppl 1, S203–S207 (2000).
Banatvala, J., Van Damme, P. & Van Hattum, J. Boosters for hepatitis B. European Consensus Group on Hepatitis B Immunity. Lancet 356, 337–338 (2000).
Goldblatt, D., Vaz, A.R. & Miller, E. Antibody avidity as a surrogate marker of successful priming by Haemophilus influenzae type b conjugate vaccines following infant immunization. J. Infect. Dis. 177, 1112–1115 (1998).
Goldblatt, D., Miller, E., McCloskey, N. & Cartwright, K. Immunological response to conjugate vaccines in infants: follow up study. Br. Med. J. 316, 1570–1571 (1998).
McVernon, J., Johnson, P.D., Pollard, A.J., Slack, M.P. & Moxon, E.R. Immunologic memory in Haemophilus influenzae type b conjugate vaccine failure. Arch. Dis. Child. 88, 379–383 (2003).
Kelly, D.F., Moxon, E.R. & Pollard, A.J. Haemophilus influenzae type b conjugate vaccines. Immunology 113, 163–174 (2004).
Trotter, C.L., Andrews, N.J., Kaczmarski, E.B., Miller, E. & Ramsay, M.E. Effectiveness of meningococcal serogroup C conjugate vaccine 4 years after introduction. Lancet 364, 365–367 (2004).
Davidkin, I., Peltola, H., Leinikki, P. & Valle, M. Duration of rubella immunity induced by two-dose measles, mumps and rubella (MMR) vaccination. A 15-year follow-up in Finland. Vaccine 18, 3106–3112 (2000).
Thomas, S.L. & Hall, A.J. What does epidemiology tell us about risk factors for herpes zoster? Lancet Infect. Dis. 4, 26–33 (2004).
Kaufmann, S.H.E. & McMichael, A. Annulling a dangerous liaison: vaccination strategies against AIDS and tuberculosis. Nat Med. 11, Suppl 1, S33–S44 (2005).
Salmaso, S. et al. Sustained efficacy during the first 6 years of life of 3-component acellular pertussis vaccines administered in infancy: the Italian experience. Pediatrics 108, E81 (2001).
Giuliano, M. et al. Antibody responses and persistence in the two years after immunization with two acellular vaccines and one whole-cell vaccine against pertussis. J. Pediatr. 132, 983–988 (1998).
Gans, H.A. et al. IL-12, IFN-γ, and T cell proliferation to measles in immunized infants. J. Immunol. 162, 5569–5575 (1999).
Alonso, P.L. et al. Efficacy of the RTS,S/AS02A vaccine against Plasmodium falciparum infection and disease in young African children: randomised controlled trial. Lancet 364, 1411–1420 (2004).
Ballou, W.R. et al. Update on the clinical development of candidate malaria vaccines. Am. J. Trop. Med. Hyg. 71, 239–247 (2004).
Hoskins, T.W., Davies, J.R., Smith, A.J., Miller, C.L. & Allchin, A. Assessment of inactivated influenza-A vaccine after three outbreaks of influenza A at Christ's Hospital. Lancet 1, 33–35 (1979).
Powers, D.C. & Belshe, R.B. Vaccine-induced antibodies to heterologous influenza A H1N1 viruses: effects of aging and “original antigenic sin”. J. Infect. Dis. 169, 1125–1129 (1994).
Smith, D.J., Forrest, S., Ackley, D.H. & Perelson, A.S. Variable efficacy of repeated annual influenza vaccination. Proc. Natl. Acad. Sci. USA 96, 14001–14006 (1999).
Voordouw, A.C. et al. Annual revaccination against influenza and mortality risk in community-dwelling elderly persons. J. Am. Med. Assoc. 292, 2089–2095 (2004).
Robbins, F.C. The history of polio vaccine development. in Vaccines (eds. A., P.S. & Orenstein, W.A.) 17–30 (Elsevier, Philadelphia, 2004).
Bresee, J.S., Glass, R.I., Parashar, U. & Gentsch, J.G. Rotavirus. in The Vaccine Book (eds. Bloom, B.R. & Lambert, P.H.) 225–243 (Academic Press, Amsterdam, 2003).
Hackell, J.G. Pneumococcus, pneumococcal disease and prevention. in The Vaccine Book (eds. Bloom, B.R. & Lambert, P.H.) 257–277 (Academic Press, Amsterdam, 2003).
