Abstract
Objective:
Severe intracranial hemorrhage (ICH) is an important prognostic variable in extremely preterm (EPT) infants. We examined imaging and clinical variables that predict outcomes in EPT infants with severe ICH.
Study design:
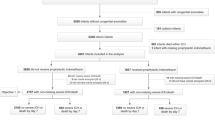
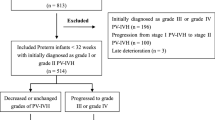
Retrospective analysis of 353 EPT infants with severe ICH. Outcomes were compared by examining: (i) unilateral vs bilateral ICH; and (ii) presence vs absence of hemorrhagic parenchymal infarction (HPI). Regression analyses identified variables associated with death or neurodevelopmental impairment (NDI).
Result:
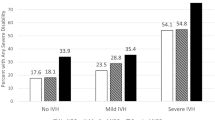
Bilateral ICH and HPI had higher rates of adverse outcomes and were independently associated with death/NDI. HPI was the most important variable for infants of lower birth weight, and bilateral ICH for larger infants. For infants surviving to 36 weeks, shunt placement was most associated with death/NDI.
Conclusion:
Bilateral ICH and the presence of HPI in EPT infants with severe ICH are associated with death/NDI, though the importance depends on birth weight and survival to 36 weeks.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Tyson JE, Parikh NA, Langer J, Green C, Higgins RD . Intensive care for prematurity: moving beyond gestational age. New Engl J Med 2008; 358: 1672–1681.
Richardson DK, Corcoran JD, Escobar GJ, Lee SK for the Canadian NICU Network and The Kaiser Permanente Neonatal Minimum Data Set Wide Area Network and The SNAP-II Study Group. SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr 2001; 138 (1): 92–100.
Meadow W, Frain L, Ren Y, Lee G, Soneji S, Lantos J . Serial assessment of mortality in the neonatal intensive care unit by algorithm and intuition: certainty, uncertainty, and informed consent. Pediatrics 2002; 109 (5): 878–886.
Broitman E, Ambalavanan N, Higgins R, Vohr B, Das A, Bhaskar B et al. Clinical data predict neurodevelopmental outcome better than head ultrasound in extremely low birth weight infants. J Pediatr 2007; 151: 500–505.
Ambalavanan N, Baibergenova A, Carlo WA, Saigal S, Schmidt B, Thorpe KE et al. Early prediction of poor outcome in extremely low birth weight infants by classification tree analysis. J Pediatr 2005; 148: 438–444.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978; 92 (4): 529–534.
Vohr BR, Wright LL, Poole WK, McDonald SA for the NICHD Neonatal Research Network Follow-Up Study. Neurodevelopmental outcomes of extremely low birth weight infants <32 weeks' gestation between 1993 and 1998. Pediatrics 2005; 116: 635–643.
Hintz SR, Kendrick DE, Vohr BR, Poole WK, Higgins RD for the National Institute of Child Health and Human Development Neonatal Research Network. Changes in neurodevelopmental outcomes at 18 to 22 months' corrected age among infants of less than 25 weeks' gestational age born in 1993-1999. Pediatrics 2005; 115: 1645–1651.
Fily A, Pierrat V, Delporte V, Breart G, Truffert P EPIPAGE Nord-Pas-de-Calais Study Group. Factors associated with neurodevelopmental outcome at 2 years after very preterm birth: the population-based Nord-Pas-de-Calais EPIPAGE cohort. Pediatrics 2006; 117 (2): 357–366.
Wood NS, Costeloe K, Gibson AT, Hennessy EM, Marlow N, Wilkinson AR et al. The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following preterm birth. Arch Dis Child Fetal Neonatal Ed 2005; 90 (2): F134–F140.
Hack M, Wilson-Costello D, Friedman H, Taylor GH, Schluchter M, Fanaroff AA . Neurodevelopment and predictors of outcomes of children with birth weights of less than 1000 g: 1992-1995. Arch Pediatr Adolesc Med 2000; 154 (7): 725–731.
O'Shea TM, Allred EN, Kuban KC, Hirtz D, Specter B, Durfee S et al. Intraventricular hemorrhage and developmental outcomes at 24 months of age in extremely preterm infants. J Child Neurol 2012; 27 (1): 22–29.
de Vries LS, van Haastert IC, Benders MJNL, Groenendaal F . Myth: cerebral palsy cannot be predicted by neonatal brain imaging. Semin Fetal Neonatal 2011; 16: 279–287.
Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan MA . United States national reference for fetal growth. Obstet Gynecol 1996; 87 (2): 163–168.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis: therapeutic decisions based on clinical staging. Ann Surg 1978; 187 (1): 1–7.
Walsh MC, Kliedgman RM . Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am 1986; 33 (1): 179–201.
Palisano R, Rosenbaum P, Walter S, Russel D, Wood E, Galuppi B . Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997; 99 (4): 214–223.
Bayley N . Bayley Scales of Infant and Toddler Development. 3rd edn. Psychological Corp: San Antonio, TX, 2006.
Ancel P-Y, Livinec F, Larroque B, Marret S, Arnaud C, Pierrat V et al. Cerebral palsy among very preterm children in relation to gestational age and neonatal ultrasound abnormalities: The EPIPAGE Cohort Study. Pediatrics 2006; 117 (3): 828–835.
Kuban KC, Allred EN, O'Shea TM, Paneth N, Pagano M, Dammann O et al. Cranial ultrasound lesions in the NICU predict cerebral palsy at age 2 years in children born at extremely low gestational age. J Child Neurol 2009; 24 (1): 63–72.
Bassan H, Benson CB, Limperopoulos C, Feldman HA, Ringer SA, Veracruz E et al. Ultrasonographic features and severity scoring of periventricular hemorrhagic infarction in relation to risk factors and outcome. Pediatrics 2006; 117 (6): 2111–2118.
Bassan H, Limperopoulos C, Visconti K, Mayer DL, Feldman HA, Avery L et al. Neurodevelopmental outcome in survivors of periventricular hemorrhagic infarction. Pediatrics 2007; 120 (4): 785–792.
Roze E, Kerstjens JM, Maathuis CGB, ter Horst HJ, Bos AF . Risk factors for adverse outcome in preterm infants with periventricular hemorrhagic infarction. Pediatrics 2008; 122 (1): e46–e52.
Roze E, Van Braeckel KNJA, van der Veere CN, Maathuis CGB, Martijn A, Bos AF . Functional outcomes at school age of preterm infants with periventricular hemorrhagic infarction. Pediatrics 2009; 123 (6): 1493–1500.
Merhar S, Tabangin ME, Meinzen-Derr J, Schibler KR . Grade and laterality of intraventricular haemorrahge to predict 18-22 month neurodevelopmental outcomes in extremely low birthweight infants. Acta Pediatrica 2012; 101: 414–418.
Maitre NL, Marshall DD, Price WA, Slaughter JC, O'Shea TM, Maxfield C et al. Neurodevelopmental outcome of infants with unilateral or bilateral periventricular hemorrhagic infarction. Pediatrics 2009; 124 (6): e1153–e1160.
Hintz SR, Slovis T, Bulas D, Van Meurs KP, Perritt R, Stevenson DK et al. Interobserver reliability and accuracy of cranial ultrasound scanning interpretation in premature infants. J Pediatr 2007; 150 (6): 592–596.
Acknowledgements
We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study. Investigators, in addition to those listed as authors, who participated in this study are listed in the Appendix. The National Institutes of Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development provided grant support for the Neonatal Research Network’s Generic Database Study and Follow-up Study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Davis, A., Hintz, S., Goldstein, R. et al. Outcomes of extremely preterm infants following severe intracranial hemorrhage. J Perinatol 34, 203–208 (2014). https://doi.org/10.1038/jp.2013.162
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2013.162
Keywords
This article is cited by
-
White matter injury in infants with intraventricular haemorrhage: mechanisms and therapies
Nature Reviews Neurology (2021)
-
Erythropoietin Improves Poor Outcomes in Preterm Infants with Intraventricular Hemorrhage
CNS Drugs (2021)
-
Cranial ultrasound findings in preterm germinal matrix haemorrhage, sequelae and outcome
Pediatric Research (2020)
-
Do transport factors increase the risk of severe brain injury in outborn infants <33 weeks gestational age?
Journal of Perinatology (2020)
-
Severe intraventricular hemorrhage and withdrawal of support in preterm infants
Journal of Perinatology (2017)