Abstract
Objective:
This study aims to determine whether fetal meconium passage is associated with autism.
Study Design:
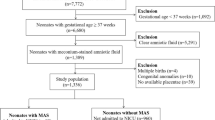
This retrospective birth cohort analysis of 9 945 896 children born in California 1991 to 2008 linked discharge diagnosis and procedure codes for prenatal stressors, meconium-stained amniotic fluid (MSAF) and meconium aspiration syndrome (MAS) with autism diagnoses for 47 277 children through 2012. We assessed the relative risk of autism by meconium status using logistic regression, adjusting for demographic and clinical features.
Results:
Children exposed to meconium (MSAF and MAS) were more likely to be diagnosed with autism in comparison with unexposed children (0.60% and 0.52%, vs 0.47%, respectively). In adjusted analyses, there was a small increase in autism risk associated with MSAF exposure (adjusted relative risk (aRR) 1.18, 95% confidence interval (CI) 1.12 to 1.25), and a marginal association that failed to achieve significance between MAS and autism (aRR 1.08, 95% CI 0.98 to 1.20).
Conclusion:
Resuscitation of neonates with respiratory compromise from in utero meconium exposure may mitigate long-term neurodevelopmental damage.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Fombonne E . Epidemiology of pervasive developmental disorders. Pediatr Res 2009; 65 (6): 591–598.
McCarthy M . Autism diagnoses in the US rise by 30%, CDC reports. BMJ 2014; 348: g2520.
Chaste P, Leboyer M . Autism risk factors: genes, environment, and gene-environment interactions. Dialogues Clin Neurosci 2012; 14 (3): 281–292.
Pinto-Martin JA, Levy SE, Feldman JF, Lorenz JM, Paneth N, Whitaker AH . Prevalence of autism spectrum disorder in adolescents born weighing <2000 grams. Pediatrics 2011; 128 (5): 883–891.
Moore GS, Kneitel AW, Walker CK, Gilbert WM, Xing G . Autism risk in small- and large-for-gestational-age infants. Am J Obstetr Gynecol 2012; 206 (4): 314 e1–314 e9.
Suren P, Roth C, Bresnahan M, Haugen M, Hornig M, Hirtz D et al. Association between maternal use of folic acid supplements and risk of autism spectrum disorders in children. JAMA 2013; 309 (6): 570–577.
Schmidt RJ, Hansen RL, Hartiala J, Allayee H, Schmidt LC, Tancredi DJ et al. Prenatal vitamins, one-carbon metabolism gene variants, and risk for autism. Epidemiology 2011; 22 (4): 476–485.
Harrington RA, Lee LC, Crum RM, Zimmerman AW, Hertz-Picciotto I . Prenatal SSRI use and offspring with autism spectrum disorder or developmental delay. Pediatrics 2014; 133 (5): e1241–e1248.
Croen LA, Connors SL, Matevia M, Qian Y, Newschaffer C, Zimmerman AW . Prenatal exposure to beta2-adrenergic receptor agonists and risk of autism spectrum disorders. J Neurodev Disord 2011; 3 (4): 307–315.
Christensen J, Gronborg TK, Sorensen MJ, Schendel D, Parner ET, Pedersen LH et al. Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA 2013; 309 (16): 1696–1703.
Atladottir HO, Henriksen TB, Schendel DE, Parner ET . Autism after infection, febrile episodes, and antibiotic use during pregnancy: an exploratory study. Pediatrics 2012; 130 (6): e1447–e1454.
Libbey JE, Sweeten TL, McMahon WM, Fujinami RS . Autistic disorder and viral infections. J Neurovirol 2005; 11 (1): 1–10.
Walker CK, Krakowiak P, Baker A, Hansen RL, Ozonoff S, Hertz-Picciotto I . Preeclampsia, placental insufficiency, and autism spectrum disorder or developmental delay. JAMA Pediatr 2015; 169 (2): 154–162.
Krakowiak P, Walker CK, Bremer AA, Baker AS, Ozonoff S, Hansen RL et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics 2012; 129 (5): e1121–e1128.
Burstyn I, Wang X, Yasui Y, Sithole F, Zwaigenbaum L . Autism spectrum disorders and fetal hypoxia in a population-based cohort: accounting for missing exposures via Estimation-Maximization algorithm. BMC Med Res Methodol 2011; 11: 2.
Gardener H, Spiegelman D, Buka SL . Perinatal and neonatal risk factors for autism: a comprehensive meta-analysis. Pediatrics 2011; 128 (2): 344–355.
Monen L, Hasaart TH, Kuppens SM . The aetiology of meconium-stained amniotic fluid: pathologic hypoxia or physiologic foetal ripening? (Review). Early Hum Dev 2014; 90 (7): 325–328.
Fanaroff AA . Meconium aspiration syndrome: historical aspects. J Perinatol 2008; 28 (Suppl 3): S3–S7.
Hutton EK, Thorpe J . Consequences of meconium stained amniotic fluid: what does the evidence tell us? Early Hum Dev 2014; 90 (7): 333–339.
Beligere N, Rao R . Neurodevelopmental outcome of infants with meconium aspiration syndrome: report of a study and literature review. J Perinatol 2008; 28 (Suppl 3): S93–101.