Hausdorff, W.P., Bryant, J., Paradiso, P.R. & Siber, G.R. Which pneumococcal serogroups cause the most invasive disease: implications for conjugate vaccine formulation and use, part I. Clin. Infect. Dis. 30, 100–121 (2000).
Bosch, F.X. et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J. Natl. Cancer Inst. 87, 796–802 (1995).
Kaplan, S.L. et al. Decrease of invasive pneumococcal infections in children among 8 children's hospitals in the United States after the introduction of the 7-valent pneumococcal conjugate vaccine. Pediatrics 113, 443–449 (2004).
Siegrist, C.A. Neonatal and early life vaccinology. Vaccine 19, 3331–3346 (2001).
Gans, H.A. et al. Deficiency of the humoral immune response to measles vaccine in infants immunized at age 6 months. J. Am. Med. Assoc. 280, 527–532 (1998).
Vazquez, M. et al. Effectiveness over time of varicella vaccine. J. Am. Med. Assoc. 291, 851–855 (2004).
Pihlgren, M. et al. Unresponsiveness to lymphoid-mediated signals at the neonatal follicular dendritic cell precursor level contributes to delayed germinal center induction and limitations of neonatal antibody responses to T-dependent antigens. J. Immunol. 170, 2824–2832 (2003).
Pihlgren, M. et al. Delayed and deficient establishment of the long-term bone marrow plasma cell pool during early life. Eur. J. Immunol. 31, 939–946 (2001).
Goriely, S. et al. Deficient IL-12(p35) gene expression by dendritic cells derived from neonatal monocytes. J. Immunol. 166, 2141–2146 (2001).
De Wit, D. et al. Blood plasmacytoid dendritic cell responses to CpG oligodeoxynucleotides are impaired in human newborns. Blood 103, 1030–1032 (2004).
Goriely, S. et al. A defect in nucleosome remodeling prevents IL-12(p35) gene transcription in neonatal dendritic cells. J. Exp. Med. 199, 1011–1016 (2004).
Ota, M.O. et al. Hepatitis B immunisation induces higher antibody and memory Th2 responses in new-borns than in adults. Vaccine 22, 511–519 (2004).
Marchant, A. et al. Newborns develop a Th1-type immune response to Mycobacterium bovis bacillus Calmette-Guerin vaccination. J. Immunol. 163, 2249–2255 (1999).
Ota, M.O. et al. Influence of Mycobacterium bovis bacillus Calmette-Guerin on antibody and cytokine responses to human neonatal vaccination. J. Immunol. 168, 919–925 (2002).
Dagan, R. et al. Immunization against hepatitis A in the first year of life: priming despite the presence of maternal antibody. Pediatr. Infect. Dis. J. 19, 1045–1052 (2000).
Shapiro, E.D. et al. The protective efficacy of polyvalent pneumococcal polysaccharide vaccine. N. Engl. J. Med. 325, 1453–1460 (1991).
Bjorkholm, B., Hagberg, L., Sundbeck, G. & Granstrom, M. Booster effect of low doses of tetanus toxoid in elderly vaccinees. Eur. J. Clin. Microbiol. Infect. Dis. 19, 195–199 (2000).
Pawelec, G. et al. Is immunosenescence infectious? Trends Immunol. 25, 406–410 (2004).
Gomez, I., Marx, F., Gould, E.A. & Grubeck-Loebenstein, B. T cells from elderly persons respond to neoantigenic stimulation with an unimpaired IL-2 production and an enhanced differentiation into effector cells. Exp. Gerontol. 39, 597–605 (2004).
Powers, D.C. & Belshe, R.B. Effect of age on cytotoxic T lymphocyte memory as well as serum and local antibody responses elicited by inactivated influenza virus vaccine. J. Infect. Dis. 167, 584–592 (1993).
American Academy of Pediatrics. Tetanus. in Red Book 2003. Report of the Committee on Infectious Diseases 26th edn. (ed. Pickering, L.K.) 611–616 (American Academy of Pediatrics, Elk Grove Village, Illinois, USA, 2003).
Gupta, P.S., Kapoor, R., Goyal, S., Batra, V.K. & Jain, B.K. Intrathecal human tetanus immunoglobulin in early tetanus. Lancet 2, 439–440 (1980).
