Abstract
Objective:
Determine the association of prenatal and neonatal infections with neurodevelopmental outcomes in very preterm infants.
Study Design:
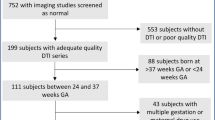
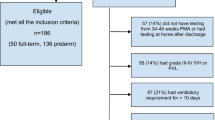
Secondary retrospective analysis of 155 very preterm infants at a single tertiary referral center. General linear or logistic regression models were used to evaluate the association with hospital factors; brain injury, growth and development; and neurobehavioral outcome.
Result:
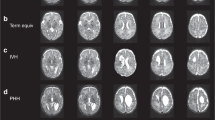
Necrotizing enterocolitis with sepsis was associated with reduced transcerebellar diameter (38.3 vs 48.4 mm, P<0.001) and increased left ventricular diameter (12.0 vs 8.0 mm, P=0.005). Sepsis alone was associated with higher diffusivity in the left frontal lobe (1.85 vs 1.68 × 10−3 mm2 s−1, P=0.001) and right cingulum bundle (1.52 vs 1.45 × 10−3 mm2 s−1, P=0.002). Neurobehavioral outcomes were worse in children exposed to maternal genitourinary infection (cognitive composite: β=−8.8, P=0.001; receptive language score: β=−2.7, P<0.001; language composite: β=−14.9, P<0.001) or histological chorioamnionitis (language composite: β=−8.6, P=0.006), but not neonatal infection.
Conclusion:
Neonatal infection was associated with changes in brain structure but not with neurobehavioral outcomes, whereas the opposite pattern was observed for maternal genitourinary tract infection. These findings emphasize the potential importance of infections during pregnancy on the neurodevelopmental outcomes of preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Marlow N, Wolke D, Bracewell MA, Samara M . Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med 2005; 352 (1): 9–19.
Williams J, Lee KJ, Anderson PJ . Prevalence of motor-skill impairment in preterm children who do not develop cerebral palsy: a systematic review. Dev Med Child Neurol 2010; 52 (3): 232–237.
Barre N, Morgan A, Doyle LW, Anderson PJ . Language abilities in children who were very preterm and/or very low birth weight: a meta-analysis. J Pediatr 2011; 158 (5): 766–774. e1.
Saavalainen P, Luoma L, Bowler D, Maatta S, Kiviniemi V, Laukkanen E et al. Spatial span in very prematurely born adolescents. Dev Neuropsychol 2007; 32 (3): 769–785.
Anderson P, Doyle LW . Neurobehavioral outcomes of school-age children born extremely low birth weight or very preterm in the 1990s. JAMA 2003; 289 (24): 3264–3272.
Anderson PJ, De Luca CR, Hutchinson E, Spencer-Smith MM, Roberts G, Doyle LW . Attention problems in a representative sample of extremely preterm/extremely low birth weight children. Dev Neuropsychol 2011; 36 (1): 57–73.
Mulder H, Pitchford NJ, Hagger MS, Marlow N . Development of executive function and attention in preterm children: a systematic review. Dev Neuropsychol 2009; 34 (4): 393–421.
Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004; 292 (19): 2357–2365.
Neufeld MD, Frigon C, Graham AS, Mueller BA . Maternal infection and risk of cerebral palsy in term and preterm infants. J Perinatol 2005; 25 (2): 108–113.
Mann JR, McDermott S . Are maternal genitourinary infection and pre-eclampsia associated with ADHD in school-aged children? J Atten Disord 2011; 15 (8): 667–673.
Kaindl AM, Favrais G, Gressens P . Molecular mechanisms involved in injury to the preterm brain. J Child Neurol 2009; 24 (9): 1112–1118.
Volpe JJ, Kinney HC, Jensen FE, Rosenberg PA . The developing oligodendrocyte: key cellular target in brain injury in the premature infant. Int J Dev Neurosci 2011; 29 (4): 423–440.
Shatrov JG, Birch SC, Lam LT, Quinlivan JA, McIntyre S, Mendz GL . Chorioamnionitis and cerebral palsy: a meta-analysis. Obstet Gynecol 2010; 116 (2 Pt 1): 387–392.