Croen LA, Grether JK, Selvin S . Descriptive epidemiology of autism in a California population: who is at risk? J Autism Dev Disord 2002; 32 (3): 217–224.
Persson M, Johansson S, Villamor E, Cnattingius S . Maternal overweight and obesity and risks of severe birth-asphyxia-related complications in term infants: a population-based cohort study in sweden. PLoS Med 2014; 11 (5): e1001648.
Swarnam K, Soraisham AS, Sivanandan S . Advances in the management of meconium aspiration syndrome. Int J Pediatr 2012; 2012: 359571.
Mundhra R, Agarwal M . Fetal outcome in meconium stained deliveries. J Clin Diagn Res 2013; 7 (12): 2874–2876.
Burstyn I, Sithole F, Zwaigenbaum L . Autism spectrum disorders, maternal characteristics and obstetric complications among singletons born in Alberta, Canada. Chronic Dis Can 2010; 30 (4): 125–134.
Guinchat V, Thorsen P, Laurent C, Cans C, Bodeau N, Cohen D . Pre-, peri- and neonatal risk factors for autism. Acta Obstet gynecol Scand 2012; 91 (3): 287–300.
Bhat R, Vidyasagar D . Delivery room management of meconium-stained infant. Clin Perinatol 2012; 39 (4): 817–831.
Dordevic M, Jovanovic B, Sazdanovic P, Dordevic G . [Neonate—newborn condition and prematurity with breech delivery]. Medicinski pregled 2009; 62 (9-10): 456–460.
Limperopoulos C, Bassan H, Sullivan NR, Soul JS, Robertson RL Jr, Moore M et al. Positive screening for autism in ex-preterm infants: prevalence and risk factors. Pediatrics 2008; 121 (4): 758–765.
Jimenez E, Marin ML, Martin R, Odriozola JM, Olivares M, Xaus J et al. Is meconium from healthy newborns actually sterile? Res Microbiol 2008; 159 (3): 187–193.
Froehlich-Santino W, Londono Tobon A, Cleveland S, Torres A, Phillips J, Cohen B et al. Prenatal and perinatal risk factors in a twin study of autism spectrum disorders. J Psychiatr Res 2014; 54: 100–108.
Gilbert WM, Jacoby BN, Xing G, Danielsen B, Smith LH . Adverse obstetric events are associated with significant risk of cerebral palsy. Am J Obstet Gynecol 2010; 203 (4): 328 e1–5.
Scafidi J, Fagel DM, Ment LR, Vaccarino FM . Modeling premature brain injury and recovery. Int J Neuroscience 2009; 27 (8): 863–871.
Salmaso N, Jablonska B, Scafidi J, Vaccarino FM, Gallo V . Neurobiology of premature brain injury. Nat Neurosci 2014; 17 (3): 341–346.
Salmaso N, Silbereis J, Komitova M, Mitchell P, Chapman K, Ment LR et al. Environmental enrichment increases the GFAP+ stem cell pool and reverses hypoxia-induced cognitive deficits in juvenile mice. J Neurosci 2012; 32 (26): 8930–8939.
Komitova M, Xenos D, Salmaso N, Tran KM, Brand T, Schwartz ML et al. Hypoxia-induced developmental delays of inhibitory interneurons are reversed by environmental enrichment in the postnatal mouse forebrain. J Neurosci 2013; 33 (33): 13375–13387.
Rennie JM, Hagmann CF, Robertson NJ . Outcome after intrapartum hypoxic ischaemia at term. Semin Fetal Neonatal Med 2007; 12 (5): 398–407.
Maximo JO, Cadena EJ, Kana RK . The implications of brain connectivity in the neuropsychology of autism. Neuropsychol Rev 2014; 24 (1): 16–31.
Duran R, Aladag N, Vatansever U, Sut N, Acunas B . The impact of Neonatal Resuscitation Program courses on mortality and morbidity of newborn infants with perinatal asphyxia. Brain Dev 2008; 30 (1): 43–46.
Acknowledgements
This publication was made possible by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development Grant #1R03HD074911-01, and a Medical Student Research Fellowship grant from the University of California, Davis School of Medicine (KM). The funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and the decision to submit the manuscript for publication. The contents of this publication are solely the responsibility of the grantees and do not necessarily represent the official views of the funding agencies. Furthermore, the funders do not endorse the purchase of any commercial products mentioned in the publication. The UC Davis School of Medicine’s Medical Student Research Fellowship provided structure, motivation and support for Ms Miller’s work in the development of this project and the writing of the manuscript. We thank the California’s Department of Public Health, Department of Developmental Services, Office of Statewide Planning and Health Development and Vital Statistics for access to data for this project. This project would not have been possible without the expertize of Beate Danielsen, PhD (Health Information Solutions) who merged these data sets. Findings from this work were presented in poster format at the International Meeting for Autism Research, May 2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Walker serves on the Speaker’s Bureau for Merck & Co. This work pertains neither to pregnancy complications nor to neurodevelopment.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Miller, K., Xing, G. & Walker, C. Meconium exposure and autism risk. J Perinatol 37, 203–207 (2017). https://doi.org/10.1038/jp.2016.200
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.200
This article is cited by
-
Maternal excessive gestational weight gain as a risk factor for autism spectrum disorder in offspring: a systematic review
BMC Pregnancy and Childbirth (2020)