American Academy of Pediatrics. Diphtheria. in Red Book 2003. Report of the Committee on Infectious Diseases 26th edn. (ed. Pickering, L.K.) 263–266 (American Academy of Pediatrics, Elk Grove Village, Illinois, USA, 2003).
Morris, D. & McDonald, J.C. Failure of hyper-immune globulin to prevent whooping cough. Arch. Dis. Child. 32, 236–239 (1957).
Edwards, K.M. Pertussis: an important target for maternal immunization. Vaccine 21, 3483–3486 (2003).
Siber, G.R. et al. Evaluation of bacterial polysaccharide immune globulin for the treatment or prevention of Haemophilus influenzae type b and pneumococcal disease. J. Infect. Dis. 165 Suppl 1, S129–S133 (1992).
Gershon, A.A. Measles virus (rubeola). in Principles and Practice of Infectious Diseases 4th edn. (eds. Mandel, G.L., Bennett, J.E. & Dolin, R.) 1519–1528 (Churchill Livingstone, New York, 1995).
American Academy of Pediatrics. Measles. in Red Book 2003. Report of the Committee on Infectious Diseases 26th edn. (ed. Pickering, L.K.) 419–429 (American Academy of Pediatrics, Elk Grove Village, Illinois, USA, 2003).
Centers for Disease Control and Prevention. Human rabies prevention—United States, 1999. Recommendations of Advisory Committee (ACIP). MMWR Morbid. Mortal. Wkly. Rep. 48, 1–21 (1999).
Hankins, D.G. & Rosekrans, J.A. Overview, prevention, and treatment of rabies. Mayo Clin. Proc. 79, 671–676 (2004).
Kempe, C.H. et al. The use of vaccinia hyperimmune gamma-globulin in the prophylaxis of smallpox. Bull. World Health Org. 25, 41–48 (1961).
Galmiche, M.C., Goenaga, J., Wittek, R. & Rindisbacher, L. Neutralizing and protective antibodies directed against vaccinia virus envelope antigens. Virology 254, 71–80 (1999).
American Academy of Pediatrics. Hepatitis A. in Red Book 2003. Report of the Committee on Infectious Diseases 26th edn. (ed. Pickering, L.K.) 309–318 (American Academy of Pediatrics, Elk Grove Village, Illinois, USA, 2003).
Centers for Disease Control and Prevention. Postexposure prophylaxis of hepatitis B. MMWR Morbid. Mortal. Wkly. Rep. 33, 398–402 (1984).
Terrault, N.A. et al. Prophylaxis in liver transplant recipients using a fixed dosing schedule of hepatitis B immunoglobulin. Hepatology 24, 1327–1333 (1996).
Storch, G.A. Humanized monoclonal antibody for prevention of respiratory syncytial virus infection. Pediatrics 102, 648–651 (1998).
Givner, L.B. Monoclonal antibodies against respiratory syncytial virus. Pediatr. Infect. Dis. J. 18, 541–542 (1999).
Fisher, R.G. & Edwards, K.M. Varicella-zoster. Pediatr. Rev. 19, 62–67 (1998).
Acknowledgements
The authors wish to thank C. Brighouse for her editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Margaret A. Liu is Vice Chairman, Transgene, Strasbourg (France). This company is involved in immunotherapy.
Rights and permissions
About this article
Cite this article
Lambert, PH., Liu, M. & Siegrist, CA. Can successful vaccines teach us how to induce efficient protective immune responses?. Nat Med 11 (Suppl 4), S54–S62 (2005). https://doi.org/10.1038/nm1216
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm1216
This article is cited by
-
Cell-traversal protein for ookinetes and sporozoites (CelTOS) formulated with potent TLR adjuvants induces high-affinity antibodies that inhibit Plasmodium falciparum infection in Anopheles stephensi
Malaria Journal (2019)
-
Enhanced germinal center reaction by targeting vaccine antigen to major histocompatibility complex class II molecules
npj Vaccines (2019)
-
Tick-borne encephalitis virus induces chemokine RANTES expression via activation of IRF-3 pathway
Journal of Neuroinflammation (2016)
-
Combined meningococcal serogroup A and W135 outer-membrane vesicles activate cell-mediated immunity and long-term memory responses against non-covalent capsular polysaccharide A
Immunologic Research (2014)
-
Measurement of the plasma levels of antibodies against the polymorphic vaccine candidate apical membrane antigen 1 in a malaria-exposed population
BMC Infectious Diseases (2012)