Dammann O, Kuban KC, Leviton A . Perinatal infection, fetal inflammatory response, white matter damage, and cognitive limitations in children born preterm. Ment Retard Dev Disabil Res Rev 2002; 8 (1): 46–50.
Adams E, Chau V, Poskitt KJ, Grunau RE, Synnes A, Miller SP . Tractography-based quantitation of corticospinal tract development in premature newborns. J Pediatr 2010; 156 (6): 882–888 888.e1.
Glass HC, Bonifacio SL, Chau V, Glidden D, Poskitt K, Barkovich AJ et al. Recurrent postnatal infections are associated with progressive white matter injury in premature infants. Pediatrics 2008; 122 (2): 299–305.
Chau V, Poskitt KJ, McFadden DE, Bowen-Roberts T, Synnes A, Brant R et al. Effect of chorioamnionitis on brain development and injury in premature newborns. Ann Neurol 2009; 66 (2): 155–164.
Hendson L, Russell L, Robertson CM, Liang Y, Chen Y, Abdalla A et al. Neonatal and neurodevelopmental outcomes of very low birth weight infants with histologic chorioamnionitis. J Pediatr 2011; 158 (3): 397–402.
Rovira N, Alarcon A, Iriondo M, Ibanez M, Poo P, Cusi V et al. Impact of histological chorioamnionitis, funisitis and clinical chorioamnionitis on neurodevelopmental outcome of preterm infants. Early Hum Dev 2011; 87 (4): 253–257.
Stoll B, Hansen N, Adams-Chapman I, Fanaroff A, Hintz S, Vohr B et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004; 292 (19): 2357–2422.
Redline RW, Faye-Petersen O, Heller D, Qureshi F, Savell V, Vogler C . Amniotic infection syndrome: nosology and reproducibility of placental reaction patterns. Pediatr Dev Pathol 2003; 6 (5): 435–448.
Smith GC, Gutovich J, Smyser C, Pineda R, Newnham C, Tjoeng TH et al. Neonatal intensive care unit stress is associated with brain development in preterm infants. Ann Neurol 2011; 70 (4): 541–549.
Kidokoro H, Neil J, Inder T . A new MRI assessment tool to define brain abnormalities in very preterm infants at term. AJNR Am J Neuroradiol 2013; 34 (11): 2208–2214.
Nguyen The Tich S, Anderson PJ, Shimony JS, Hunt RW, Doyle LW, Inder TE . A novel quantitative simple brain metric using MR imaging for preterm infants. AJNR Am J Neuroradiol 2009; 30 (1) 125–131.
Carter A, Briggs-Gowan M, Jones SM, Little TD . Infant-Toddler Social and Emotional Assessment (ITSEA): factor structure, reliability, and validity. J Abnorm Child Psych 2003; 31: 495–514.
Spittle AJ, Anderson PJ, Lee KJ, Ferretti C, Eeles A, Orton J et al. Preventive care at home for very preterm infants improves infant and caregiver outcomes at 2 years. Pediatrics 2010; 126 (1): e171–e178.
Helderman JB, O'Shea TM, Kuban KC, Allred EN, Hecht JL, Dammann O et al. Antenatal antecedents of cognitive impairment at 24 months in extremely low gestational age newborns. Pediatrics 2012; 129 (3): 494–502.
Kenyon S, Pike K, Jones DR, Brocklehurst P, Marlow N, Salt A et al. Childhood outcomes after prescription of antibiotics to pregnant women with spontaneous preterm labour: 7-year follow-up of the ORACLE II trial. Lancet 2008; 372 (9646): 1319–1327.
Reiman M, Kujari H, Maunu J, Parkkola R, Rikalainen H, Lapinleimu H et al. Does placental inflammation relate to brain lesions and volume in preterm infants? J Pediatr 2008; 152 (5): 642–647. e1–2.
Chau V, Brant R, Poskitt KJ, Tam EW, Synnes A, Miller SP . Postnatal infection is associated with widespread abnormalities of brain development in premature newborns. Pediatr Res 2012; 71 (3): 274–279.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK . Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 2006; 117 (4): 1253–1261.
Leviton A, Allred EN, Dammann O, Engelke S, Fichorova RN, Hirtz D et al. Systemic inflammation, intraventricular hemorrhage, and white matter injury. J Child Neurol 2012; 28 (12): 1637–1645.
Stout MJ, Conlon B, Landeau M, Lee I, Bower C, Zhao Q et al. Identification of intracellular bacteria in the basal plate of the human placenta in term and preterm gestations. Am J Obstet Gynecol 2013; 208 (3): 226. e221–227.
Woodward LJ, Anderson PJ, Austin NC, Howard K, Inder TE . Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N Engl J Med 2006; 355 (7): 685–694.
Hack M, Taylor HG, Drotar D, Schluchter M, Cartar L, Wilson-Costello D et al. Poor predictive validity of the Bayley Scales of Infant Development for cognitive function of extremely low birth weight children at school age. Pediatrics 2005; 116 (2): 333–341.
Webster RI, Majnemer A, Platt RW, Shevell MI . The predictive value of a preschool diagnosis of developmental language impairment. Neurology 2004; 63 (12): 2327–2331.
Dale PS, Price TS, Bishop DV, Plomin R . Outcomes of early language delay: I. Predicting persistent and transient language difficulties at 3 and 4 years. J Speech Lang Hear Res 2003; 46 (3): 544–560.
Hamrick SE, Miller SP, Leonard C, Glidden DV, Goldstein R, Ramaswamy V et al. Trends in severe brain injury and neurodevelopmental outcome in premature newborn infants: the role of cystic periventricular leukomalacia. J Pediatr 2004; 145 (5): 593–599.
Apisarnthanarak A, Holzmann-Pazgal G, Hamvas A, Olsen MA, Fraser VJ . Ventilator-associated pneumonia in extremely preterm neonates in a neonatal intensive care unit: characteristics, risk factors, and outcomes. Pediatrics 2003; 112 (6 Pt 1): 1283–1289.
Bose CL, Laughon MM, Allred EN, Michael O'Shea T, Van Marter LJ, Ehrenkranz RA et al. Systemic inflammation associated with mechanical ventilation among extremely preterm infants. Cytokine 2013; 61 (1): 315–322.
Acknowledgements
We wish to acknowledge those who assisted in acquiring, processing or reading MRI and US scans at Washington University in St Louis, including Karen Lukas, Joe Ackerman, Tara Smyser, Jeanette Kenley and Eilon Shany (visiting from Soroka University Medical Center, Israel). We are grateful for the advice on statistical processing from Mike Wallendorf and editing from Deborah Frank (both at Washington University in St Louis). This work is financially supported by National Institute of Health (NICHD) R01HD05805, P30HD062171 and the Doris Duke Foundation Distinguished Clinical Scientist Award to Dr Inder. This work was also supported by a grant from the Doris Duke Charitable Foundation to Washington University in St Louis for Clinical Research Fellow IL. Dr Rogers is supported by Grant Number UL1 TR000448 and TL1 TR000449/ KL2 TR000450 from the NIH-National Center for Research Resources (NCRR) and the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health. Dr Symser is supported by the Child Neurology Foundation, NIH K12 NS001690 and UL1 TR000448. Dr Mysorekar is supported by the Preventing Prematurity Initiative grant from the Burroughs Wellcome Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lee, I., Neil, J., Huettner, P. et al. The impact of prenatal and neonatal infection on neurodevelopmental outcomes in very preterm infants. J Perinatol 34, 741–747 (2014). https://doi.org/10.1038/jp.2014.79
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.79
This article is cited by
-
Altered microstructure of the splenium of corpus callosum is associated with neurodevelopmental impairment in preterm infants with necrotizing enterocolitis
Italian Journal of Pediatrics (2022)
-
Human milk feeding and cognitive outcome in preterm infants: the role of infection and NEC reduction
Pediatric Research (2022)
-
Neurocognitive and social-communicative function of children born very preterm at 10 years of age: Associations with microorganisms recovered from the placenta parenchyma
Journal of Perinatology (2020)
-
Experimental necrotizing enterocolitis induces neuroinflammation in the neonatal brain
Journal of Neuroinflammation (2019)
-
Screening for Language Delay between 6 Months and 3 Years of Corrected Age in Very Low Birth Weight Children
Indian Pediatrics (2019)